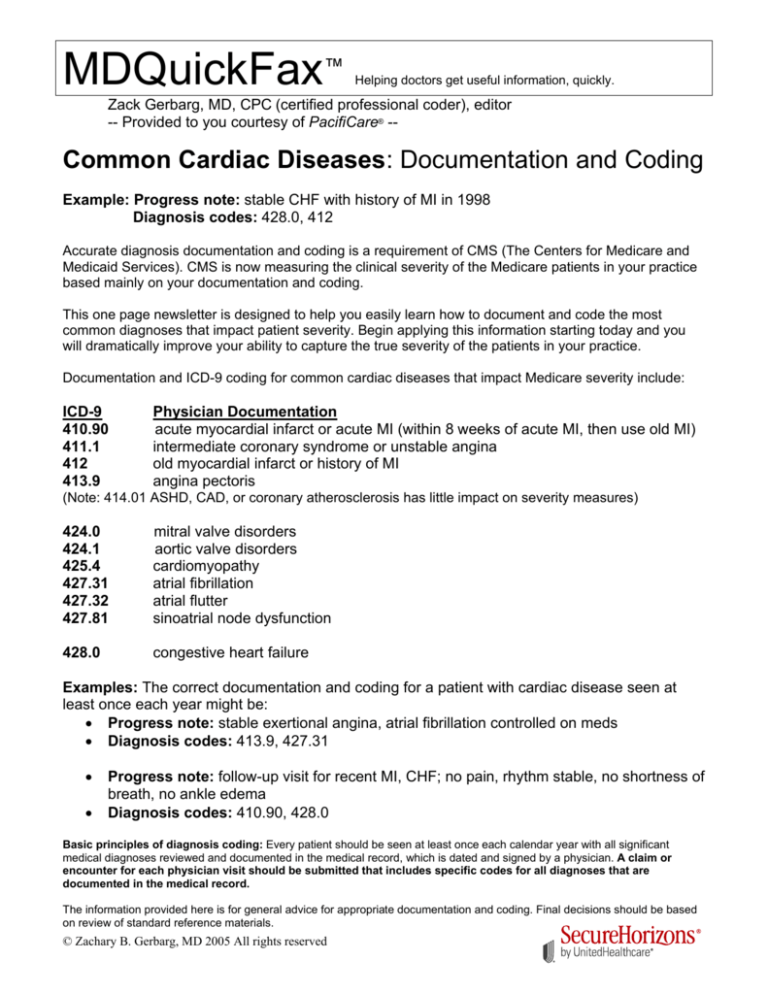
MDQuickFax™
Helping doctors get useful information, quickly.
Zack Gerbarg, MD, CPC (certified professional coder), editor
-- Provided to you courtesy of PacifiCare® --
Common Cardiac Diseases: Documentation and Coding
Example: Progress note: stable CHF with history of MI in 1998
Diagnosis codes: 428.0, 412
Accurate diagnosis documentation and coding is a requirement of CMS (The Centers for Medicare and
Medicaid Services). CMS is now measuring the clinical severity of the Medicare patients in your practice
based mainly on your documentation and coding.
This one page newsletter is designed to help you easily learn how to document and code the most
common diagnoses that impact patient severity. Begin applying this information starting today and you
will dramatically improve your ability to capture the true severity of the patients in your practice.
Documentation and ICD-9 coding for common cardiac diseases that impact Medicare severity include:
ICD-9
410.90
411.1
412
413.9
Physician Documentation
acute myocardial infarct or acute MI (within 8 weeks of acute MI, then use old MI)
intermediate coronary syndrome or unstable angina
old myocardial infarct or history of MI
angina pectoris
424.0
424.1
425.4
427.31
427.32
427.81
mitral valve disorders
aortic valve disorders
cardiomyopathy
atrial fibrillation
atrial flutter
sinoatrial node dysfunction
428.0
congestive heart failure
(Note: 414.01 ASHD, CAD, or coronary atherosclerosis has little impact on severity measures)
Examples: The correct documentation and coding for a patient with cardiac disease seen at
least once each year might be:
• Progress note: stable exertional angina, atrial fibrillation controlled on meds
• Diagnosis codes: 413.9, 427.31
•
•
Progress note: follow-up visit for recent MI, CHF; no pain, rhythm stable, no shortness of
breath, no ankle edema
Diagnosis codes: 410.90, 428.0
Basic principles of diagnosis coding: Every patient should be seen at least once each calendar year with all significant
medical diagnoses reviewed and documented in the medical record, which is dated and signed by a physician. A claim or
encounter for each physician visit should be submitted that includes specific codes for all diagnoses that are
documented in the medical record.
The information provided here is for general advice for appropriate documentation and coding. Final decisions should be based
on review of standard reference materials.
© Zachary B. Gerbarg, MD 2005 All rights reserved