Cross-cultural Communication Skills
advertisement

Albert Einstein College of Medicine
Academic Year 2014-2015
SECTION II. EDUCATIONAL PROGRAM FOR THE M.D. DEGREE
Part A: Key Quantitative Indicators
a. Total number of scheduled weeks of instruction for the complete medical education program. Do
not include weeks devoted to vacation or holiday time.
Source: LCME Part II Medical School Questionnaire
167
b. For U.S. medical schools only:
Provide the USMLE results for first-time takers during the three most recently completed academic
years.
Source: National Board of Medical Examiners School Reports
STEP 1:
Year or
Academic
Year
Number
Examined
Percent
Passing
2011
2012
2013
175
185
187
96
97
97
Year or
Academic
Year
Number
Examined
Percent
Passing
2011-2012
2012-2013
2013-2014*
* Interim data
177
189
153
98
99
99
Mean
Total Score
and S.D.
Score S.D.
227
230
230
20
21
21
National Mean
Total Score
and S.D.
Score S.D.
224
227
228
22
22
21
STEP 2 CK:
Mean
Total Score
and S.D.
Score S.D.
240
19
241
16
241
17
National Mean
Total Score
and S.D.
Score
S.D.
237
21
238
19
239
18
STEP 2 CS:
Year or Academic
Year
2010-2011
2011-2012
2012-2013
Number
Examined
178
170
199
ED-1
Percent
Passing
99
98
99
Albert Einstein College of Medicine
Academic Year 2014-2015
For Canadian medical schools only: Provide the results on Part I of the MCCQE Examination for each
of the three most recently completed academic years.
Source: Dean’s Report, Section II from Medical Council of Canada
Year or
Academic
Year
Number
Examined
Mean Total Exam
Standard Score
and S.D.
Score
S.D.
National Mean
Standard Score
and S.D.
Score
S.D.
c. For U.S. medical schools, show the percentage of graduating medical students in each indicated
academic year who agree or strongly agree (sum of the two categories) with the statement, “Overall, I am
satisfied with the quality of my medical education.”
Source: AAMC GQ (Question 14), the independent student analysis, or other internal survey data.
Percent
Responding
Agree or
Strongly
Agree
2007-08
2008-09
2009-10
2010-11
2011-12
2012-13
2013-14
86.0
90.1
85.8
89.0
84.8
85.0
90.6
d. For Canadian medical schools, show the percentage of graduating medical students in each
academic year who rated the quality of their medical education as good, very good, or excellent using
data from the AAMC Canadian Graduation Questionnaire [CGQ] or other source [please identify].
2007-08
2008-09
2009-10
2010-11
Percent of
students
participating
in the survey
Percent
Responding
Good, Very
Good, or
Excellent
ED-2
2011-12
2012-13
2013-14
Albert Einstein College of Medicine
Academic Year 2014-2015
SECTION II. EDUCATIONAL PROGRAM FOR THE M.D. DEGREE
Part B: Narrative Data and Tables
ED-1. The faculty of an institution that offers a medical education program must define
the objectives of its program. The objectives must serve as guides for establishing
curriculum content and provide the basis for evaluating the effectiveness of the program.
Objectives for the medical education program as a whole serve as statements of what students are expected to learn
or accomplish during the course of the program.
It is expected that the objectives of the medical education program will be formally adopted by the curriculum
governance process and the faculty (as a whole or through its recognized representatives). Among those who should
also exhibit familiarity with these objectives are the dean and the academic leadership of clinical affiliates who share
in the responsibility for delivering the program.
ED-1-A. The objectives of a medical education program must be stated in outcome-based
terms that allow assessment of student progress in developing the competencies that the
profession and the public expect of a physician.
The objectives of the medical education program are statements of the items of knowledge, skills, behaviors, and
attitudes that medical students are expected to exhibit as evidence of their achievement.
The educational objectives, along with their associated outcome measures, should reflect whether and how well
graduates are developing these competencies as a basis for the next stage of their training.
There are several widely recognized definitions of the knowledge, skills, behaviors, and attitudinal attributes
appropriate for a physician, including those described in the AAMC's Medical School Objectives Project, the
general competencies of physicians resulting from the collaborative efforts of the Accreditation Council for
Graduate Medical Education (ACGME) and the American Board of Medical Specialties (ABMS), and the physician
roles summarized in the CanMEDS 2005 report of the Royal College of Physicians and Surgeons of Canada.
__________________________________________________________________________________
The questions below refer to standards ED-1 and ED-1-A.
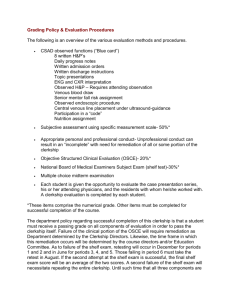
a. Complete the following table showing the general competencies expected of graduates, the
educational program (institutional learning) objectives related to each competency, and the outcome
measure(s) specifically used to assess achievement of each listed objective. Add rows to the table, as
needed.
The table below lists outcome measures used at Einstein to assess our educational program
objectives; these educational program objectives are also referred to as “sub-competencies” later in
the document. The key to the assessment codes used in the competencies can be found in ED
Appendix A. A visual representation of course and clerkship contributions to each competency and
corresponding sub-competencies can be found in ED Appendix B.
ED-3
Albert Einstein College of Medicine
General Competency
HEALER: Students will
demonstrate outstanding
clinical, diagnostic, and
communication skills,
cultural sensitivity, and
empathy, in accordance
with each patient’s needs
and in a partnership with
each patient. Students will
recognize that professional
development in this area
requires becoming
comfortable with
uncertainty and cultivating
humility in light of the vast
breadth of human
experience they will
encounter.
Academic Year 2014-2015
Educational Program Objectives (i.e.
“sub-competencies”)
Demonstrate interview and
physical exam skills appropriate to
the clinical encounter.
Use effective listening skills that
recognize patients’ verbal, nonverbal, and contextual cues.
Use sound clinical judgment in
diagnosing and managing care.
Recognize the individuality of each
patient, including the impact of
culture, faith and spirituality on
patient understanding of health
and disease.
Offer comfort, reassurance, and
hope to patients and families.
Acknowledge a debt of gratitude
toward patients for allowing
students’ experiential involvement
with them to facilitate the
development of future physicians.
ED-4
Outcome Measures
•1st year Introduction to Clinical
Medicine (ICM): student
performance on videotaped
interview competency exercise
with standardized patients,
narrative evaluations, and
performance on quizzes and
written final exam
• 2nd year ICM: student
performance on clinical
competency examination with
standardized patients
•Student performance in all 3rd
year required rotations
(competency-based evaluation
form)
•Student performance on the
Clinical Skills Assessment (CSA)
at end of year 3
• Patients, Doctors &
Communities (PDC): narrative
evaluation used
•Student performance in all 4th
year required rotations
•Student performance on
USMLE Step 2-CS
•OB/Gyn and Surgery Clerkships:
student performance on oral
examination
• OB/Gyn clerkship: student
performance on summative
OSCE
•Pediatrics clerkship: student
performance in PBL sessions
(competency-based evaluation
form)
•Family Medicine Clerkship:
required participation in ECHO
Free Clinic (for the medically
uninsured)
• AAMC Graduation
Questionnaire
• Program directors survey
Albert Einstein College of Medicine
SCIENTIST: Students will
acquire, appraise, and
apply knowledge of
biomedical, clinical,
psychosocial, and
population health sciences
as the foundation for all
their endeavors. Students
will understand the critical
role of basic, clinical, and
translational research in
enhancing the health of
individuals and
populations. By
participating in scholarly
investigation, students will
advance scientific
knowledge and master
principles that can be used
to improve health and
heath care.
Academic Year 2014-2015
Acquire scientific knowledge of the
normal structure and function of
the body and its organ systems,
and the underlying molecular,
biochemical and cellular
mechanisms of homeostasis.
Recognize congenital and acquired
causes of illness, and be familiar
with the altered structure and
function of the body and its
components in various disease
states.
Appreciate the impact of
psychosocial factors, nutrition, and
behavior on health and disease.
Use knowledge of science and the
scientific method to characterize
the quality of evidence, and to
critically evaluate scientific and
medical literature.
Translate and apply scientific and
medical discoveries to improve the
health of individuals and
populations.
Demonstrate scientific research
processes through scholarly
investigation conducted in the
laboratory, clinic, or field to
address well-defined problems or
test specific hypotheses.
ED-5
•Student performance on basic
science course exams
•1st year ICM: student
performance on quizzes and
written exam
•2nd year ICM: student
performance on written final
exam
•Epidemiology, Population
Health, and Evidence-based
Medicine (EPHEM) course (1st
and 2nd year): student
performance in laboratory, case
conferences and final exam
• Student performance on
USMLE Step 1 exam & USMLE
Step 2 CK exams
•Student performance in 3rd year
required rotations (competencybased evaluation form)
•Student performance on NBME
subject exams in all clerkships,
and on institutional exam for
Family Medicine clerkship
•Pediatrics clerkship: student
performance in PBL sessions
(competency-based evaluation
form)
• Pediatrics clerkship: student
performance on required Basic
Science section for mandatory
patient write-ups
•Student performance on CSA at
end of year 3
•Student performance in all 4th
year required rotations
•4th year required Scholarly
Project (SP) ; student
performance assessed by
mentor’s narrative evaluation
•AAMC Graduation
Questionnaire
• Program directors survey
Albert Einstein College of Medicine
ADVOCATE: Students will
become aware of the larger
system of health care, and
embrace their roles as
advocates for patients and
families within the
community, nationally, and
globally. Through skill
development and hands-on
service and leadership
experiences, students will
develop the confidence and
ability to advocate for
improved access to health
care for diverse populations
and for the highest quality
and safest care for all
patients.
Academic Year 2014-2015
Compare major policies
affecting U.S. health care.
Discuss healthcare economics
and financing.
Appreciate the important role
that physicians play in
advocating for improvements
within the U.S. and other health
care systems, including
equitable distribution of
healthcare to diverse
communities.
Demonstrate an ability and
commitment to advocate on
behalf of patients to have their
needs addressed.
Develop skills to ensure patient
safety and high quality care for
all patients.
Serve patients and families in
their own communities, whether
locally, nationally or abroad.
ED-6
•1st year ICM: student
performance written final exam
• Bioethics 1 and 2: student
performance on midterm and
final written exams
• Patients, Doctors, &
Communities (PDC): narrative
evaluation of student
performance
•Student performance in all 3rd
year required rotations
(competency-based evaluation
form)
• Student performance in all 4th
year required rotations
•Family Medicine clerkship:
student performance on
institutional final exam
•Family Medicine clerkship:
student performance on graded
Community Projects
•AAMC Graduation
Questionnaire
• Program directors survey
Albert Einstein College of Medicine
EDUCATOR: Students will
become familiar with
educational principles and
apply these to facilitate
effective learning and
promote well-being among
patients, families, and
communities. Students will
recognize their vital roles as
educators, and dedicate
themselves to teaching the
next generation of
physicians in all areas of
clinical practice, basic
science, and translational
medicine.
Academic Year 2014-2015
Use appropriate communication
skills, terminologies, educational
methods and technologies based
on individual learner needs.
Employ appropriate methods to
educate patients and families,
including techniques to motivate
and reinforce healthy behaviors.
Create conducive learning
environments and encourage selfdirected learning.
Utilize appropriate teaching
techniques for individual, and small
and large group settings.
Select appropriate methods to
evaluate learning by patients,
families, and peers.
Develop professional presentation
skills.
Reflect on the important balance
between respecting patients and
educating students.
ED-7
•1st and 2nd year ICM: student
performance on clinical
competency exams with
standardized patients
• Bioethics 1 and 2: student
performance on midterm and
final written exams
• Patients, Doctors, &
Communities (PDC): narrative
evaluation of student
performance
•Student performance in all 3rd
year required rotations
(competency-based evaluation
form)
•Pediatrics clerkship: student
performance in PBL sessions
(competency-based evaluation
form)
•Family Medicine clerkship:
student performance on graded
Community Projects
•Student performance on
Clinical Skills Assessment (CSA)
at end of year 3
• Student performance in all 4th
year required rotations
•AAMC Graduation
Questionnaire
• Program directors survey
Albert Einstein College of Medicine
COLLEAGUE: Students will
recognize their
responsibility to work
collaboratively as members
of a team in medical,
scientific and educational
communities. Effective
teamwork requires
outstanding oral and
written communication
skills, demonstration of
respect for others’ roles in
an interdisciplinary group,
listening receptively to
diverse viewpoints, and
welcoming feedback to
facilitate personal and
professional growth.
Academic Year 2014-2015
Appreciate the roles and
contributions of the various
members of an interdisciplinary
team.
Demonstrate ability to work
collaboratively in team settings,
and receptivity to diverse
perspectives.
Develop and utilize effective oral
and written communication
skills.
Appreciate the vital importance
of coordination of care as
patients move between clinical
environments, and from medical
settings to home or community.
Consider alternative approaches
to problem solving, and
appreciate the importance of
shared decision-making.
Elicit and integrate feedback
from others as an opportunity to
grow personally and
professionally.
ED-8
• 1st and 2nd year ICM: student
performance in group sessions
(narrative evaluation used)
•1st year ICM: graded case writeups (grading rubric used)
• Anatomy course: peer
feedback exercise
• 2nd year ICM: peer feedback
exercise
• Patients, Doctors, &
Communities (PDC): narrative
evaluation of student
performance
•Required mid-clerkship
feedback sessions in
all required clinical rotations
•Student performance in all 3rd
year required rotations
(competency-based evaluation
form)
•Pediatrics clerkship: student
performance in PBL sessions
(competency-based evaluation
form)
•Clinical Skills Assessment (CSA):
student performance in the
required “Review Program” at
end of year 3
• Student performance in all 4th
year required rotations
• Program directors survey
Albert Einstein College of Medicine
ROLE MODEL: Students will
recognize that they serve as
role models for individual
patients, as well in society
at large. This recognition
necessitates that students
act in accordance with the
highest levels of ethics and
professionalism in all
realms, including clinical
care, research endeavors,
and general behavior as a
member of society. Serving
as a role model requires
dedication to one’s
personal development, and
includes ongoing self-care
and self-reflection to
sustain one’s commitment
to core humanistic
principles and to the
service of others.
Academic Year 2014-2015
Behave professionally,
respectfully, and responsibly.
Adhere to highest ethical
principles in all aspects of
patient care, as well as in
research and educational
activities.
Demonstrate accountability to
patients, society, and the
profession.
Show sensitivity to a diverse
patient population, including
diversity in gender, age, culture,
race, religion, disabilities, and
sexual orientation.
Learn and regularly practice
self-reflection to promote
personal growth and
development.
While maintaining the primacy
of the patient, recognize that
self-care and wellness are
mandatory in order to best serve
others.
ED-9
•ICM: student performance on
written narratives reflecting on
their clinical experiences (graded
using a reflection rubric)
•ICM: Student performance on
self-assessment of videotaped
encounter with standardized
patients (self-assessments are
evaluated by faculty)
•Patients, Doctors, &
Communities (PDC): student
performance on reflective
writing exercises
•Mid-clerkship feedback session
in all 3rd and 4th year required
clinical rotations includes faculty
review of student selfassessment
•Student performance in 3rd year
required rotations (competencybased evaluation form)
•Pediatrics clerkship: student
performance in PBL sessions
(competency-based evaluation
form)
• Student performance in all 4th
year required rotations
• Program directors survey
Albert Einstein College of Medicine
LIFE-LONG LEARNER:
Students will recognize that
learning is a life-long
endeavor. Not only does
scientific knowledge
continually advance, but
the methodologies,
modalities and
technologies available to
learners are ever changing.
Students must learn to
critically assess new
research and clinical
innovations, and apply
evidence-based
recommendations.
Effective life-long learning
requires that students
engage in ongoing selfassessment and receive
comprehensive feedback
from external sources to
identify personal
knowledge gaps and to
maintain enduring
commitment to best
practices.
Academic Year 2014-2015
Learn to review and critically
appraise medical literature.
Apply evidence-based practice, and
follow best practice guidelines
when appropriate.
Demonstrate ongoing selfassessment of personal knowledge
and correction of deficiencies.
Use feedback from external sources
to further identify personal
knowledge gaps and learning
needs.
Develop and maintain skills needed
to utilize information resources and
evolving technologies.
Integrate newly acquired
knowledge and technologies into
clinical and research
environments.
ED-10
•ICM: Student performance on
self-assessment of videotaped
encounter with standardized
patients (self-assessments are
evaluated by faculty)
• 1st and 2nd year EPHEM course:
student performance on written
final exam
• Patients, Doctors, &
Communities (PDC): narrative
evaluation of student
performance
•Student performance in all 3rd
year required rotations
(competency-based evaluation
form)
•Mid-clerkship feedback session
in all 3rd and 4th year required
clinical rotations includes faculty
review of student selfassessment
•Pediatrics clerkship: student
performance in PBL sessions
(competency-based evaluation
form)
•Clinical Skills Assessment (CSA):
student performance in the
required “Review Program” at
end of year 3
• Student performance in all 4th
year required rotations
•4th year required Scholarly
Paper (SP); student performance
assessed by mentor’s narrative
evaluation and formal review by
Office of Medical Student
Research
• Program directors survey
Albert Einstein College of Medicine
Academic Year 2014-2015
b. Describe the medical school’s use of these outcome measures in reaching a summative judgment
regarding students’ attainment of each competency.
Background: As will be described later in section d., Einstein has recently shifted to a competencybased education model, and students are now being assessed throughout their preclinical and
clinical years regarding their attainment of these competencies.
While all competency objectives are covered in the curriculum as a whole, individual course and
clerkship contributions to the seven competency domains vary (see ED Appendices A and B). The
outcome measures allow us to reach a summative judgment regarding students’ attainment of the
appropriate competencies for each course and clerkship, and will allow us to track students’
attainment of each competency across the continuum of their education.
Preclinical years:
1) All preclinical course objectives have been formally linked to individual competencies and their
sub-competency areas. For these courses, faculty leaders are also piloting new software (ExamSoft;
http://learn.examsoft.com/), which will enable them to link exam questions to specific competency
areas and to facilitate a more formal assessment of students’ attainment of each competency.
2) Course objectives for the required Introduction to Clinical Medicine course have been mapped
to the competencies and sub-competencies; the course uses a narrative-based evaluation to assess
students in these areas.
Clinical years:
1) All third- and fourth-year clerkship objectives have been formally linked to the new
competencies and their sub-competency areas. As of June 2013, all students in the required core
clerkships are assessed via our new competency-based Evaluation of Clinical Performance and
Professional Behaviors form (ED Appendix C). Using this form, evaluators and students can easily
visualize how the skills that are being tested relate to specific competency domains. In addition,
problem-based learning evaluation forms for use by clerkship faculty facilitators have been
redesigned, and students’ performance in these small group sessions can now be assessed using a
competency-based framework.
2) The evaluation instrument for the Clinical Skills Assessment, a performance-based evaluation
required of all third year students, has been mapped to the competencies, and students’
performance in this exercise will be evaluated using a competency-based assessment.
In summary, while our competencies are new this academic year, we are already intensively
utilizing outcome measures to reach a summative judgment regarding students’ attainment of each
competency in both the pre-clinical and clinical years. Individual course and clerkship leaders are
already able to give specific competency-based feedback to each student; in addition, we look
forward to the next stage in this process, which will allow us to use data from longitudinal
assessments to track an individual student’s progress through each of these competencies over the
course of his or her medical education. In this way, students can receive highly specific guidance on
strengths and weaknesses, and those with academic difficulty may benefit from targeted feedback
and remediation in discrete competency areas.
c. Indicate the year in which current educational program (institutional learning) objectives were
originally adopted and the year in which they were most recently reviewed or revised.
ED-11
Albert Einstein College of Medicine
Academic Year 2014-2015
Year Adopted
2012
Year Last
Reviewed or
Revised
2012
d. Briefly describe how and by what individuals/groups the educational program objectives are
used in curriculum planning and in the initial selection and ongoing review of the content
included in the curriculum. Note especially whether the objectives of the individual courses and
clerkships have been linked to the educational program objectives and provide examples of how
this linkage is used to determine if appropriate content is being covered in the curriculum.
Einstein had originally developed institutional objectives in 1997, which were refined in 2006. As
noted above, we recently completed an intensive institution-wide process that enabled us to shift to
a competency-based education model. The process began in the summer of 2011 with the
announcement that Dean Allen M. Spiegel had appointed a time-limited Educational Competency
Task Force to draft a set of competencies for Einstein's medical education program. The task force
was chaired by Dr. Julia Arnsten, Chief of the Division of General Internal Medicine. Members
were chosen based on their experience in the areas of educational design, methods, and
measurement, and/or for their expertise in areas that were deemed critical for preparing students
for the future practice of medicine (e.g., patient safety, health economics, technology, etc.). Task
force members represented multiple basic science and clinical departments and affiliate
institutions.
The task force met biweekly starting on September 13, 2011 and over the course of the first three
meetings discussed a detailed list of potential future competencies, compared them with the
ACGME competencies, and reviewed competency models from other institutions. The task force
ultimately decided not to use the ACGME competencies for Einstein, but to develop competencies
that were more clearly consonant with the educational goals and mission of the school. The model
that was selected included seven competency areas, as noted in the chart in Section a. above. In
December 2011, a draft of the competencies and sub-competencies was approved by the Task
Force. Over the next few months, the competency document was presented to the educational
leadership of the medical school for comments and revisions. Presentations were made to key
committees of the Medical Education Council (Executive Committee, Course Directors and Clinical
Directors Sub-committees), the Office of Medical Education's Educational Deans and Directors
Committee, and the dean’s bimonthly meeting with the department chairs and his monthly meeting
with his staff. The final competencies were approved by the Executive Committee of the Medical
Education Council on October 22, 2012.
The annual Davidoff Education Day, held on January 25, 2013, served as the venue for introducing
the competencies and as a forum in which course and clerkship faculty would work together to map
their objectives to the new competency framework. The day began with a nationally renowned
speaker, Dr. Eric Holmboe, discussing the importance of the competencies and competency-based
assessment in medical education, followed by a presentation of the local process that went into
developing our competencies. In preparation for the day, we held the first screening of the new
Educational Competencies video; the 15-minute video featured a wide range of faculty members
and medical students speaking about what each of these seven competencies meant to them as a
way to inspire us as an institution to move forward together in this new direction. During the
afternoon session, course and clerkship faculty worked together to map their current objectives to
the new competencies and their sub-competency areas. Faculty were supervised and guided in this
ED-12
Albert Einstein College of Medicine
Academic Year 2014-2015
process by the senior associate dean for medical education and a specialist in curriculum
development. The goals were to measure how well we were already covering the new competencies,
gain insight into any gaps in the curriculum, and work together to brainstorm future educational
innovations. This exercise revealed that the Einstein medical education curriculum as a whole was
well matched to our new competencies and sub-competency areas, without any significant gaps.
Any future educational modifications will serve to enrich the curriculum, rather than replace
missing elements of our competency-based education. Additional mapping is being done to further
define our educational program and the tools we use to assess student performance. Along these
lines, the Clinical Skills Assessment at the end of year 3 has recently been mapped to the
competencies, allowing for further competency-based assessment of our students. Finally, as new
curricular themes are being developed, mapping to the Einstein Educational Competencies is an
integral part of the process. The task force on Population Health and the Practice of Medicine
started this process in the fall of 2013.
e. Briefly describe how the educational program objectives are used in the evaluation of the effectiveness
of the educational program as a whole.
Each course and clerkship has learning objectives, which are directly linked to our Einstein
competencies and sub-competencies. Each course and clerkship learning objective is also linked to
one or more assessment methods. We use aggregate data of student performance on these
assessments to evaluate our program outcomes. These assessments include class performance on
NBME SHELF exams, institutionally developed exams, USMLE, clinical evaluations, oral
examinations, OSCEs, the Clinical Skills Assessment (CSA), student logs reports, among others. A
low class performance on aggregate data is treated as a gap in the curriculum that will need to be
addressed by the appropriate committee of the Medical Education Council.
In addition, AAMC GQ data are reviewed annually by the Executive Committee of the MEC and
by the Course Directors Sub-committee, Clinical Directors Sub-committee, and the Evaluation Subcommittee. We also survey our graduates’ residency program directors as a way to receive
feedback on the effectiveness of our educational program as a whole. As we begin to survey our
graduates who have been educated in our new framework, we will restructure these surveys to
allow us to evaluate the effectiveness of our new competency-based education program.
Also see information for standards ED-33, ED-35, and ED-46 in this section of the database.
ED-13
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-2. An institution that offers a medical education program must have in place a system
with central oversight to ensure that the faculty define the types of patients and clinical
conditions that medical students must encounter, the appropriate clinical setting for the
educational experiences, and the expected level of medical student responsibility. The
faculty must monitor medical student experiences and modify them as necessary to ensure
that the objectives of the medical education program are met.
The institution that offers a medical education program is required to establish a system to specify the types of
patients or clinical conditions that medical students must encounter and to monitor and verify the medical students'
experiences with patients so as to remedy any identified gaps. The system must ensure that all medical students have
the required experiences. For example, if a medical student does not encounter patients with a particular clinical
condition (e.g., because it is seasonal), the medical student should be able to remedy the gap by a simulated
experience (e.g., a standardized patient experience, an online or paper case) or in another clerkship rotation.
When clerkship rotations in a given discipline are provided at multiple instructional sites, compliance with this
standard (ED-2) may be linked to compliance with standard ED-8, which requires that the medical education
program demonstrate comparability of education experiences across instructional sites.
____________________________________________________________________________________
a. Describe the mechanisms used for the initial selection and subsequent revision of the kinds of patients
or clinical conditions, along with the clinical setting(s) for each, needed to meet the medical school’s
objectives for clinical education. Note if the kinds of patients or clinical conditions were selected by each
clinical discipline or by a group (e.g., a clinical clerkship committee) with representation from multiple
disciplines. Briefly summarize the role of the curriculum committee or other central oversight body (e.g.,
a clerkship rotation directors committee) in reviewing the criteria across courses and clerkships (or in
Canada, clerkship rotations).
Students must log their clinical experiences on all required third- and fourth-year clerkships and
sub-internships. In 2012, Einstein reviewed and revised the existing process in two phases. The first
phase concentrated on standardizing the working nomenclature and format used in electronic
logging; the second phase focused on establishing a new requisite set of conditions and procedures
across all required third- and fourth-year clerkships and sub-internships, and updating existing
logging policies.
In April 2012, a working group of the Clinical Directors Sub-committee comprising clerkship
directors presented their recommendations, which were approved by the Sub-committee effective
for the 2012-13 academic year. Several policies on uniform nomenclature and log format were
adopted. Required rotations must collect patient age and gender demographics but must not collect
specific patient identifiers, in compliance with HIPAA regulations; the clinical setting is defined as
“inpatient” or “outpatient”; clinical location is defined as our hospital affiliate sites, community
health clinics and private practices; and clinical service is defined as a unit within a clinical site
(e.g., hospital floor, consultation service, emergency department) when appropriate. All required
clerkships and sub-internships must set the minimum number of patient encounters in order for
students to pass each rotation. Students must submit the name of supervising attendings (and
residents when applicable) for each encounter logged.
Clinical conditions and procedures are to be logged by students in all required clerkships and
rotations. Clinical conditions are defined as diagnosis, symptoms or conditions, while “procedures”
are defined as procedures, skills and counseling. The level of student responsibility for all “clinical
conditions” is set as “participated.” Participated is defined as: “The student must be actively
involved in seeing the patient with appropriate supervision, either from the initial presentation
ED-14
Albert Einstein College of Medicine
Academic Year 2014-2015
and/or during the discussion of the diagnosis and management of the patient’s condition. The
student should be actively engaged in eliciting or discussing the patient’s complaints and history,
the physical diagnosis and the results of supporting labs and imaging studies. The student should
have the opportunity to ask questions.”
The level of student responsibility for “procedures” is set at “performed” (e.g., breast exam,
venipuncture) and/or “observed” (e.g., Cesarean section), as appropriate to the task and
determined by the clerkship director. Performed is defined as: “The student, under direct
supervision, appropriately executes the required steps of the task. The student received guidance,
support and feedback from the preceptor.” Observed is defined as: “The student is present and
attentively studying the patient encounter in order to learn from the observation (e.g., the process,
the patient experience).”
In December 2012, a working group of the Clinical Directors Sub-committee began meetings to
work on the second phase of this project. The charge was to: 1) revise and formulate a new common
set of “clinical conditions” and “procedures” all students must encounter across every required
third- and fourth-year clerkship; 2) establish a list of alternate experiences for each condition or
procedure should a student not encounter this during direct patient care; and 3) update student log
policies and monitoring systems. This working group had representation from every clerkship/subinternship director, and was chaired by the assistant dean for medical education.
In order to formulate a list of conditions and procedures our students must encounter, the working
group reviewed: population health data from the Centers for Disease Control and the New York
City Department of Health; the list of conditions and procedures to be logged as recommended by
national medical education societies (e.g., Society of General Internal Medicine, etc.); and the
Einstein Educational Competencies, sub-competencies and specific clerkship objectives. Each
clerkship director first submitted a preliminary list of conditions and procedures, and the working
group met monthly to discuss the submissions. The clerkship directors negotiated extensively on
using common nomenclature for conditions and procedures; debated the developmental
appropriateness of other submissions; and worked collaboratively on owning any gaps in conditions
or procedures. The group recommended additions, deletions or clarifications and labored tirelessly
to reduce the initial submission of 535 conditions and procedures down to a feasible yet
educationally appropriate list of 206 conditions and procedures.
In May 2013, a final map of common conditions and procedures all Einstein students must
encounter in required clinical rotations was established and approved by the Clinical Directors’
Subcommittee for use starting in the 2013-14 academic year. This map was called the Einstein 206.
The appropriate level of student responsibility, clinical setting and alternate experiences has been
set for each condition and procedure.
Any changes to the Einstein 206 policies or requisite conditions and procedures must be presented,
reviewed and approved by the Clinical Directors’ Sub-committee. Accordingly, after a recent
review by this sub-committee, this list of conditions and procedures was recently revised; its
current title is the Einstein 203 (ED Appendix D.)
b. Provide a table summarizing the criteria for patient types or clinical conditions, level of student
responsibility, and clinical setting for each required clerkship rotation.
The Einstein 203 manual in ED Appendix D contains the table mapping all the common conditions
and procedures all Einstein students must encounter in specific clinical rotations. This table also
lists the level of student responsibility for each condition and procedure on each required rotation.
ED-15
Albert Einstein College of Medicine
Academic Year 2014-2015
c. Describe the system(s) used by students to log the clinical experiences required of them.
The required clerkship/sub-internship logs are maintained electronically in our online learning
management system (eMED). Students can also access the eMED log system via their personal
mobile smartphones and tablets. The log requires the student to document the date of the
encounter, the patient’s age and gender, the conditions in which they participated; any observed
and/or performed procedures, the clinical setting, and the name of the supervising attending (and
resident as appropriate). A few clerkships may also collect additional data such as clinical service,
clinical location or para/gravida status. Log reports can be generated by students, faculty or
clerkship directors for their mid-cycle review in order to determine progress and gaps within the
clerkship experience. Students can also log approved alternate experiences in the event that they do
not encounter the condition/procedure with an actual patient.
d. Summarize the system(s) used by faculty to monitor students’ completion of required clinical
experiences. When and by whom are clerkship-specific clinical experiences reviewed and monitored?
When and by whom are overall clinical experience data for all students collected and monitored?
All students must review with a specified faculty member (e.g., supervising attending, clinical site
director, or clerkship director/s) the progress of their patient encounter logs during the mandatory
mid-cycle feedback session on all required clinical rotations in the third and fourth year. The
clerkship/sub-internship director is responsible for designating the specific faculty member who
will review the logs with students and for communicating this information to students. The student
and designated faculty member are mutually responsible for arranging the mid-cycle feedback
session. The clerkship director must be contacted immediately if there is any difficulty in arranging
this session. Each student is responsible for providing the report for review by the designated
faculty member during this session. The student and faculty must formulate plans for meeting the
remaining requisite conditions and procedures before the end of the rotation. The student is
responsible for proactively seeking out these experiences. If a student cannot complete the required
conditions or procedures in the clinical setting, he/she must complete an alternative educational
experience, as determined by the clerkship director/s, before the rotation has ended.
For all clerkships with an NBME shelf exam or institutionally developed exam, all log requirements
must be completed prior to the date of the administration of the exam. The exact due date is
determined by each clerkship/sub-internship director(s) and communicated to students. If all log
requirements are not completed by this date, the student will be unable to sit for the clerkship exam
and will receive an Incomplete grade for the clerkship. The student will not be allowed to sit for a
make-up clerkship examination until all log requirements have been satisfied. A student who
completes the log requirements after the end of their clerkship and who passes a clerkship via a
make-up examination may not receive an Honors grade in the clerkship. An exception may be
allowed for maternity or disability-related issues. If after six months counted from the last day of
the rotation in question, the student still does not complete the log requirements and does not sit for
a make-up clerkship examination – the Incomplete grade will revert to a permanent failing grade.
For the clerkships without an NBME shelf exam or institutionally developed exam, the log
requirements must be completed by 11:59 pm of the last Friday of the clerkship. If all log
requirements are not completed, the student will be automatically issued an Incomplete grade for
the clerkship. If after six months counted from the last day of the rotation, the student still does not
complete the log requirements, the Incomplete grade will revert to a permanent failing grade.
ED-16
Albert Einstein College of Medicine
Academic Year 2014-2015
Starting in the 2014-2015 academic year, the Sub-internships in Surgery and Obstetrics will also
follow this policy.
Students who do not complete all log requirements in the third year will postpone the start of their
fourth year. Students planning to take a year off between third and fourth year (for participation in
research, global health programs, etc.), cannot start their year off until all patient logs are
complete. Students who do not complete all log requirements in the fourth year will not receive a
diploma at graduation.
A bi-annual report demonstrating the comparability of educational experiences, across clinical sites
within each required clerkship/sub-internship, is generated by the Office of Educational Resources.
This report is based on cumulative data from the student logs in eMED. Every six months, the
assistant dean for medical education reviews the site comparability reports for all the required
rotations and notes any gaps across sites. A copy of the individual clerkship/sub-internship site
comparability report is provided to each clerkship director for review. The clerkship/subinternship director is responsible for sharing this report with his or her clinical site directors. (See
ED Appendix E for examples of reports.)
e. For each required clinical clerkship/clerkship rotation during the most recently completed academic
year, provide the percent of students who completed each required clinical experience and procedure.
Note the required clinical experiences where more than 20% of students used options/alternative
experiences to meet the requirement. For programs with distributed campuses, provide the data for each
campus.
Describe how the information on completion rates is used by clerkship directors and the curriculum
committee.
During the 2012-2013 academic year, our patient log system did not have the capability to generate
the percentage of students who completed each required clinical experience and procedure. The
table below was created from estimates by each clerkship and sub-internship director.
Required Rotation
Family Medicine
Geriatrics
Medicine
Obstetrics and
Gynecology
Pediatrics
Third-Year Clerkships
Percent of students
Required clinical experiences where more than 20%
completing each required
of students used options/alternative experiences to
clinical experience and
meet the requirement
condition
100%
None
100%
None
100%
None
100%
None
100%
Psychiatry
100%
Radiology
100%
Abuse, child
Altered mental status/lethargy
Gait abnormality/musculoskeletal pain
Eating disorder
Mood disorder due to generalized medical
condition
Child abuse
Ectopic pregnancy
ED-17
Albert Einstein College of Medicine
Surgery
Advanced
Ambulatory
Family Medicine
Ambulatory
Medicine
Ambulatory
Pediatrics
Family Medicine
Sub-internship
Medicine Subinternship
Neurology
Pediatrics Subinternship
Academic Year 2014-2015
Pneumoperitoneum
Radiation safety
Bowel obstruction
100%
i.
Burns
ii.
Trauma
Fourth-Year Clerkships and Required Sub-internships
100%
None
100%
None
100%
None
100%
None
100%
None
100%
100%
Myasthenia gravis
None
During our working group meetings, we designed a new log system in eMED for the 2013-14
academic year that will allow us to generate the percent of students who completed each required
clinical experience and procedure, and any clinical experience where more than 20% of students
used alternate experiences to meet the requisites.
Once a year, the Evaluation Sub-committee reviews student completion rates of educational
experiences for each clerkship and sub-internship. This information will be integrated into the
Evaluation Subcommittee report to each clerkship/sub-internship director. The clerkship/subinternship director responds to the Evaluation Sub-committee report and conducts a brief
presentation to the Clinical Directors’ Subcommittee. As part of the response and presentation, the
clerkship/sub-internship director must address specific strategies for addressing any issues noted.
f. For each required clerkship or clerkship rotation (for Canadian schools), list the options (e.g.,
simulation, assigned readings, CLIPP cases) for remedying gaps in student clinical experiences.
Students who are unable to locate the required conditions or procedures in the clinical setting must
complete an alternative educational experience as determined by the clerkship before the rotation
has ended. Alternative educational experiences approved by the Clinical Directors’ Subcommittee
are the following:
a) Online cases
b) Standardized patients
c) Simulation
d) Case presentations
e) Video cases
f) Readings
g) Problem-based learning sessions
h) Team-based learning sessions
i) Didactics / Conferences
ED-18
Albert Einstein College of Medicine
Academic Year 2014-2015
The specific alternate experiences available to students within each clerkship and sub-internship
are listed in the table below:
Third-Year Clerkships
Alternate experiences
Online cases; readings; didactics/conferences; video cases
Online cases; readings; didactics/conferences; case presentations
Online cases; readings; standardized patients; didactics/conferences
Online cases; simulation; standardized patients;
didactics/conferences; video cases
Pediatrics
Online cases; problem-based learning sessions; reading; standardized
patients; didactics/conferences
Psychiatry
Online cases; case presentations; readings; simulation;
didactics/conferences; video cases
Radiology
Online cases; readings; case presentations; didactics/conferences
Surgery
Online cases; case presentations; readings; simulation;
didactics/conferences; video cases
Fourth-Year Clerkships and Required Sub-internships
Advanced Ambulatory Family
Online cases; readings; didactics/conferences; video cases
Medicine
Ambulatory Medicine
Online cases; case presentations; readings; didactics/conferences;
video cases
Ambulatory Pediatrics
Online cases; case presentations; video cases; readings; didactics /
conferences
Family Medicine Sub-internship Online cases; readings; didactics/conferences; video cases
Medicine Sub-internship
Online cases; readings; standardized patients; didactics/conferences
Neurology
Case presentations; readings; didactics/conferences; video cases
Obstetrics Sub-internship
This sub-internship will be available AY2014-15.
Pediatrics Sub-internship
Case presentations; didactics/conferences; readings
Surgery Sub-internship
This sub-internship will be available AY2014-15.
Required Rotation
Family Medicine
Geriatrics
Medicine
Obstetrics and Gynecology
See also the Required Clerkship Rotation Forms.
ED-19
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-3. The objectives of a medical education program must be made known to all medical
students and to the faculty, residents, and others with direct responsibilities for medical
student education and assessment.
____________________________________________________________________________________
Describe the means by which the general objectives of the educational program (institutional learning
objectives) are made known to each of the following:
(a) Medical students:
After the final competencies were approved, the Einstein Graphic Arts Center designed the
Einstein Educational Competencies logo, which visually represents the seven competency pillars,
including the theme of professionalism that runs through the entire spectrum of the competencies.
In addition, the Office of Medical Education sponsored the production of the Einstein Educational
Competencies video, on which a diverse group of our faculty and medical students speak about what
these new competencies mean to their careers and or their education at Einstein.
The competencies were introduced during the orientations for first- and second-year classes in the
summer of 2013. The third-year students’ initiation occurred during their Introduction to the
Clerkships Day in June 2013; students heard a presentation on the new competencies, were
educated on the new competency-based evaluation form for their required clerkships, and watched
a screening of the Educational Competencies video. Students also received a laminated “competency
card” designed to fit in the pocket of their white coats. During these orientations, students were
additionally directed to the appropriate site on the Einstein website for further viewing of the new
competencies as well as the competency video (See: https://www.einstein.yu.edu/education/mdprogram/curriculum/educational-competencies.aspx). In addition, students can now access these
competencies on eMED, and in the near future will see the competency logo on the face pages for
each course and clerkship. The process of introducing the Educational Competencies will be
repeated annually at the firs-second-, and third-year orientations.
b) Instructional staff, including course and clerkship rotation directors, full-time and volunteer
(community) faculty, graduate students, and resident physicians with responsibility for teaching,
assessing, and supervising medical students:
As detailed in ED 1-A section d., the annual Davidoff Education was the venue used to introduce
the new competencies to course and clerkship leaders and key faculty from across the institution
and all affiliates. The day included a keynote speech from Dr. Eric Holmboe, a national expert on
competency-based medical education, presentations on the development of the Einstein Educational
Competencies, the introduction of the new logo, and the first screening of the Einstein Educational
Competencies video. In addition, the annual Einstein Clerkship Retreat, held on April 10, 2013, was
dedicated to further educating key clinical faculty about the new competencies. The theme of the
Clerkship Retreat was “Assessing Clinical Competency,” and featured a keynote address by Dr.
Kristen Goodell, Director of Innovation in Medical Education at Harvard Medical School. In
addition to her keynote address on the topic, Dr. Goodell also delivered two other presentations on
assessing clinical competency, including “A Competency Toolkit: How to Get Past Direct
Observation,” and “Competency Cares: A Method to Evaluate Students, Standardize Experiences
and Develop Faculty.”
ED-20
Albert Einstein College of Medicine
Academic Year 2014-2015
All Einstein faculty members received a faculty “blast” email on May 31, 2013 announcing the new
competency-based curriculum and directing faculty to Einstein’s website to view the competency
document and watch the video. Course and clerkship directors have received laminated
competency cards and are responsible for further reinforcing the competencies with their
respective faculty. In addition, faculty members who recently joined the Einstein community
attended a New Faculty Orientation on October 15, 2013 where they were introduced to the new
competencies, received a laminated competency card and viewed the Einstein Educational
Competencies video.
Residents and non-faculty teachers learned about the competencies from the clerkship site leaders
and during the Resident-as-Teacher sessions at their respective sites. In addition, every house
officer and non-faculty teacher of medical students received an electronic copy of the competencies,
and was required to verify his or her receipt of the information.
(c) The academic leadership of the medical school and its affiliated institutions
The academic leadership of the College and its affiliated institutions reviewed the competency
document prior to its approval. As noted in ED 1-A, presentations of the competency document
were made to key committees of the Medical Education Council (Executive Committee, Course
Directors Sub-committee and Clinical Directors Sub-committee), the Office of Medical Education's
Educational Deans and Directors Committee, and the dean’s bimonthly meeting with the
departmental chairs and his monthly meeting with his staff. In addition, Dean Allen M. Spiegel and
other academic leaders have viewed the Einstein Educational Competencies video. All faculty
leaders at the school and affiliates received the faculty “blast” email announcement, which included
the links to the competency document and video at: https://www.einstein.yu.edu/education/mdprogram/curriculum/educational-competencies.aspx.
Also see information for standard ED-24.
ED-21
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-4. A medical education program must include at least 130 weeks of instruction.
____________________________________________________________________________________
Report the number of scheduled weeks of instruction in each of the following:
Year/Academic Period One
Year/Academic Period Two
Year/Academic Period Three
Year/Academic Period Four
Total Weeks
42
35
46
44
167
Also see Part A, item (a.) in this section of the database.
ED-5. The curriculum of a medical education program must provide a general
professional education and prepare medical students for entry into graduate medical
education.
___________________________________________________________________________________
a. Supply a schematic or diagram that illustrates the structure of the educational program for the base
academic year (e.g., 2013-2014) used in the database and self-study. The schematic or diagram should
show the approximate sequencing of, and relationships among, required courses and clerkship rotations in
each academic period of the curriculum.
YEAR 1: The first year of the curriculum includes elective mini-courses in Health Disparities,
Nutrition and Health, and Medical Spanish. Spanish language training in the first year is provided
at beginning, intermediate and advanced levels. An elective in medical Mandarin will be offered in
2014-2015.
Medical
Histology and
Cell Structure
Clinical and Developmental Anatomy
Molecular and Cellular Foundations of Medicine
Introduction to Clinical Medicine:
Introduction to the Patient/The Clinical Experience
Cardiovascular The Renal
Physiology
System
Disease
Mechanisms
Principles of
Pharmacology
Epidemiology, Public Health,
& Evidence-Based Medicine 1
Bioethics 1
YEAR 2: In the second year, all students are required to take instruction in Cardiopulmonary
Resuscitation (CPR) with certification by the American Heart Association. Medical Spanish
elective courses continue with offerings at beginning, intermediate and advanced levels.
Interdisciplinary courses integrating physiology, pathobiology, pharmacology, epidemiology
population Health, Evidence-Based Medicine, bioethics, and radiology are required.
ED-22
Albert Einstein College of Medicine
Academic Year 2014-2015
CardioNervous System and Human vascular
Behavior
Medicine
Endocrine
System
Pulmonary
and Critical
Care
Medicine
GastroHematology
intestinal and
Liver
Diseases
Reproductive
System
and Human
Sexuality
Musculoskeletal
Disorders
Microbiology and Infectious Diseases
Bioethics 2
Parasitology & Global
Medicine
Introduction to Clinical Medicine:
The Clinical Examination/Introduction to Clerkships
Epidemiology, Public Health, & Evidence-Based Medicine 2
YEAR 3: In June of the third year, the student begins a sequence of clerkships in internal
medicine, general surgery, pediatrics, psychiatry, obstetrics and gynecology, family medicine,
geriatrics and radiology. During this important phase of medical education, the student becomes
virtually a full-time inhabitant of the various public and private health care affiliates of the
College. The student learns to take responsibility for patient care under supervision and interacts
with attending physicians, residents, nurses, social workers and physician assistants.
Required clinical clerkships
Internal Pediatrics Psychiatry Obstetrics & General Family Radiology Geriatric
Medicine medicine medicine Gynecology Surgery Medicine medicine Medicine
11 weeks
7 weeks
6 weeks
6 weeks
8 weeks 4 weeks
2 weeks
2 weeks
Patients, Doctors and Communities
YEAR 4: During the Ambulatory Care Program, students participate in the evaluation and therapy of adult or
pediatric outpatients. Students in this program are expected to develop a sense of responsibility for continuity
of patient care and appreciation of the special problems that confront the physician of first contact.
Every student is required to do a two-month sub-internship in medicine, pediatrics or adolescent medicine; a
sub-internship is offered for those students interested in a career in family medicine. Beginning in June
2014, each student will be required to complete a one-month sub-internship in one of the core
ED-23
Albert Einstein College of Medicine
Academic Year 2014-2015
primary care fields (medicine, pediatrics or family medicine). A second month of the sub-internship
can be completed in one of the three primary care fields or in general surgery or obstetrics.
Functioning as an integral member of the patient-care team, the sub-intern assumes many of the
responsibilities of a first-year resident under supervision of the resident and attending physician staff.
A one-month clerkship in Neurology completes the four months of required senior year courses.
A major part of the senior year is an elective period of five months duration. Students choose from a
wide selection of electives offered by virtually every department. Through the elective program, a
student may choose to obtain additional sub-internship experience, further training in ambulatory
medicine and primary care, or participate in a research project. Electives in clinical specialties such
as cardiology, infectious disease, endocrinology, dermatology, nephrology, gastroenterology,
pulmonary medicine and emergency medicine are very popular. Also available are programs in
community medicine, drug abuse, alcoholism, and geriatrics. Electives may be arranged at other
medical schools in the US or abroad. Funding is available for students to participate in exchange
programs with overseas medical schools or obtain clinical/research experience in less developed
nations.
Required clinical experiences and electives:
Sub-internship
in Medicine,
Pediatrics or
Family Medicine
(see paragraph
above for
changes in 20142015)
Neurology
Ambulatory Care
Program
in Medicine,
Pediatrics or
Family Medicine
ELECTIVES
7 months of electives available
in blocks of one or two months
1 month
1 month
2 months
If the structure of the curriculum has changed since the base year (i.e., a new curriculum or curriculum
year has been implemented), also include a schematic of the new curriculum, labeled with the year it was
implemented. N/A
b. Provide a separate brief description of any parallel curriculum (“track”), including the sequence of
courses/clerkships. Note the location of the track (main campus or geographically separate/distributed
campus), the year it was first offered, and the general curriculum structure. Highlight the differences
from the regular educational program.
Einstein has a single required curriculum for all medical students.
See the definition of a parallel curriculum in the instructions at the beginning of this section.
Also see Required Courses and Clerkship Rotations (A. Summary Data).
ED-24
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-5-A. A medical education program must include instructional opportunities for active
learning and independent study to foster the skills necessary for lifelong learning.
It is expected that the methods of instruction and assessment used in courses and clerkship rotations will provide
medical students with opportunities to develop lifelong learning skills. These skills include self-assessment on
learning needs; the independent identification, analysis, and synthesis of relevant information; and the appraisal of
the credibility of information sources. Medical students should receive explicit experiences in using these skills, and
they should be assessed and receive feedback on their performance.
___________________________________________________________________________________
Active learning: a type of learning where the student 1) independently, or collaboratively with peers,
identifies learning objectives and seeks the information necessary to meet the objectives and/or 2)
independently identifies, prepares, and discusses information in a way that contributes to group
learning. In active learning, the learner has a role in defining his or her own learning outcomes
and/or those of his or her peers.
a. Provide sample weekly schedules in the Appendix that illustrate the amount of time in the first and
second years (phases) of the curriculum that students spend in scheduled activities.
See ED Appendix F.
b. Provide a list of the types of instructional formats that the medical school characterizes as active
learning.
Einstein uses the standardized terminology and definitions from MedBiquitous to characterize and
categorize our instructional formats. Our institution characterizes the following instructional
methods as active learning:
Mentorship – Students set their own learning goals with discussion and guidance of senior
faculty.
Problem-based learning (PBL) – Use of specially designed cases where students acquire team
participation skills, critical knowledge, problem solving abilities, and self-directed learning
strategies.
Research - Limited or sustained participation in research.
Reflection - Examination by the student of personal cognitive, emotional, and affective
experiences from a learning event.
Self-directed learning – Students take responsibility for their own learning by self-assessing
their needs, formulating goals, identifying resources, implementing appropriate activities, and
evaluating outcomes.
Service learning activity - Students are involved in meaningful community service and reflect
on their service experiences in order to instill a sense of civic responsibility.
Team-based learning (TBL) - A specific method of collaborative learning that follows a specific
sequence of individual work, teamwork and class work with immediate feedback. During the
peer assessment sequence students assess their own performance and those of their peers, and
set individual goals for improvement in interpersonal skills.
c. Describe the time available for students to prepare for active learning.
ED-25
Albert Einstein College of Medicine
Academic Year 2014-2015
Years 1 and 2:
Our academic calendar does not denote specific blocks of time allocated to active learning in the
pre-clinical years; however time for active learning is integrated into the weekly schedule. The
College is sensitive to each student’s individual learning needs and diverse learning styles. On
average, every first- and second-year student has some protected time mid-day or during the
afternoon on most week days for self-directed learning, to prepare for small-group sessions, or to
work on other projects.
Each spring, first-year students are offered additional time blocks for self-directed learning. Based
on their personal interests and educational needs, they may use this protected time to take one of
three available electives: Health Disparities: Awareness to Action; Nutrition and Health: Patients
and Populations; or the Medical Spanish Program. The Medical Spanish Program extends into the
second year. These electives are scheduled from once to four times a week in 1-2 hour blocks.
Completion of these electives is noted in the student’s official transcript.
All medical students are given protected time in the summer between the first and second year to
explore their own educational interests. Students may participate in a variety of research projects;
volunteer their time on service-learning projects in the community; learn a second language
abroad; or participate in global health experiences. Fellowship stipends are provided for students
conducting mentor-guided research at Einstein and for Global Health projects. Notably about 100110 students receive summer research stipends for the summer between years 1 and 2. Travel
grants are provided for presentation of research at national meetings.
Years 3 and 4:
Work hours policies have been established for third- and fourth-year students in clerkships and
required sub-internships. Student work hours across sites within each clerkship/sub-internship
must be comparable and monitored by the clerkship directors. Students’ total weekly work hours
will not exceed 80 hours spent in scheduled clinical and educational activities at clinical sites or the
medical school. Each clerkship determines its own policy regarding distribution of student work
hours (e.g., may include overnight call). Sub-interns, who have primary patient care
responsibilities, may not exceed PGY‐1 work hours as mandated by ACGME policy and NYS 405
regulations.
Clerkship directors are sensitive to allocating protected time for self-directed learning and study.
For example, during the four-week Family Medicine clerkship the directors reduced the number of
one-hour lectures from 12 to 4 in order to give students more time to prepare for each team-based
learning (TBL) session. Additionally in this clerkship, students are also given six half days to work
on their required community service-learning projects, with only one hour of formally structured
activities during each half-day, and the rest of the time open for student-directed preparation.
During the Pediatrics clerkship, students are given protected time to prepare and research their
learning issues, individually and as a group, before and after each problem-based learning session
(PBL).
Medical students have the opportunity to take an additional year between the traditional third and
fourth year, depending on their own learning and career goals. They can participate in formal
research or service-learning project, or take an active part in global health experiences. Students
can obtain a Master of Science in clinical research methods or a Masters in Bioethics. These
programs require an extra year to complete the didactic work. MD, MS, or MD, MBE degrees are
conferred at graduation.
ED-26
Albert Einstein College of Medicine
Academic Year 2014-2015
A major part of the fourth year is an elective period of up to seven months in duration. Students
choose from a wide selection of electives depending on their own learning needs and career
preparation. Through the elective program, a student may choose to obtain additional subinternship experience, further training in ambulatory medicine and primary care, or participate in
a research project. Most electives are hosted by various departmental affiliates of the College.
Many electives also may be taken in other medical schools in the US or abroad. Funding is available
for students to travel abroad to participate in exchange programs with overseas medical schools or
obtain clinical or research experience in less developed nations.
d. In the context of the annotation to this standard and the definition of active learning (above), provide
examples that illustrate the opportunities that exist in the curriculum for students to do each of the
following:
Assess their learning needs, individually or in groups
Identify, analyze, and synthesize information relevant to their learning needs
Assess the credibility of information sources
Share the information with their peers and supervisors
Introduction to Clinical Medicine (ICM): Introduction to the Patient - Students conduct a selfassessment of each of two videotaped interviews. For the mid-course evaluation, students meet
individually with one of their small-group faculty leaders for a review of the videotape and their
self-assessment. Faculty encourage students to set personal learning goals based on this discussion.
After their final videotaped Interview Competency Exam at the end of the course, this process is
repeated: students review their learning goals and assess their progress in meeting them, as
measured by their performance on the videotaped interview.
Currently, students in the Introduction to the Patient course are assigned two short reflective essays
and one final reflective paper targeting specific aspects of their clinical experiences. Faculty and
students use a “Reflective Writing Rubric” to guide this process. Students share and discuss these
reflections with students and faculty in their respective ICM groups. Initiatives have been
undertaken with the third-year Patients, Doctors and Communities (PDC) course director to
facilitate a vertical integration of the reflective process with students during the clerkship year.
Medical Histology – Histology has two components: 1) “flipped classroom” exercises and 2)
preparation and oral presentation of histopathology relevant to specific diseases. In both exercises,
students must individually assess their own learning, analyze information relevant to their learning
needs, and assess the credibility of sources. In the flipped classroom, the student performs these
tasks individually and shares their experience with peers in the classroom during the selfassessment/problem solving class that follows their self-study. In the oral reports, student pairs
work together and present their work collaboratively.
Molecular & Cellular Foundations of Medicine (MCFM) - MCFM holds 11 small-group
conferences in which groups of 20-22 first year medical students are facilitated by a faculty,
medical student, or fellow. The first-year students are assigned reading and questions prior to the
conference. Facilitators ask students to assess and identify their learning needs as individuals and
as a group. Groups of 4-5 students then use both assigned and on-line resources to gather and then
critically assess the relevant information linked to their self-identified questions. After 10-12
minutes of group activity, the information relevant to each of the identified questions is discussed in
ED-27
Albert Einstein College of Medicine
Academic Year 2014-2015
a whole-group format with feedback from the facilitator. Typically, one person from a group will
start the recitation. The facilitator will elicit responses from other members of that group or other
groups, enhancing the student response and leading students to related areas of inquiry that may
not have been part of the slated assignment.
Nervous System & Human Behavior: The NS&HB small group sessions consist of three “casebased” topics. The class is divided into permanent groups of 12-14 students and an assigned faculty
facilitator. The case material is not posted prior to the session, but instead is distributed, part-bypart, during the sessions. The progressive release of additional information is designed to
strengthen or complicate the diagnosis. At the conclusion of each 2-hour small group session, the
students generate Learning Objectives/Homework requiring their further exploration (e.g., outline
the common types of cerebral aneurisms and their available treatment options). The students in
each group work together to assign coverage of the material and to organize the distribution of the
obtained information within the group.
Introduction to Clinical Medicine (ICM): The Clinical Examination – Second-year students are
assigned to work together in pairs at clinical sites during this course. Students participate in an
initial reflective goal-setting exercise regarding their communication skills with patients at their
clinical sites. Several weeks later, the student pairs reconvene for a reflective session. Student pairs
exchange and give feedback to each other on their stated goals after having had a period of time to
observe each other with patients.
Bioethics 1 and 2 – One 90-minute session in Bioethics 1 is dedicated to Ethical Issues in Genomic
Medicine. The goals of the session are: 1) to identify key ethical issues in genomic medicine; and 2)
to participate in a debate in order to learn how to crystallize and analyze ethical arguments.
Students work in small groups to formulate arguments related to an ethical issue in genetics.
Students use the Internet and any other available sources to research the topic, create arguments,
and actively debate each other. A similar debate format session (60 minutes) is held in Bioethics 2.
Epidemiology, Population Health, and Evidence-Based Medicine (EPHEM) 2 - In the second year,
the EPHEM 2 course introduces students to concepts and problems in population health,
epidemiology, clinical epidemiology and evidence-based medicine. The goal of the course is for
students to develop the skills needed to critically analyze the medical literature in order to
understand: 1) The distribution and determinants of disease in populations; 2) The elements of
diagnosis, treatment, and prognosis of disease in individuals; and 3) The application of these to the
health of populations and individual patients. Much of the content covered in EPHEM 2 is
integrated and revisited throughout the clinical years.
Pediatrics Clerkship – Students participate in seven problem-based learning case discussions. These
standardized small-group sessions take place weekly at each clinical site for the entire rotation. The
cases cover crucial topics outlined in the national Council on Medical Student Education in
Pediatrics (COMSEP) pediatric curriculum. The groups are student-centered and use a two-part
format: the first day students discuss the history and physical, identify possible diagnoses, and
identify individually and as a group where they need more information. Each student chooses a
learning issue to research. The group reconvenes several days later to share information and to
discuss the case in light of that new information. They will then receive new laboratory data,
evolving medical and psychosocial information, and eventually the conclusion of the patient’s case.
ED-28
Albert Einstein College of Medicine
Academic Year 2014-2015
Family and Social Medicine Clerkship – As part of the Community Project completed during six
afternoons over the 4-week clerkship, students complete an individual self-reflection worksheet
requiring them to identify: their own strengths and areas for improvement in knowledge and skills
applicable to the project; any concerns and/or anticipated challenges about completing the project;
and three personal learning goals. The projects require students, working in teams, to define and
analyze a health problem in a specific population. Teams work in existing community-based
programs to develop brief health education interventions to address an identified need. The project
culminates in an oral presentation to the entire cohort of students for that rotation, faculty
evaluators, and invited community and faculty guests.
Students participate in three team-based learning sessions during their four-week rotation focused
on health promotion and disease prevention; patient-centered management of hypertension and
hyperlipidemia; and diabetes standards of care and quality improvement principles. Starting in the
2014-15 academic year, students will reflect, self-assess and peer-assess their individual
accountability to their teams and on their team communication skills. The exercise will allow
students to create an individualized learning plan to develop their team.
Clinical Skills Assessment (CSA) Program - The CSA is conducted at the end of the third year for
all Einstein students. The exam is similar in design to the USMLE Step 2 CS exam and covers all
content areas in the major clerkships. In addition to a diagnostic challenge, each case also includes
a psychosocial component, which poses an interpersonal or communication challenge. Students are
given the opportunity to review and self-assess their own videotape of their encounters. They are
also offered the opportunity to review their videotaped encounters with three of their peers and a
faculty facilitator for feedback. They also provide feedback to their peers on their performance.
Scholarship Requirement - The College offers a broad range of research and service opportunities
enabling students to pursue their individual interests and enhance their own education beyond the
core curriculum. As part of the Einstein experience, all medical students (with the exception of
MSTP students) are required to submit a Scholarly Paper (SP), based on a mentor guided project,
in order to graduate. Additionally, we offer a scholarly concentration program, Student
Opportunities for Academic Research (SOAR), for up to 20 students per class for a more intensive
mentor-guided research experience.
Scholarly Paper (SP): All students at Einstein write an SP based on a mentor-guided project. Many
seek out the Office of Medical Student Research for advice about potential mentors, but many
students use faculty software, the medical student faculty research directory, other resources about
faculty and word of mouth. This often takes place after the student has decided on a medical
specialty, which guides their choice of a mentor for the paper. While submission of the SP is
required for graduation, it is largely driven by the medical student and vetted by the mentor and
the Office of Medical Student Research. The writing of the SP is a significant undertaking
underscoring the relation of research and the application of evidence to medical practice or
delivery or understanding disease pathogenesis.
Student Opportunities for Academic Research (SOAR): All SOAR students are affiliated with one
of eight concentrations (aging, bioethics, clinical research, global health, integrative medicine,
public health, urban community health, and translational science, each of which is led by a
concentration director who oversees their progress, mentors the student, and acts as a liaison with
the primary mentor). SOAR students then develop relationships with the primary mentor for their
project and the director of their chosen concentration. The SOAR students’ seminar series includes
a discussion of “mentoring up” which specifically addresses the need for students to identify their
ED-29
Albert Einstein College of Medicine
Academic Year 2014-2015
academic and research needs and their own responsibility to reach out to their main mentor. They
are also encouraged to reach out to faculty with expertise or special knowledge that can enrich their
research, broadening the breadth of their mentoring. All SOAR students are required to submit a
capstone project by the end of their fourth year.
All Clerkships – All students on required clinical rotations in third-year clerkships and fourth-year
rotations > 4 weeks in length (Neurology, Sub-internships and Ambulatory Care) must receive
individual mid-cycle feedback. Mid-cycle feedback sessions must include the following components
Review of progress in completion of required elements of the rotation
Review of patient logs (occurs on all clerkships regardless of duration)
Meaningful review of clinical performance
Student self-assessment with format determined by each clerkship/sub-internship
Identification of areas of strength and areas needing improvement
Setting of learning goals for remainder of rotation
(See ED Appendix G for mid-cycle feedback guidelines, basic form, and examples of mid-cycle tools
from Ob/Gyn and Pediatrics clerkships.)
e. Describe where and how in the curriculum there is assessment of students’ progress in developing the
skills needed for lifelong learning, including the ability to learn through self-directed, independent study.
In the Appendix, provide examples of any instruments used for such assessment.
The Einstein Educational Competencies include nine sub-competencies under four major
competency domains related to student development of self-directed, life-long learning skills. The
grid below provides examples of four of these sub-competencies, where they are taught, and how
they are assessed in courses and clerkships.
Einstein Competency: Physician as Educator
Sub-competency
D3. Create conducive learning
environments and encourage
self-directed learning.
Year/Courses/Clerkships
Year 1:
Histology
Disease Mechanisms
Year 2:
ICM-Physical Exam
Repro Pathology
Year 3:
Family Med Clerkship
Medicine Clerkship
OB/GYN Clerkship
Pediatrics Clerkship
ED-30
Assessment Methods
Participation, multisource assessment,
self-assessment
Participation, self-assessment
Peer assessment
Participation
Project assessment, institutionally
developed written exam
Clinical performance checklist,
narrative assessment, multisource
assessment
Clinical performance checklist,
Institutionally developed clinical
performance exam, participation,
project assessment
Clinical documentation, oral patient
Albert Einstein College of Medicine
Academic Year 2014-2015
Patient, Doctors and
Communities
presentation
Oral patient presentation,
participation, portfolio-based
assessment, self-assessment, practical
lab
Year 4:
i. Clinical documentation, clinical
Sub-I: Medicine
performance checklist, multisource
assessment, narrative assessment
Einstein Competency: Physician as Role Model
Sub-competency
Year/Courses/Clerkships
Assessment Methods
F5. Learn and regularly practice
Year 1:
self-reflection to promote
ICM-Clinical Experience
ii. Participation, self-assessment,
personal growth and
ICM-Introduction to
narrative assessment
development.
Patient
iii. Clinical performance checklist,
narrative assessment, peer
assessment, self-assessment
Histology
iv. Peer assessment, self-assessment
Anatomy
v. Peer assessment, self-assessment
Year 2:
Microbiology / ID
a. Peer assessment, self-assessment
Year 3:
Family Med Clerkship
b. Clinical performance checklist,
Institutionally developed clinical
performance exam, project
assessment, self-assessment
Medicine Clerkship
c. Oral patient presentation,
participation, narrative assessment
Psychiatry Clerkship
d. Clinical performance checklist,
narrative assessment, participation,
self-assessment
Patient, Doctors and
e. Oral patient presentation,
Communities
participation, portfolio-based
assessment, self-assessment
Year 4:
Ambulatory: Family Med
1)
Clinical performance checklist,
self-assessment
Sub-I: Family Medicine
2)
Clinical documentation, clinical
performance checklist, narrative
assessment
Sub-I: Medicine
3)
Clinical documentation, clinical
performance checklist, multisource
assessment, narrative assessment
Sub-I: Pediatrics
4)
Clinical performance checklist,
narrative assessment, Oral patient
presentation, self-assessment
Einstein Competency: Physician as Life-long Learner
Sub-competency
Year/Courses/Clerkships
Assessment Methods
G1. Learn to review and
Year 1:
critically appraise medical
Histology
1)
Oral patient presentation
literature.
Disease Mechanisms
2)
Institutionally developed written
ED-31
Albert Einstein College of Medicine
Academic Year 2014-2015
EPHEM 1
exam
3)
Institutionally developed written
exam, participation, practical lab
4)
Institutionally developed written
exam, participation
Renal
Year 2:
EPHEM 2
Microbiology / ID
Musculoskeletal
Year 3:
Medicine Clerkship
OBGYN Clerkship
Psychiatry Clerkship
Year 4:
Sub-I: Medicine
Neurology
Sub-competency
G3. Demonstrate ongoing selfassessment of personal
knowledge and correction of
deficiencies.
Year/Courses/Clerkships
Year 1:
ICM-Introduction to
Patient
Histology
Anatomy
Renal
Year 2:
ICM-Physical Exam
Microbiology / ID
Year 3:
Family Med Clerkship
ED-32
Institutionally developed written
exam, practical lab
Institutionally developed written
exam, participation, oral patient
presentation
Institutionally developed written
exam
5)
Oral patient presentation,
participation
6)
Clinical performance checklist,
participation, nationally standardized
exam, project assessment, clinical
documentation
7)
Clinical performance checklist,
participation, self-assessment,
nationally standardized exam,
institutionally developed written
exam, oral patient presentation
8)
Clinical documentation, clinical
performance checklist, multisource
assessment, narrative assessment
9)
Clinical documentation,
narrative assessment, oral patient
presentation, nationally standardized
exam
Assessment Methods
10)
Clinical performance checklist,
narrative assessment, peer
assessment, self-assessment
11)
Self-assessment, peer
assessment
12)
self-assessment, peer assessment
13)
Participation, self-assessment
14)
Self-assessment
15)
Self-assessment, peer
assessment
16)
Clinical performance checklist,
institutional developed clinical
performance exam, project
Albert Einstein College of Medicine
Academic Year 2014-2015
Medicine Clerkship
Patients, Doctors and
Communities
Year 4:
Ambulatory: Family Med
Ambulatory: Medicine
Sub-I: Family Medicine
Sub-I: Medicine
Sub-I: Pediatrics
assessment, self-assessment
17)
Clinical performance checklist,
narrative assessment, multisource
assessment, participation
18)
Oral patient presentation,
participation, portfolio-based
assessment, self-assessment, clinical
performance checklist
19)
Clinical performance checklist,
self-assessment
20)
Clinical performance checklist,
self-assessment
21)
Clinical documentation, clinical
performance checklist, narrative
assessment
22)
Clinical documentation, clinical
performance checklist, multisource
assessment, narrative assessment
23)
Oral patient presentation, selfassessment, clinical performance
checklist, narrative assessment
See ED Appendix H for examples of assessment tools from the following courses and clerkships:
1. ICM-The Clinical Experience course - Students are assessed by clinical faculty on their abilities
to:
Demonstrate understanding of the limitations of the student role
Motivation and industry to seek out additional tasks and learning opportunities
Accept direction and/or criticism and utilize feedback to improve skills
2. ICM- Introduction to the Patient – Students are assessed by clinical faculty on their ability to:
Critically reflect on lessons learned and how they will change their behavior in the future based
on them.
3. Family and Social Medicine Clerkship – Students are assessed on their community projects by
faculty on their abilities to:
Appraise evidence-based studies related to health problems and interventions in both clinical
and community settings.
Participate in effective collaborative teaching and learning activities with peer medical students.
Discuss limitations of their projects and formulate future recommendations.
4. Pediatrics Clerkship – Students are assessed on their ability to demonstrate the following lifelong learning skills during problem-based learning sessions:
Active participation and engagement in group discussion.
Identification of own and group’s educational needs (learning issues).
willingness to elicit and responds constructively to feedback.
ED-33
Albert Einstein College of Medicine
Academic Year 2014-2015
f. Is demonstration of these skills considered as a criterion for grading in any course or clerkship
rotation?
In the ICM-Introduction to the Patient course, first-year students are assessed by clinical faculty on
their ability to critically reflect on lessons learned and how they will change their behavior and
integrate this change in future encounters. The reflective writing assignments are graded by faculty
using the Reflective Writing Rubric. The reflection assignments are required to pass this course.
In clerkships, faculty evaluate students on two competency-based objectives linked to the Einstein
competency: “Physician as lifelong learner.” The first objective is focused on self-directed learning
by asking faculty, site directors and clerkship directors to assess students’ ability to identify and
address their own educational needs. The second objective asks faculty, site directors and clerkship
directors to assess students’ ability to demonstrate willingness to elicit and respond constructively
to feedback.
Also see Required Courses and Clerkship Rotations (A. Summary Data).
ED-34
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-6. The curriculum of a medical education program must incorporate the fundamental
principles of medicine and its underlying scientific concepts; allow medical students to
acquire skills of critical judgment based on evidence and experience; and develop medical
students' ability to use principles and skills wisely in solving problems of health and
disease.
ED-7. The curriculum of a medical education program must include current concepts in
the basic and clinical sciences, including therapy and technology, changes in the
understanding of disease, and the effects of social needs and demands on care.
_____________________________________________________________________
The questions below are related to standards ED-6 and ED-7.
a. Provide one or more examples of where in the curriculum students are introduced to and expected to
demonstrate the following:
1. Skills of critical judgment based on evidence:
Molecular & Cellular Foundations of Medicine (MCFM) -Year 1 Course
Einstein sub-competency B4 of Physician as Scientist is Use knowledge of science and the scientific
method to characterize the quality of evidence, and to critically evaluate scientific and medical
literature. To that end, students are assigned articles from the scientific and medical literature to
read, discuss among themselves and critically evaluate with respect to validity of conclusions.
Recent examples are articles on second generation Gleevecs and correlation of PET scan data with
KRAS status of tumors.
EPHEM I and II (Epidemiology, Population Health and Evidence-based Medicine) -Year 1 and 2
Courses
The objectives of EPHEM 1 and EPHEM 2 are to equip the students with the skills required to be
critical consumers of the medical literature. In EPHEM 1 students are introduced to the science of
preventive medicine and clinical research methods. Basic methodology of epidemiology and
biostatistics are introduced from the perspective of population-based approaches to preventive
medicine and public health/prevention. The application of population-based evidence to the care of
individual patients is introduced during the second year. In EPHEM 2, students apply these skills to
critically appraise the medical literature, interpret the results, and apply them to the care of
individual patients.
Family Medicine Clerkship
During the clerkship, in preparation for team-based learning (TBL) session about prevention, the
students are provided conflicting guidelines from different societies. They are asked to apply the
guidelines during the TBL quiz, and judge the evidence for guidelines as part of their discussion
with peers. They are then asked to engage in shared decision making with simulated patients
around cancer screening, based on the best available evidence, as part of their end-of-rotation
OSCE.
2. Skills of medical problem solving:
Year 1 and Year 2 Courses
ED-35
Albert Einstein College of Medicine
Academic Year 2014-2015
All first- and second-year courses have case-based, small-group conferences. Many of these test and
develop medical problem solving, from foundation science exercises on mechanism of disease, to
genetic counseling and ethical decision-making, to clinical decision-making as part of a
management plan in organ system courses.
All Required Clerkships
In all clerkships, students are expected to develop and improve their proficiency in solving medical
problems. This is achieved by presentation and discussion of their assigned patients or through
study cases. The student assessment form includes the competency of physician as healer, with subcompetencies related to problem solving in a clinical setting: e.g., the sub-competencies of clinical
judgment and patient management.
Family Medicine Clerkship
The clinical experiences for the clerkship students occur in a primary care setting, where students
have first contact with the patient. On average, students see two patients per half-day clinic session
and are expected to generate a diagnostic plan for undifferentiated complaints and/or a
management plan for established diagnoses. The students present this formulation to their clinical
preceptor for feedback on their clinical reasoning.
3. Knowledge and understanding of societal needs and demands on health care:
Family Medicine Clerkship
During the clerkship orientation lecture, students hear a review of the primary care needs to
maintain good health for the national population and the population in the Bronx. As part of the
required Community Project during the clerkship, students in pairs are required to use publicly
available data to establish the severity of a health problem in the community they are serving, as
well as the problem’s relation to social determinants of health, and compare this to national figures.
Population Health and the Practice of Medicine (PHPM) Working Group
A working group has recently reviewed this subject and identified these sub-domains of knowledge
to be integrated into the curriculum as part of future curricular change: Public Health and
Medicine, Health Disparities, and Determinants of Health and Community, Occupational and
Environmental Health. A new learner-centered PHPM longitudinal curriculum will be integrated
into required courses and clerkships starting in the 2014-15 academic year, and will continue to
integrate new PHPM content each academic year thereafter (See ED-10).
b. Indicate whether students are explicitly assessed on these skills and this knowledge in any required
courses or clerkship rotations. Describe the manner in which the knowledge and skills are assessed.
Molecular & Cellular Foundations of Medicine (MCFM) -Year 1 Course
Comprehension of the assigned articles, which are not discussed in conference or didactic sessions
of MCFM, is assessed on the next MCFM exam. By cataloging questions on MCFM exams, i.e.,
linking questions to sub-competencies, the MCFM course director can determine student progress
in mastering critical evaluation of the scientific and medical literature.
EPHEM 1 and 2 (Epidemiology, Population Health and Evidence-based Medicine) -Year 1 and 2
Courses
The course grade I EPHEM 2 comprises grades on the quizzes (20%) and the final exam (80%).
For the final exam students are assigned to read a journal article and tested by short answer and/or
ED-36
Albert Einstein College of Medicine
Academic Year 2014-2015
essay questions on their interpretation of data in the article. In EPHEM 2, three multiple-choice
quizzes and a multiple-choice exam constitute 30% and 70% of the course grade, respectively.
All Required Clerkships
There is a specific competency on the Evaluation of Clinical Performance and Professional
Attributes form that assesses the student’s clinical judgment.
Family Medicine Clerkship
During the clerkship, team-based learning provides the opportunity to assess problem solving,
clinical reasoning, and decision making through the individual/group quiz questions based on
online modules reviewed by students prior to the session. Together, these quizzes account for 15%
of each student’s overall grade. Students are assessed on their application of shared decisionmaking around conflicting guidelines for cancer screening, during an end-of-rotation OSCE station
with a simulated patient. Students are assessed on their ability to use data to establish the severity
and social determinants of a community-wide health problem, as part of their final presentation,
judged independently by three faculty judges using the same grading rubric.
ED-37
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-8. The curriculum of a medical education program must include comparable
educational experiences and equivalent methods of assessment across all instructional sites
within a given discipline.
Compliance with this standard requires that the educational experiences at all instructional sites be
designed to achieve the same educational objectives. Course or clerkship rotation length must be
identical, unless a compelling reason exists for varying the length of the experience. The instruments and
criteria used for medical student assessment, as well as the policies for the determination of grades,
should be the same at all instructional sites. The faculty who teach at all instructional sites should be
sufficiently knowledgeable in the subject matter to provide effective instruction and have a clear
understanding of the objectives of the educational experience and the assessment methods used to
determine achievement of those objectives. Opportunities to enhance teaching and assessment skills
should be available for faculty at all instructional sites.
Although the types and frequency of problems or clinical conditions seen at each instructional site may
vary, each course or clerkship rotation must identify any core experiences needed to achieve its objectives
and ensure that students receive sufficient exposure to such experiences. Similarly, although the
proportion of time spent in inpatient and ambulatory settings may vary according to local circumstances,
in such cases the course or clerkship rotation director must ensure that limitations in learning
environments do not impede the accomplishment of objectives.
To facilitate the comparability of educational experiences and the equivalency of assessment methods, the
course or clerkship rotation director should orient all participants, both faculty and students, to the
educational objectives and grading system used. This orientation can be accomplished through regularly
scheduled meetings between the director of the course or clerkship rotation and the directors at the
various instructional sites that are used.
The course and clerkship rotation leadership should review medical students’ evaluations of their
experiences at all instructional sites to identify any persistent variations in educational experiences or
assessment methods.
______________________________________________________________________________
. List the courses and clerkships/clerkship rotations that are offered at more than one teaching site:
Introduction to Clinical Medicine (ICM) – The Clinical Experience (Year 1)
Introduction to Clinical Medicine (ICM) – The Clinical Examination (Year 2)
All third- and fourth-year clerkships
For each course or clerkship rotation offered at more than one teaching site, describe the following:
b. The means by which faculty members at each site are informed of and oriented to the objectives and
grading system for the course or clerkship rotation.
Pre-clerkship Courses:
Year-1 ICM: The Clinical Experience:
The clinical placements used for this course are divided among programs that break down along
discipline lines. These include: 1) Emergency Medicine, 2) Primary Care & Subspecialties, 3)
Geriatrics, 4) Hospitalists, 5) Pediatrics, 6) Psychiatry, 7) Rehab Medicine, 8) Substance Abuse, and
ED-38
Albert Einstein College of Medicine
Academic Year 2014-2015
9) Women’s Health. Designated discipline coordinators assist the course directors in identifying and
recruiting physicians within their respective disciplines as preceptors for the course. These
coordinators sometimes serve as preceptors themselves, but generally have administrative
responsibilities, either within their discipline or department across clinical sites, or within a
department at a single site. They share oversight responsibilities with the course directors in terms
of preceptor coverage and other logistical issues, and might facilitate a didactic session with
students within the program or at a site.
All preceptors in each clinical program within the course are initially contacted by telephone or in
person to review the course objectives and to discuss how the objectives might be achieved at a
preceptor’s site, and with particular patient populations. Each preceptor receives a course syllabus
in which the goals, objectives, program description, procedures, expectations of students and
evaluation and grading criteria are explicitly stated. Each preceptor also receives the course
syllabus from the companion campus-based course, Introduction to the Patient, to enable them to
follow and understand the clinical interviewing skills that are a focus of that course, and to aid in
the preparation of students to enhance their learning and skill development in clinical settings.
The objectives shared by the two ICM first-year courses are the following:
1. Conduct a medical interview: Demonstrate ability to simultaneously elicit pertinent biological,
psychological, and social information, while building a therapeutic relationship with the patient.
2. Demonstrate physical examination technique of the heart, lungs and abdomen on patients.
3. Utilize feedback from peers and preceptors to improve medical interviewing, physical examination
skills and patient presentations.
Year-2 ICM: The Clinical Examination:
At each of the clinical sites, we designate a clinical site leader who is responsible for recruiting the
preceptors at a particular site. Once these site leaders are recruited, the ICM administrative office
staff collects the preceptors’ contact information so that we can communicate directly with them
about course-related matters. Before the course begins, we email all preceptors a faculty guide that
includes dates, course objectives, and a teaching plan by session and criteria for evaluation.
Specifically, we have devised a teaching model of observation and direct feedback at the bedside
specific to the course, which is thoroughly described in the faculty guide.
Common objectives for all clinical sites in Part II of this course are as follows:
Course Objectives – PART II:
1. Apply basic science knowledge, i.e., anatomy, to inform proper performance of PE techniques
2. Demonstrate proper use of instruments commonly employed in the medical examination of patients
including: stethoscope, sphygmomanometer, ophthalmoscope, otoscope, reflex hammer, and tuning
fork.
3. Demonstrate all the components of the physical examination of the various body parts and systems
including: head and neck, eyes, ears, nose, throat, pulmonary, cardiovascular, abdomen,
musculoskeletal, and neurological.
ED-39
Albert Einstein College of Medicine
Academic Year 2014-2015
4. Conduct a medical interview to obtain a detailed history of present and past illnesses and a complete
review of systems.
5. Demonstrate sensitivity to the patient’s level of comfort during the physical examination.
6. Demonstrate ability to gather data in the process of observation of the patient as a clinical skill.
7. Utilize data gathered by observation, patient history and physical examination to inform
development of differential diagnoses.
8. Demonstrate physical examination maneuvers on a patient in a logical and focused manner.
9. Recognize the range of normal physical examination findings.
10. Recognize and interpret abnormal physical examination findings.
11. Use effective listening skills that recognize patients’ verbal, non-verbal and contextual cues while
eliciting the history and during the performance of the physical examination.
12. Formulate a basic patient problem list.
13. Organize historical and physical findings in a logical, standardized manner for delivery of a clear,
concise and relevant oral presentation and written case history.
14. Reflect on individual learning goals for professional development.
Clerkships:
There is a variety of methods used by the required clerkships to orient faculty to the objectives and
grading policies of the rotation. These include:
Regular meetings of the clerkship directors with their site leaders, who then disseminate
information to the faculty at their respective clinical sites. (Internal Medicine, Pediatrics,
Surgery, Ambulatory Medicine, Psychiatry, Ob/Gyn)
Distribution of written materials, on paper or electronically, which include goals, objectives,
expectations, responsibilities, Einstein educational competencies, and student evaluation
form with instructions to all faculty at a site, by the clerkship director or site director. (all
clerkships)
Posting on each individual clerkship’s webpage on eMED, the school’s online education
management system. (all clerkships)
Regularly scheduled faculty meetings, where clerkship directors and/or site leaders discuss
these and other student education related issues. (Neurology, Family Medicine, Geriatrics)
Annual or biennial site visits by clerkship director. (Internal Medicine, Family Medicine)
c. How and how often the individuals responsible for the course or clerkship rotation communicate with
faculty at each site regarding course or clerkship planning, implementation, student assessment, and
course evaluation.
Pre-clerkship Courses:
Year -1 ICM: The Clinical Experience:
Communication between the course directors, program coordinators and preceptors is ongoing.
Targeted face-to-face meetings, program review and revisions take place from late spring to the
ED-40
Albert Einstein College of Medicine
Academic Year 2014-2015
start of the academic year. Face-to-face meetings prior to the beginning of the course are done with
all newly recruited preceptors and done on-site for newly acquired sites. Throughout the course,
there is communication by email with program coordinators and preceptors to check in, elicit any
questions or concerns, make announcements, and send reminders about deadlines, etc. Throughout
the year, course directors have lunch meetings with students by program to find out how things are
going at each clinical site. If any problems are elicited from the students, their concerns are
addressed directly with program coordinators and preceptors. Student evaluations are sent to each
preceptor prior to the end of the course to encourage and facilitate preceptor/student discussion of
the evaluation, and opportunities exist at that point for preceptors to raise issues or questions with
the course directors.
Year-2 ICM: The Clinical Examination:
In addition to sending materials electronically at the beginning of the course, we arrange meetings
with groups of preceptors at the various sites. All new preceptors meet with the course leaders
before the beginning of the course to review the learning objectives, teaching strategies and faculty
guide. Also, throughout the duration of the course, we send emails (approximately 3 times per
course year) soliciting feedback from preceptors and the clinical site leaders about how things are
going in general. Any identified problems are followed up with a phone call to the preceptor/clinical
site director or an individual meeting is scheduled. We also send email reminders to faculty about
when the students’ case write-ups are due and encourage them to give feedback to students before
the subsequent one is due. In particular, several weeks before the end of the course, we email
student evaluation forms to the preceptors asking them to complete these evaluations of students.
We ask them to spend 15 minutes on the last clinical days going over the evaluations with them.
Specific instructions for returning the completed evaluations with both the student’s and
preceptor’s signature are included in these communications.
Clerkships:
Clerkship directors interact primarily with clinical teaching faculty through the clerkship site
leaders. Clerkship site leaders have ongoing communication, either directly at faculty meetings,
through individual discussions at the smaller sites or through email, with faculty involved in
student teaching and assessment to keep them apprised of new and ongoing clerkship activities,
curriculum, and student evaluation. The frequency of communication varies, but is at a minimum
annually and in some cases is as often as weekly or biweekly. Most of the time, it is the site leader
who informs site faculty of clerkship activities, although some clerkship directors make annual site
visits themselves to enhance communication.
d. The process by which faculty development activities related to teaching and assessment are made
available to instructional staff across sites and the frequency with which these activities are provided.
The Office of Faculty Development (OFD) currently presents a number of faculty development
sessions designed to develop the skills of our faculty as medical educators. All faculty development
programs are offered throughout the year without charge to all faculty at Einstein and at its
affiliated sites. (See ED Appendix I for Faculty Development Calendar.)
The session entitled “How to Enhance Your PowerPoint Presentation” demonstrates how to
improve student participation in lectures using Audience Response Systems and other active
learning tools. The “Assessment of Learning” series covers the following topics: “Writing and
Evaluating Multiple-Choice Questions,” “Incorporating Formative Assessment into Teaching,” and
“Classroom Assessment.” The office also sponsors successful sessions on Giving Feedback. A
session targeting hospitalists, entitled “Teaching on a Busy Inpatient Ward,” reviewed many tools
ED-41
Albert Einstein College of Medicine
Academic Year 2014-2015
and techniques, such as teaching micro skills and the RIME technique. A recent off-campus
workshop, held at Beth Israel Medical Center, focused on “Bedside Rounds: A Learning Toolbox”
and reviewed the framework and practical teaching skills used when the patient is present.
The OFD sponsors sessions on Team-Based Learning (TBL 101 and 102). TBL 101 is a freestanding
session introducing the learner to TBL. As a follow-up to the TBL 101 workshop, TBL 202 offers a
six-session series to assist faculty participants in creating their own TBL activities
Additional Campus-wide Offerings:
There are several annual, daylong Einstein-sponsored faculty development activities geared
towards teaching faculty across clinical sites.
Annual Clerkship Retreat-organized by the Clinical Directors Subcommittee of the Medical
Education Council based on needs of clerkship faculty. Attended by 80-100 clerkship site
leaders and key teaching attendings from all clinical sites in all major disciplines. Programs
include talks by nationally recognized keynote speakers, large- and small-group interactive
sessions and workshops focusing on teaching and assessment skills. Recently covered themes
include:
2010 - Use of Simulation in Teaching and Assessing Clinical Skills
2011- Residents as Teachers
2012 - Enhancing Clinical Teaching
2013 - Assessing Clinical Competency
2014 - Inter-professional Education
Davidoff Education Day- sponsored by the Office of Medical Education and Office of Faculty
Development to recognize the critical roles that medical education and mentoring play at
Einstein and to provide opportunities for Einstein faculty to improve their skills as medical
educators. In addition to keynote addresses by national figures and small group workshops,
over 100 faculty showcase their innovative work in medical education at Einstein at a lively
poster session.
Recent themes include:
2010 - Innovations in Medical Education
2011 - Curricular Enhancement
2012 - Social Media in Medical Education
2013 - Competency-based Medical Education
2014 - E-Learning
Summer Intensive for New Medical Educators – initiated in summer 2013, this is a new annual
event targeted to new teaching faculty, covering basic topics in medical education including
adult learning theory, teaching in various clinical venues, assessing the learner, and giving
feedback. The second annual Summer Intensive is schedule for July 16, 2014.
Course-specific Offerings:
Year-1 ICM: The Clinical Experience:
This course, which places first-year students at clinical sites and physicians’ offices in the
community and throughout our affiliate network, offers faculty development workshops for
preceptors in order to enhance the teaching skills of the faculty and to ensure that the objectives of
ED-42
Albert Einstein College of Medicine
Academic Year 2014-2015
the program are met. When physical examination (PE) skills were integrated into the course
curriculum, a series of both on-campus and on-site faculty development workshop sessions for
CME credit were held to inform faculty on which PE skills students would be assessed and to
practice feedback skills based on direct observation to enhance faculty teaching of the students in
this area.
Clinical Experience preceptors also receive descriptions and invitations to selected campus faculty
development sessions relevant to their career and clinical enhancement and student teaching.
Year-2 ICM: The Clinical Examination:
Each year, ICM offers faculty development sessions with CME credit to all preceptors teaching in
Part 1 or Part 2 of the course. These sessions begin with a general introduction to the course, review
of objectives and teaching strategies, which is followed by an educational activity to bolster
preceptors’ clinical knowledge and/or teaching skills. Each year these faculty development sessions
involve outside faculty and focus on enhancing the faculty’s knowledge and skills in a particular
area of physical examination education. For example, this past year faculty from the departments
of orthopedics and rheumatology led a workshop on the musculoskeletal exam.
Family Medicine Clerkship Year 3:
Family Medicine provides an annual evening faculty development session repeated on two evenings
in different geographic areas to maximize participation by clerkship faculty. Some examples of
topics on teaching include Breaking Bad News to Students, What is Honors?, Professionalism in
Medicine-Recognizing a Teaching Opportunity, Agenda Setting and Questioning as a Tool for
Effective Teaching. The Faculty Development Fellows also sponsored a workshop on Implicit Bias
that was open to all faculty at our sites and there was a departmental Grand Rounds on Teaching
in the Patient's Presence. These faculty development sessions are also used as an opportunity to
review curricular and organizational changes in the clerkship and in the institution.
e. The mechanisms used for review and sharing of student evaluations of their educational experiences,
data regarding students’ completion of required clinical experiences, student performance data, and any
other data reflecting the comparability of learning experiences across sites. Describe the specific types of
data reviewed and the individuals or groups responsible for reviewing the information.
Pre-Clerkship Courses:
Year-1 ICM: The Clinical Experience:
Students evaluate their experience and preceptor via required, online evaluations at the conclusion
of the course. These course evaluations ask many detailed questions about the students’ perception
of the teaching by their preceptor, the learning experience at their clinical site as well as all other
aspects of the course. Preceptors do not see how students have evaluated them until after
submitting each evaluation to the course directors. Individual preceptors receive the studentgenerated evaluations from the students they have precepted in the course. Additionally, preceptors
receive data tables which allow them to compare the scores they have received from students to
mean scores for comparable items for both preceptors within their clinical program (i.e. Geriatrics,
Emergency Medicine, Women’s Health, etc.) and with preceptors course wide.
Preceptors complete detailed course evaluations based upon their observations and assessments.
This course has no examinations or structured performance-based assessments. If a student
receives a “Does not meet criteria” assessment on one or more items on the evaluation, or receives
an overall grade of Fail for the course, the course directors speak directly with the preceptor to
discuss how the evaluation was determined and how the standards and criteria were interpreted for
ED-43
Albert Einstein College of Medicine
Academic Year 2014-2015
the student’s assessment. Where appropriate, a remedial action plan is developed and, in the case
of student failure, the school’s Office of Student Affairs is notified.
Year-2 ICM: The Clinical Examination:
Course directors review the results of students’ clinical skills performance scores on our end-ofcourse standardized patient encounter assessment as a collective consideration to identify strengths
and weaknesses in our clinical teaching program and detect major differences between sites.
In addition, the Evaluation Sub-committee reviews all end-of-course evaluation data and provides
detailed reports to the course directors. Course directors respond in writing; this information is
also presented annually to the Course Directors Sub-committee, and sub-committee members offer
suggestions on ways to improve inconsistencies across sites.
Clinical Clerkships and Sub-internships:
For the required clinical clerkships and sub-internships, there are multiple sources of information
used to compare student experiences across sites. These include mandatory student evaluations of
the clerkship, student log data, and grade distribution across sites.
At the conclusion of each required clerkship, students must complete a comprehensive evaluation of
the rotation containing questions related to four major areas: orientation/organization,
teaching/teachers, feedback/evaluation, and global assessment. They are also asked for comments
on strengths of the clerkship, suggestions for improvement, and any mistreatment they may have
experienced. Responses are anonymous and pooled, and reported biannually by the Office of
Educational Resources to clerkship directors, the senior associate dean for medical education, the
deans of students, and the assistant deans at the sites. The numerical data as well as all comments
are reported by site. This report provides clerkship directors with detailed information on the
student experiences at all sites and their comparability. Clerkship directors review the information
with their site leaders and ascertain that inconsistencies across sites are addressed. Because of the
multiple sites and preceptors participating in the Family Medicine clerkship, additional student
feedback is obtained from internal surveys, and data are aggregated across students by an educator
not involved in grading, reviewed by the clerkship directors, and delivered to faculty electronically
twice a year, with comparisons between sites provided.
In May 2013, a final list of procedures and common conditions all Einstein students must encounter
in required clerkships and sub-internships was established and approved by the Clinical Directors
Subcommittee for use beginning with the 2013-14 academic year. This list of requisite educational
experiences is known as the Einstein 203, and all students must log these encounters in our eMED
learning management system. Using cumulative student log data, the Office of Educational
Informatics generates a report every six months of the students’ completion rate of requisite
educational experiences across all clinical sites within each required clerkship/sub-internship A
copy of the individual clerkship/sub-internship site comparability report is provided to each
clerkship director for review. The clerkship/sub-internship directors are responsible for sharing
this report with their clinical site directors.
Once a year, the Office of Student Affairs and Registrar provide grade distribution data by
clerkship and by site within each clerkship to all clerkship directors and deans of medical
education. Clerkship directors address inequalities directly with their respective site leaders who in
turn work with their faculty to improve and ensure standardization of student evaluation and
clerkship grading across sites.
ED-44
Albert Einstein College of Medicine
Academic Year 2014-2015
The Evaluation Sub-committee reviews all end-of-clerkship evaluations and site comparability data
for each clerkship/sub-internship annually. Site-specific information is integrated into the
Evaluation Sub-committee’s report to each clerkship/sub-internship director. The clerkship/subinternship director responds in writing to the Evaluation Subcommittee report and presents the
data and response to the Clinical Directors’ Subcommittee. As part of the discussion, the
clerkship/sub-internship director must address specific strategies for closing any comparability
gaps if they are noted, and subcommittee members also offer suggestions on ways to remove
inconsistencies across sites. In addition, site comparisons are one component of the Phase 2
clerkship review conducted by the Executive Committee (See p. ED-35).
f. The mechanisms employed to address inconsistencies across sites in such areas as student evaluations
of courses and clerkship rotations and students’ grades.
Pre-clerkship Courses:
ICM: Years 1 and 2:
The course directors review the students’ extensive and detailed course evaluations and analyze the
data by preceptor, by clinical site and by program. Program coordinators also receive copies of all
the individual preceptor evaluations from within that program, as well as the means tables
mentioned above for cross comparisons. Program coordinators and course directors use these
comparative data to identify deficits and any preceptors who may require remedial attention and
training.
Recently end-of-course preceptor evaluation of students was revised to include behaviorally
anchored criteria for each learning objective on the evaluation to assist preceptors in evaluating
student performance using more standardized measures and to strive for more descriptive
assessments that provide for greater consistency across preceptors, sites and clinical programs.
Clerkships:
Inconsistencies across sites in student evaluations and student grades are addressed at several
levels. First, semi-annual summaries of student clerkship evaluations are compiled by the Office of
Educational Resources and distributed to clerkship directors (as well as to the assistant deans at the
sites, the senior associate dean for medical education, department chairs, and the associate deans
for students). Clerkship directors review these in detail and share them with their site leaders,
addressing any inconsistencies in the educational experiences as reported by the students.
Additionally, shortly after each academic year, annual grade distribution statistics at all sites for
each required clerkship are distributed to all clerkship directors by the Office of Student Affairs.
Clerkship directors and site leaders work together to address discrepancies, such as by better
educating faculty on student assessment.
The school embarked on the development of a new assessment form, implemented for third year in
2013-2014 and for fourth year in 2014-2015, with a narrower grading scale and clear behavioral
anchors for each assessment. This is intended to reduce variation in grading, with reinforcement by
faculty development. In addition, the Clinical Directors Sub-committee has approved a policy that
over the course of an entire academic year, a maximum of 20-33% of students within a clerkship
could be awarded a grade of Honors.
ED-45
Albert Einstein College of Medicine
Academic Year 2014-2015
Clerkship directors use actual grade distribution information to make adjustments to grading
policy at the start of an academic year. The grade distributions are also used annually to modify the
weight of different aspects of the clerkship, and point-score cutoffs for different grades, in order to
produce a more normalized distribution of grades in the following year.
Also see information for standard ED-41in this section and standard FA-11 in Section IV if the school
operates one or more geographically separate/distributed campuses, as defined in the instructions.
ED-46
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-9. A medical education program must notify the LCME and the CACMS, when
applicable, of its plans for any major modification of its curriculum.
The notification should include the explicitly defined goals of the change, the plans for implementation, and the
methods that will be used to evaluate the results. Planning for curriculum change should consider the incremental
resources that will be required, including physical facilities and space, faculty and resident effort, library facilities
and operations, information management needs, and computer hardware.
_____________________________________________________________________________
a. Indicate the year that the last major revision of the curriculum was implemented:
N/A
b. Summarize the principal features of that curricular revision, including the reasons for the change and
the specific goals that the change was designed to accomplish.
The curriculum is continuously being updated and enhanced. Some of the changes have involved
the creation of new courses. In other cases, changes have been accomplished by instituting
curricular themes or interdisciplinary projects. Specifically, two new courses have been added in
the last few years, Bioethics and EPHEM, which successfully addressed identified deficiencies since
the last LCME visit. Highlights of these changes since the last LCME review include:
Creation of new courses that emphasize core competencies across disciplines:
A new bioethics course (Bioethics 1) was created for the academic year 2009-2010. The course
introduces first-year students to foundational ethical concepts, and provides them with a
framework to use in analyzing ethical dilemmas. The goals of the course are to enable students to
identify ethical issues in clinical and research situations, analyze ethical dilemmas using moral
reasoning skills, and recognize ethical issues associated with the information students are learning
in their first-years courses. Topics covered include informed consent, decision-making capacity,
ethical issues at the end of life, ethical issues in genetics, research ethics, and conflict of interest.
The bioethics training was extended to year two (Bioethics 2) in 2011-2012 to build upon the
foundational concepts introduced in year one and introduce more advanced topics such as ethical
issues in reproductive medicine, organ transplantation, and medical errors. In addition to Bioethics
1 and 2, sessions on Ethical Issues in Internal Medicine, and Ethical Issues in Pediatrics have been
introduced into the Medicine and Pediatrics clerkships, respectively. The purpose of these sessions
is to provide students with an opportunity to discuss and analyze real-world bioethical issues that
they are facing in these clerkships.
Creation of a new course spanning years one and two, entitled Epidemiology, Population Health,
and Evidence-Based Medicine (EPHEM). This course introduced the basic methodology of
biostatistics and epidemiology, utilizing a population based approach to preventive medicine and
public health. The course which started in the academic year 2012-2013 replaced and formally
integrated the material covered in two previous courses, the Principles of Preventive Medicine and
Clinical Research course in year one and the Evidence-Based Medicine Course in year two.
Establishment of a curricular theme designed to coordinate coverage of topics for areas that do not
readily fall under the realm of a specific course or clerkship:
ED-47
Albert Einstein College of Medicine
Academic Year 2014-2015
Population Health and the Practice of Medicine: A working group was formed in September 2013
and charged with developing a four-year longitudinal curriculum to address identified population
and practice of medicine gaps in our curriculum. The educational programs developed by this
working group will be integrated into existing courses and clerkships during the 2014-2015
academic year.
Development of an interdisciplinary educational project
Social Media and Professionalism: The development of this educational project was supported by a
grant from the Josiah Macy Jr. Foundation. It focuses on training medical students (and faculty)
about the benefits and potential challenges with utilizing social media as a health care professional.
The content is currently taught in several courses, including the Introduction to Clinical Medicine
in years 1 and 2, Bioethics in years 1 and 2, and the Patient, Doctors and Communities course in
year 3.
c. Describe the planning process for that curricular revision, identifying the individuals, committees, or
others involved.
The planning process for the above curricular enhancements was under the auspices of the
Executive Committee of the Medical Education Council (MEC) and its standing sub-committees
and task forces. The course director for Bioethics was identified by the former associate dean for
educational affairs, who was in charge of the medical education program through 2009. The
directors for EPHEM were appointed by the current senior associate dean for medical education
with approval by the Executive Committee. Each of the new course directors, the theme and project
directors worked with a core group of faculty with expertise in the respective content areas to
develop the programs.
d. Describe any plans for major modification of the present curriculum, along with the timetable for
planning and implementation.
With the introduction of the new Einstein Educational Competencies, there have been numerous
discussions within the MEC about the timing and process for modification of the present
curriculum. In the spring of 2013, a working group of faculty from several disciplines and students
was put together to examine whether the current clinical clerkship curriculum (the current third
and fourth year) could be redesigned to best address these competencies.
The working group was chaired by Dr. Jeffrey Levine, Assistant Dean at Bronx-Lebanon Hospital
Center and a member of the Clinical Directors Sub-committee. In addition to working group
meetings, Dr. Levine conducted qualitative interviews with each member of the working group to
gather input. Several key issues emerged from this process, including the need to: 1) provide more
flexibility in year three; 2) create more balance in the number of weeks that students spend in
different specialties; 3) develop intersessions during the clinical years that allow for integrating of
material from the preclinical curriculum, the new population health and practice of medicine
theme, and other interdisciplinary topics; 4) explore the possibility of creating an integrated
longitudinal clerkship and increasing time in the ambulatory setting; and 5) shorten the time in the
preclinical years to allow students to enter clerkships earlier than the summer of the third year.
Although valuable insights were gained from this process, the working group determined that it
would be difficult to modify the clinical curriculum alone without looking at the entire four-year
curriculum.
ED-48
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-10. The curriculum of a medical education program must include behavioral and
socioeconomic subjects in addition to basic science and clinical disciplines.
Lists of subjects widely recognized as important components of the general professional education of a physician are
included in the medical education database that is completed in preparation for full accreditation surveys.. Depth of
coverage of the individual topics will depend on the medical education program’s educational goals and objectives.
_____________________________________________________________________
a. Check the topics listed below that are included in the curriculum as part of a required course/clerkship
and/or an elective course. Provide the total number of sessions in which each topic is included in one or
more required courses and clerkship rotations in the preclinical and clinical phase of the curriculum. To
be included in this listing, the subject should be included in the objectives for the session or as a
significant topic covered during that session.
Content Area
Biostatistics
Biomedical informatics
Clinical/translational research
Communication skills
Community health
Complementary/alternative health
care
Cultural competence
End-of-life care
Epidemiology
Evidence-based medicine
Domestic violence/abuse
Global health issues
Health care financing
Health care systems
Health care quality improvement
Health disparities
Human development/life cycle
Human sexual/gender development
Human sexuality/sexual
functioning
Medical ethics
Medical genetics
Medical humanities
Medical jurisprudence
Medical socioeconomics
Nutrition
Occupational health/medicine
Subject Included in
Required
Course/
Clerkship
x
x
x
x
Elective
Course
x
x
Number of Sessions in
Required
Clinical
Preclinical
Clerkship
Course(s)
Rotation(s)
22
2
36
4
42
23
x
x
6
12
x
x
5
1
x
x
x
x
x
x
x
x
x
x
x
x
x
5
1
33
22
4
34
2
2
4
1
x
x
x
x
x
1
2
11
8
x
11
x
x
x
x
18
31
x
x
x
x
x
ED-49
3
2
10
10
2
2
2
2
1
2
5
2
1
3
Albert Einstein College of Medicine
Pain management
Palliative care
Patient safety
Population-based medicine
Prevention/health maintenance
Rehabilitation/care of the disabled
Research methods
Substance abuse
Academic Year 2014-2015
x
x
x
x
x
x
x
x
x
x
x
x
3
2
4
18
17
3
36
11
4
6
3
16
1
b. Describe any steps being taken to improve content coverage in any areas in which the medical school
has evidence or believes that more exposure is needed.
In August 2013, the Executive Committee charged the Population Health and Practice of Medicine
(PHPM) Working Group with the goal of developing a new thematic program focused on
enhancing the behavioral and socioeconomic education of our medical students. This action was in
response to a review of our AAMC GQ data showing many of our students rated their education on
a number of these subjects as inadequate. The membership of this working group includes content
experts, course and clerkship directors, and medical students, and is chaired by the assistant dean
for medical education. The PHPM Working Group reviewed competency-based guidelines from
several national societies (e.g., Association of Preventive Teaching and Research, Inter-professional
Education Collaboration, Institute for Healthcare Improvement, etc.) and appraised medical
education publications on best practices to teach these topics from other institutions. In December
2013, the working group established the following educational framework for the new curriculum:
The Population Health and Practice of Medicine Theme Curriculum
Domain: Population Health
Sub-domains:
1. Public Health and Medicine
2. Health Disparities and Determinants of Health
3. Community, Occupational and Environmental Health
Domain: The Practice of Medicine
Health Care and Quality Improvement
Enhancing Patient Safety in Medicine
Inter-professional Team Health Care and Training
Medical Economics
Health Care Systems
Practice Management
Law and Medicine
In addition, the PHPM established 147 competency-based learning objectives that will serve as the
foundation for this new curriculum. Each new PHPM learning objective was mapped to an Einstein
competency.
The working group conducted a needs assessment of students in early 2014 in order to assess in
baseline satisfaction, self-assessed competency, attitudes and knowledge on these subjects. The data
will help the PHPM Working Group to design a new learner-centered PHPM longitudinal
curriculum that will be integrated into required courses and clerkships starting in the 2014-15
academic year, and will continue to integrate new PHPM content each academic year thereafter.
ED-50
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-11. The curriculum of a medical educational program must include content from the
biomedical sciences that supports students' mastery of the contemporary scientific
knowledge, concepts, and methods fundamental to acquiring and applying science to the
health of individuals and populations and to the contemporary practice of medicine.
It is expected that the curriculum will be guided by clinically relevant biomedical content from, among others, the
disciplines that have been traditionally titled anatomy, biochemistry, genetics, immunology, microbiology,
pathology, pharmacology, physiology, and public health sciences.
__________________________________________________________________________________
a. Describe the process used to ensure that the content taught in the preclinical phase of the curriculum
is appropriate and sufficient to prepare students for their clerkships.
At Einstein, this process occurs at three phases of our educational program: 1) at the pre-clerkship
course level; 2) at the clerkship level; and 3) at the level of the Executive Committee of the Medical
Education Council.
1. Pre-clerkship Courses:
Pre-clerkship courses prominently include clinicians who teach in the clerkship years and
practicing clinicians to teach first- and second-year students the clinical skills and the foundation
science necessary for their clerkships.
Introduction to Clinical Medicine (ICM): Clinical skills are predominantly taught in the
Introduction to the Patient course (year 1) and The Clinical Examination (year 2). The first-year
course focuses on the doctor-patient relationship. With patients and standardized patients
representing a wide range of disorders and ages, students practice, observe and assess their
performance in interviewing skills. In ICM-The Clinical Experience, first-year students are placed
in hospital and community clinics, private patient and in emergency room and other hospital
setting, observing interviewing, physical examination and procedure skills. The second-year course
focuses on the clinical exam. Throughout the course, students, in classroom and then hospital
settings, are taught the examination of pulmonary, cardiovascular, abdominal, ear, nose, throat,
musculoskeletal, geriatric and dermatological systems
Medical Histology and Cell Structure: In the Histology course, basic science is learned in the
context of human diseases. Lecturers connect abnormal structure and function to disease
mechanisms. In small group labs, students engage in case studies of histopathological bases of
multiple diseases. In addition, students must research specific diseases and present the
histopathological mechanisms to their peers.
Molecular and Cellular Foundations of Medicine (MCFM): Clinicians who teach and precept in
clerkships are instructors in this first-year course. These clinicians, who deliver lectures and
facilitate in small-group conferences, are aware of the demands on clerks and emphasize content
areas from MCFM foundation science that are most relevant to our clerks. Examples are lectures
on bilirubin metabolism and hypoglycemia in neonates and acid-base balance and conferences on
diabetic ketoacidosis, hypercholesterolemia and pernicious anemia. In addition, fourth-year
students who have completed their third-year clerkships serve as facilitators for MCFM
conferences on diabetic ketoacidosis, hypercholesterolemia and pernicious anemia. These fourthyear students frequently describe their encounters with patients who display the preceding
disorders and ensure that the content taught in first-year MCFM is appropriate and sufficient for
students in their clerkships.
ED-51
Albert Einstein College of Medicine
Academic Year 2014-2015
Clinical & Developmental Anatomy: During the Clinical and Developmental Anatomy course,
students observe evidence of surgeries and disease processes from their initial surface examination
of the cadaver, which is facilitated by clinicians participating as clinical anatomy attendings during
each dissection lab session. These consultations continue throughout the regional dissection of the
whole body and are of particular importance, since the presence of surgeons and pathologists in
each dissection laboratory permits the daily assessment and interpretation of anatomical findings
that are not normal anatomy. Other clinical contributions include regional conferences on medical
imaging/radiology given by the Radiology faculty and tableside demonstrations of common
emergency procedures, including tube thoracostomy and cricothyrotomy, performed by Emergency
Department physicians. Lectures presented by physicians address topics such as cardiothoracic
surgery, care of the spine, fetal heart development and defects, liver transplantation, endoscopic
examination of the GI tract and ultrasound in musculoskeletal diagnosis.
Hematology: Examples of laboratory exercises in the Hematology course that are applicable to the
practice of medicine and to acquiring and applying science to the health of individuals and
populations include: venipuncture and phlebotomy; universal precautions when drawing blood or
handling any body fluids; identification and recognition of normal and abnormal blood cells and
diagnosis of primary and secondary hematologic conditions by preparation and microscopic
examination of Wright-stained blood smears; review of images of normal and abnormal blood cells
from the on-line Hematology Course Image Bank; evaluation of red blood cell production by
preparation and microscopic examination of reticulocyte blood smears; preparation and
interpretation of erythrocyte sedimentation rates; manual performance and measurement of
hematocrits; interpretation of normal and abnormal Serum and Urine Protein Electrophoreses and
Serum and Urine Immune Electrophoreses; and interpretation of normal and abnormal results of
blood coagulation tests.
Microbiology & Infectious Disease: Examples of laboratory exercises in performed during six hours
of hands-on bench top experiences in the Microbiology-Infectious Disease course include best
practices and safe use of microbiological laboratory equipment, Gram staining of diverse
laboratory specimens, practical use of microscopes to observe pathogens after staining, plating of
microbes onto different laboratory agars, utilization of differential growth on sugars to identify
organisms, determination of antibiotic susceptibilities by disc diffusion methodologies, processing of
samples from nasal mucosa and gingival spaces, microscopic observation of bacteria, and
performing catalase, coagulase and other rapid tests.
All pre-clerkship courses include didactic instruction that provides the scientific foundation of the
practice of medicine. All courses have small-group activities that are case-based and directly
related to preparation for clerkships. A sample from many instances are conferences in the Renal
Physiology course on control of GFR, acid-base balance and sodium and water balance, in the
Rheumatology course cases on monoarthritis and polyarticular arthritis, in the GI/Liver course
case conferences on inflammatory bowel disease and diarrhea and on liver disease, in the
Endocrinology course, conferences on diabetes and thyroid disorders and in the Molecular and
Cellular Foundations of Medicine course, conferences on Rh incompatibility, Marfan syndrome,
familial hypercholesterolemia and pernicious anemia.
2. Clerkships:
Clinicians and clinician scientists teach in the clerkships, reinforcing basic science concepts in the
context of direct clinical applications to patient care. All faculty and non-faculty instructors in
clerkships are provided with the competencies of Einstein medical education as well as the goals
and objectives of the clerkships in which they teach. Each required clerkship has identified
ED-52
Albert Einstein College of Medicine
Academic Year 2014-2015
required Clinical Conditions and Procedures that the clerks are required to experience and log
during the course of the clerkship. The identification of required Clinical Conditions links the
students back to core disease topics they learned in the pre-clinical years. Basic science concepts are
then reviewed in several formats including discussion on rounds, student reading, clerkship
lectures, and clerkship preceptor sessions. In these ways, clerks are reminded of pre-clerkship
content they learned in different settings, essentially labeling these clerkship-relevant topics for
future retrieval in the clerkship arenas.
Some of many examples of such didactic presentations in clerkships are the following topics:
Pediatrics: immunization, congenital heart disease, genomic medicine, child abuse
Obstetrics/Gynecology: menopause, fetal heart rate, ectopic pregnancy, reproductive genetics
Medicine: acid/base balance, infectious disease, dermatology, explicit discussion of the basic science
underpinnings with preceptors for angina, anemia, diabetic retinopathy, HIV infection, and
development of multidrug resistance in tuberculosis.
Surgery: fluids electrolytes and nutrition, infections, burn management
3. The Executive Committee of the Medical Education Council:
The MEC Executive Committee reviews each course and clerkship as part of the “Phase 2”
evaluation process. At this time, the Executive Committee will engage in oversight of the
preparation for clerkships by the pre-clerkship curriculum.
Annually, the Committee reviews GQ data, such as the data shown below, to identify the
effectiveness of pre-clerkship education in preparing students for their clerkship rotations.
Disciplines in which there is a rating significantly below that of the rating for all schools are
addressed. For example, for the basic science disciplines of Pathology and Pharmacology, preclerkship course directors of the organ system courses, Cardiovascular System, Nervous System,
GI/Liver System, Pulmonary System and Renal System, are in discussions with course directors of
the Pathology/Disease Mechanisms and Pharmacology courses to increase coverage of clerkshiprelevant content in their didactic and small-group exercises in the organ system courses. For the
discipline of Behavioral Science, the first-year ICM and Nervous System and Human Behavior
course directors are identifying behavioral science content areas from the Step 1 exam for increased
coverage in their courses.
b. Include data from the most recent AAMC Medical School Graduation Questionnaire (GQ) or the
AAMC Canadian Graduation Questionnaire (CGQ) (for Canadian medical schools) on how well
instruction in the following basic science subjects was rated by respondents in preparing them for clinical
clerkship rotations:
ED-53
Albert Einstein College of Medicine
Academic Year 2014-2015
Basic Science Disciplines
% Rating Preparation
for Clinical Clerkship
Rotations as Excellent
or Good
National % Rating
Preparation for
Clinical Rotations as
Excellent or Good
58.5
70.2
75.6
89.4
87.5
76.3
74.2
92.7
66.7
61.0
69.9
87.5
80.8
82.8
86.6
77.7
90.4
83.7
Biochemistry
Genetics
Gross Anatomy
Immunology
Microbiology
Pathology
Pharmacology
Physiology
Behavioral Science
Data from 2014 GQ
c. Include data from the most recent AAMC GQ (Question 13) or AAMC CGQ on the percent of
respondents rating instruction in public health as inadequate, appropriate, and excessive.
Topic (list topic from
GQ or CGQ)
Instruction in Public
Health
Percent of respondents indicating that instruction was
Excessive
Appropriate
Inadequate
35.6
60.0
4.4
Data from 2014 GQ
Also see information for standards ED-5 and ED-10 and Required Courses and Clerkship Rotations (B.
Required Course Forms)
ED-54
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-12. The curriculum of a medical education program should include laboratory or
other practical opportunities for the direct application of the scientific method, accurate
observation of biomedical phenomena, and critical analysis of data.
Opportunities in the curriculum could include hands-on or simulated (e.g., computer-based) exercises in which
medical students either collect or use data to test and/or verify hypotheses or to address questions about biomedical
principles and/or phenomena. The medical education program should be able to identify the location in the
curriculum where such exercises occur, the specific intent of the exercises, and how the exercises contribute to the
objectives of the course and the ability to collect, analyze, and interpret data.
____________________________________________________________________________________
a. List the preclinical courses that include laboratory sessions where students collect and analyze data to
test and/or verify hypotheses or to address questions about biomedical principles and/or phenomena. Do
not include laboratory sessions where the main objective is to observe and/or identify.
First-year Courses: Medical Histology & Cell Structure, Clinical and Developmental Anatomy,
Epidemiology, Population Health and Evidence based Medicine 1 (EPHEM 2)
Second-year Courses: Microbiology and Infectious Disease, Hematology, Epidemiology, Population
Health and Evidence based Medicine 2 (EPHEM 2)
b. Provide examples of opportunities for medical students to participate in educational sessions (actual
or simulated) that involve the direct application of the scientific method; accurate observation of
biomedical phenomena; and the collection, analysis, and interpretation of scientific data.,
Medical Histology & Cell Structure: Several sessions for scientific analysis and for addressing
questions about biomedical principles occur in labs where cases are used together with
histopathology specimens. There are 6-8 problem-solving sessions each year. Students must apply
analytical approaches to identify the source of the specimens, describe the microscopic changes that
occurred, and describe how the microscopic changes may be involved in the mechanisms of the
disease.
Students are asked to apply biomedical principles to understand disease mechanisms by
researching an assigned disease, its symptoms, diagnosis, prognosis, treatment and
histopathological basis. This report is then presented orally to the class, followed by a Q/A period.
EPHEM 1 and 2: The objectives of EPHEM 1 and EPHEM 2 are to equip the students with the
skills required to be critical consumers of the medical literature. In the first-year course, students
are introduced to the science of preventive medicine and clinical research methods. The basic
methodology of epidemiology and biostatistics is introduced from the perspective of populationbased approaches to preventive medicine and public health/prevention. The application of
population-based evidence to the care of individual patients is introduced during the second-year
course, which builds on and develops the concepts introduced in the first year. In EPHEM 2,
students apply these skills to critically appraise the medical literature, interpret the results, and
apply them to the care of individual patients.
In both courses, students have the opportunity to apply concepts of epidemiology and basic
statistics to the interpretation of journal articles in small-group settings (n=18-20) with a faculty
facilitator. In EPHEM 1, each of six sessions focuses on a journal article. Sessions include aspects
of team-based learning, and case-discussions, as well as work in groups of 4-5 students on problem
ED-55
Albert Einstein College of Medicine
Academic Year 2014-2015
sets that involve interpretation of the data in the focus article. In EPHEM 2, there are nine casebased sessions integrated into the organ systems courses. Sessions are in small-group format (n=
18-20), and each is based on a problem set that involves interpretation of a journal article.
Microbiology and Infectious Diseases: Medical students are given multiple unknown microbes
(bacteria and fungi) that they must identify/characterize based on phenotypic, morphologic,
biochemical or molecular means. The unknowns are utilized in evaluating clinical vignettes that are
paradigms in infectious disease syndromes by applying the knowledge gained in the identification
process to multiple clinical cases/scenarios. There are six labs that are paired (two paired labs for
each: overview of microbiological methodologies, Gram positive bacteria, and Gram negative
bacteria; however, molecular diagnostics are included in the Gram positive and negative
laboratories, and antibiotic susceptibilities are also evaluated in the context of the sessions).
Hematology – Laboratory Sessions: The Hematology Course has three laboratory sessions in which
all students have their blood drawn by their partners and draw their partners’ blood. We do not
do experiments with the specimens, so we do not directly apply the scientific method to test
hypotheses. However, the students do perform actual laboratory procedures on their own blood
specimens, which qualify as direct applications of scientific method, or methods.
Using their own blood specimens, students make blood smears suitable for staining and microscopic
inspection. They stain their smears with Wright stain for general inspection of their blood cells as
we learn about normal blood cells, morphology and function, and then view their own blood under
actual (not virtual) microscopy. They stain their own blood smears with a reticulocyte stain, as
they learn the normal and pathologic biology of red blood cell production, and inspect their own
blood and again under actual microscopy perform reticulocyte counts to assess the adequacy of
their own erythropoiesis. The students use their own blood specimens to spin hematocrits; they
learn the value and limitations of using hematocrits to describe anemia, and they discuss true and
false erythrocytosis. The students also use their own blood specimens to perform erythrocyte
sedimentation rates (ESRs), as we discuss the mechanisms by which inflammation increases the
ESR, and the role of immunoglobulins in particular in determining ESR in health and disease. In
this session, actual serum protein electrophoresis gels and serum immunoelectrophoresis gels are
handed out for the students’ direct inspection of normal and abnormal patterns, including
monoclonal dysproteinemias.
Students perform one small-group session activity using very brief clinical summaries, and small
sets of CBC and other laboratory data to do a group mix and match of 12 cases of anemia; the
students also do a similar exercise matching very brief clinical scenarios of bleeding disorders with
sets of hemostasis laboratory test results to match the correct laboratory test outcome with the
appropriate clinical scenario.
Hematology – Case Conferences
There are three 2-hour clinical case conferences, covering Anemia, Hematologic Malignancies, and
Disorders of Hemostasis and Thrombosis. These sessions are devoted specifically to analysis and
interpretation of clinical and laboratory data, as necessary, and are part of the conference goals of
formulating diagnostic plans, differential diagnoses, and therapeutic regimens.
Each case begins with a clinical scenario and some introductory laboratory data, which are
interpreted to uncover the case’s pathophysiology and to compose a plan for further diagnostic
evaluation. Additional information is presented once or twice more during the detailed discussion
of mechanisms of disease, and comprehensive differential diagnoses are produced and analyzed,
ED-56
Albert Einstein College of Medicine
Academic Year 2014-2015
with their indicated therapies reviewed in detail. Finally, the last diagnostic data are presented and
the final diagnosis discussed.
In the first conference, students discuss three cases of Anemia, each of moderate complexity and of
different pathophysiology. In the second conference, students discuss a complex case of leukocytosis
and splenomegaly. And in the third conference, they discuss a complex case of thrombocytopenia,
coagulopathy, and bleeding.
ED-57
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-13. The curriculum of a medical education program must cover all organ systems, and
include the important aspects of preventive, acute, chronic, continuing, rehabilitative, and
end-of-life care.
____________________________________________________________________________________
a. Describe the means by which the medical school ensures that each aspect of clinical medicine
identified above is included in required courses and/or clerkships/clerkship rotations.
Einstein has developed a multifaceted approach for ensuring that all organ systems are covered and
that the important aspects of preventive, acute, chronic, continuing, and rehabilitative and end-oflife care are included in our educational program. All of these topics are addressed in each of the
clinical clerkships (see examples below), and selected topics are also addressed in the several of the
courses in the first two years.
Information from course and clerkship evaluations is reviewed in depth at the Evaluation Subcommittee, and strengths and areas that need strengthening are identified. These findings are
forwarded to the appropriate sub-committee, either the Course Directors for courses in the first
two years or the Clinical Directors Subcommittee for the clerkships in the clinical years. In these
sub-committees, there is a review by all directors of both content and areas for horizontal and
vertical integration. This two-pronged approach to the review allows for collaboration and input
by a broad range of faculty members involved in our educational program. Student representatives
also sit on all of these sub-committees and provide important feedback. Phase 2 of the evaluation
process, to begin in the 2014-2015 academic year, will provide a more in-depth approach and will
address longitudinal outcome measures as well as coverage of specific interdisciplinary content
areas.
All clerkship directors also review curriculum recommendation guidelines of their respective
national clerkship organizations and have developed specific objectives that provide appropriate
coverage of the organ systems and of these key clinical topics. In addition, the implementation of
the Einstein 203, the full list of medical conditions on the patient log for the entire clinical
curriculum, has provided another method for ensuring coverage of all organ systems.
b. Provide one or more examples of where in the curriculum the following are covered:
Selected examples of coverage of each of these areas within the medical education curriculum are
described below:
Preventive Care:
Introduction to Clinical Medicine – A didactic session focuses on behavioral change counseling.
First-year students have a pre-assignment to interview a patient about a behavior they are
considering changing and to find a social media website or app designed to help the patient with
the desired behavioral change. Students complete two role plays in small groups to practice
health behavior assessment.
Microbiology and Infectious Diseases - Important aspects of preventive care are covered both
in lecture and small-group case-based formats, including detailed interactive discussions on
vaccinations, prophylactic antimicrobial therapy, infection control, and antibiotic stewardship.
ED-58
Albert Einstein College of Medicine
Academic Year 2014-2015
Strategies aimed at specific diseases such as tuberculosis and sexually transmissible diseases are
also covered.
Geriatrics Clerkship – A didactic session is devoted to geriatric assessment highlighting specific
measures relating to fall prevention. Another session on the hazards of hospitalization includes
a discussion about prevention of complications such as delirium and urinary tract infections.
Patients, Doctors and Communities (PDC) – During a small-group session, students view
YouTube clips on motivational interviewing to promote heart-healthy behavior, discuss pros
and cons of differing techniques, and participate in role plays in small groups.
Pediatrics Clerkship – Small-group case discussions based on health supervision.
Neurology Clerkship – Didactic session on primary and secondary prevention of stroke by risk
factor modification.
Ambulatory Care Medicine – Each student completes a table addressing prevention/early
diagnosis of diabetic complications for at least two patients. Each module includes an
interactive lecture about diet, focusing mostly on diet in chronic disease.
Obstetrics/Gynecology Clerkship – Didactic session devoted to preconception care and
prevention of complication during pregnancy. Students participate in preventive care with
patients at prenatal visits.
Family Medicine Clerkship – All students are required to complete an online module and
participate in a team-based learning session on prevention covering such important areas as:
goals of prevention with reference to Healthy People 2020; the principles of health promotion
and disease prevention (including risk assessment, immunization, and screening) ; and
evidence-based recommendations and guidelines (e.g., USPSTF). In the clinical setting,
preventive care services based on age and risk stratification are routinely covered as part of the
regular health care maintenance. An OSCE on shared decision making provides the
opportunity for students to guide a simulated patient through a preventive care decision where
there are uncertain or conflicting guidelines.
Acute Care:
Neurology Clerkship- Students learn by clinical exposure and didactic lectures how to manage
many acute medical issues in Neurology, including treatment of status epilepticus, assessment
criteria for patient selection for IV TPA for acute stroke, management of raised intracranial
pressure, diagnosis and treatment of acute inflammatory demyelinating polyneuropathy
(Guillaine-Barre).
Radiology Clerkship – Students are taught to recognize many conditions that require acute
management, such as pneumothorax, pneumonia, and improper line placements on CXR.
Geriatrics Clerkship - Students follow patients in the inpatient setting and learn about the
evaluation and management of acute issues, including falls, syncope, delirium, and atypical
presentations of common diseases urinary tract infections, cellulitis, and pneumonia.
Pediatrics Clerkship - Didactic session at orientation of clerkship entitled “Approach to the
Acutely Ill Child.”
ED-59
Albert Einstein College of Medicine
Academic Year 2014-2015
Medicine Clerkship – Group OSCE covering indication for avoidance of antibiotics in upper
respiratory infection.
Obstetrics/Gynecology Clerkship – Didactic session on obstetrical emergencies and ruptured
ectopic pregnancies. Clinical exposure to a variety of acute care management scenarios,
including placental abruption, postpartum hemorrhage, and acute pelvic/abdominal pain.
Family Medicine Clerkship – Students are exposed to a wide variety of acute conditions in the
clinical setting and must learn how to recognize and manage the most commonly occurring
outpatient conditions. These include but are not limited to: abdominal pain, cough, dyspnea,
fever, and rash.
Chronic Care:
Medicine Clerkship- Group OSCE focusing on establishing a therapeutic alliance with a patient
with uncontrolled DM for ongoing diabetic management.
Neurology Clerkship: Students are exposed through lecture and clinical cases to the
management of many chronic conditions such as: epilepsy, hemiplegic stroke, multiple sclerosis,
Parkinson's disease, dementia, etc. Instruction includes strategies for treatment of chronic
conditions such as spasticity, chronic pain, prevention of late complications, and medical
management to prevent relapse.
Ambulatory Care Medicine—Small-group interactive case-based sessions highlight
the chronic care of patients with diabetes and hyperlipidemia.
Family Medicine Clerkship – All students are required to complete online modules
and team-based learning sessions on diabetes, hypertension and hyperlipidemia.
Principles of diagnosis, management, patient-centered care and health education are
covered. The importance of the patient-doctor relationship is emphasized.
Continuing Care:
Introduction to Clinical Medicine - Several small group sessions involve discussions about longterm continuity relationships between doctors and patients. The students have an assignment
to write a narrative reflection on what they observe of their preceptor's interactions with their
patients, and these are discussed in the small group.
Pediatrics Clerkship – Online CLIPP cases assigned on growth and development.
Radiology Clerkship – With respect to continuing care through a patient's lifetime, students are
taught about radiation safety and the concept of ALARA (As Low as Reasonably Achievable) to
minimize patients’ radiation exposure.
Medicine Sub-internship – Specific didactic session on components of a good sign-out to allow
with optimal ongoing care with caregiver transition and cross coverage.
Geriatrics Clerkship: Students have didactic sessions and clinical exposure covering homecare
and long-term care facilities. Students are observed while establishing a health care proxy.
ED-60
Albert Einstein College of Medicine
Academic Year 2014-2015
Family Medicine Clerkship – At each primary care site, students see the advantages of
providing continuous care and the effective therapeutic alliance that results from providing
care throughout the life cycle.
Obstetrics & Gynecology – Ongoing clinical care of patients throughout pregnancy and the
postpartum period. Students participate in sign-out of patients in labor from one team to
another.
Rehabilitative Care:
Nervous System & Human Behavior Course – Small-group case working through the diagnosis
and management of a ruptured aneurysm with discussion of both OT and PT needed for
rehabilitation, and a didactic session on rehabilitant needed for traumatic brain injury.
Neurology Clerkship - Depending on the site, students either follow patients on a specific neurorehabilitation ward or participate in consults from a rehabilitation service. Discussions with
social workers and PT/OT include such topics as issues of progress in rehabilitation and
appropriate placement.
Geriatrics Clerkship - Didactic sessions on the evaluation of function, sizing of assistive devices
(such as canes), management of gait disturbance and spinal cord disorders.
Ambulatory Care Medicine - Students practice the physical exam of the knee and the shoulder
and are taught some exercises useful in treating common maladies involving those joints.
Family Medicine Advanced Ambulatory Care – Students spend time with a family doctor
providing wound care in an interdisciplinary setting (with specialized nursing, dietitians,
vascular and general surgeons) to manage chronic wounds, minimize complications and
facilitate rehabilitative care.
End-of-life Care:
Introduction to Clinical Medicine: Half-day session on Grief and Loss. There is a lecture by a
grief counselor and medical educator followed by a video about a young physician who on
graduation from residency is diagnosed with terminal cancer. The film follows him and his
family with readings from the young man's diary and interviews with him and his family,
friends, colleagues, and clergy. The students then break into their small-groups to discuss the
film.
Nervous System & Human Behavior Course - Lecture on management of pain in a palliative
care setting. This session deals with the unique aspects of treating chronic pain in an end-of-life
setting, including a discussion of equianalgesic dosing, alternative routes of delivery of
analgesia, and the unique concerns for pain therapy at the end of life (e.g., co-morbidities, renal
function, liver function, venous access, etc.).
Bioethics 1- Session on Ethical Issues at the End of Life. The session begins with a 45-minute
lecture on fundamental ethical concepts in end-of-life care, such as advance directives,
surrogate decision making and palliative care. Students then meet in small groups with
bioethics facilitators for an hour of case-based discussion.
ED-61
Albert Einstein College of Medicine
Academic Year 2014-2015
Geriatrics - Students spend a half-day at a hospice and palliative care facility where they are
provided with a formal lecture and round with the palliative care team.
Medicine Sub-internship - OSCE involving discussion of treatment option for a patient with
end-stage renal disease who declines dialysis.
Ambulatory Care Medicine - Session focusing on an actual patient with advanced Alzheimer’s
disease and her proxy’s concern about whether to work up a probable cancer.
Family Medicine Clerkship – There is a one-hour didactic session on Palliative Care, followed
by one afternoon at a palliative care site interviewing a patient. An OSCE at the end of the
rotation assesses students’ communication skills around referral and explanation of palliative
care.
ED-62
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-14. The curriculum of a medical education program must include clinical experience in
primary care.
ED-16. The clinical experiences provided to medical students by a medical education
program must utilize both outpatient and inpatient settings.
______________________________________________________________________
The following questions relate to standards ED-14 and ED-16.
a. List each required clerkship (in Canada, clerkship rotation) that provides experiences in primary care,
including the number of weeks classified as primary care.
Third Year:
Family and Social Medicine Clerkship – all 4 weeks of the clerkship are primary care
Pediatrics Clerkship – 3 weeks out of the 7-week clerkship are primary care
Obstetrics and Gynecology Clerkship – 1 week of the 6-week clerkship is primary care
Fourth Year:
Ambulatory Care Selective – all students must take an ambulatory care clerkship in one of three
available rotations:
Ambulatory Medicine – 3 1/2 weeks out of the 4-week clerkship are primary care
Ambulatory Pediatrics - 3 weeks out of the 4-week clerkship are primary care
Advanced Ambulatory Family Medicine – all 4 weeks of the clerkship are primary care
b. List the required clerkships (in Canada, clerkship rotations) that do not include any required
ambulatory experiences.
Third Year:
Medicine Clerkship
Fourth Year:
All students must take one 8-week sub-internship in one of three available inpatient rotations:
Medicine
Pediatrics
Family Medicine
Beginning in the 2014-15 academic year, all students must take:
One 4-week “core sub-internship” in either:
Medicine
Pediatrics
Family Medicine
And one 4-week “selective sub-internship” in either:
Medicine
Pediatrics
Family Medicine
Obstetrics
Surgery
Also see information for standard ER-6 in Section V: Educational Resources and Required Courses and
Clerkship Rotations, Part A, item (A.).
ED-63
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-15. The curriculum of a medical education program must prepare students to enter
any field of graduate medical education and include content and clinical experiences
related to each phase of the human life cycle that will prepare students to recognize
wellness, determinants of health, and opportunities for health promotion; recognize and
interpret symptoms and signs of disease; develop differential diagnoses and treatment
plans; and assist patients in addressing health-related issues involving all organ systems.
It is expected that the curriculum will be guided by the contemporary content from and the clinical experiences
associated with, among others, the disciplines and related subspecialties that have traditionally been titled family
medicine, internal medicine, obstetrics and gynecology, pediatrics, preventive medicine, psychiatry, and surgery.
________________________________________________________________________________
a. Describe how the curriculum prepares students to recognize wellness, determinants of health, and
opportunities for health promotion. Include examples of where in the curriculum these topics are
addressed and how student achievement is assessed.
In the clinical years at Einstein, students are taught recognition of wellness, determinants of health,
and opportunities for health promotion in a number of clerkships. Most have stated objectives
related to these areas in their respective clerkship objectives.
For example, during the Obstetrics & Gynecology and Women’s Health Clerkship, students teach
patients about breast self-awareness, safe sex, contraception, and lactation. They are assessed in the
clinics and on post-partum rounds on their ability to speak to patients and teach them about these
areas. In addition, oral presentations and written notes are reviewed to ensure these topics have
been mentioned.
The Pediatrics Clerkship uses the COMSEP (Council on Medical Student Education in Pediatrics)
clinical problem sets to teach many of these topics. This collection of clinical vignettes is used at all
sites, specifically the units on Health Supervision, Growth and Development, Behavioral Problems,
Nutrition, Adolescent Care, and Newborn Care. Students are also required to complete online,
interactive cases (CLIPP-Computer Learning in Pediatrics Program), which include health
supervision cases. In addition students learn about wellness, health determinants and health
promotion during the 3-week outpatient portion of the clerkship, during which they see patients for
health maintenance and sick visits in general pediatrics clinics under direct supervision of faculty.
In the Ambulatory Medicine and Ambulatory Pediatrics rotations in the fourth year (students are
required to do one or the other), health promotion and wellness are routine topics taught around all
clinic visits in the general practices. Students are assessed in these areas through their oral case
presentations and written notes. Some specific examples for teaching related themes include an
interactive classroom session on nutrition/diet (wellness) and another conference on breast cancer
prevention/screening (determinants of health/health promotion) in the Ambulatory Medicine block.
On Ambulatory Pediatrics, students are directly observed examining newborns and counseling
mothers on the post-partum unit. Additionally, they work directly with nurses and patient care
technicians to learn the norms and practice techniques for routine screenings (anthropometrics,
vitals, BP, hearing/vision, development) and preventive procedures (immunizations).
During the 4-week Family Medicine Clerkship, there is a 2-hour team-based learning session is
devoted to health promotion, preceded by completion of an online module. In the clinical setting,
each student addresses wellness and health promotion as part of the required conditions (health
care maintenance) and required procedures (including counseling on anticipatory guidance, family
ED-64
Albert Einstein College of Medicine
Academic Year 2014-2015
planning, immunization, and nutrition/exercise). Each week, students are in their continuity clinical
sites for three and a half days; in the community setting for two half days and in didactic sessions
for a half day. Most students complete these requirements with live patients, but if this is not
feasible, online materials are substituted. As part of the required community project, students in
pairs are required to use publicly available data to establish the relationship between a communitywide health problem and social determinants of health, with a comparison to national figures.
Students are assessed as part of their final presentation, judged independently by three faculty
judges using the same grading rubric.
Across all clerkships, there is a specific competency on the Evaluation of Clinical Performance and
Professional Attributes form that assesses students’ skills in health promotion/disease prevention.
b. For U.S. medical schools, provide data in the following table from the most recent AAMC GQ
(Question 13) on respondents’ perceptions of the adequacy of instruction in the following areas:
Topic
Diagnosis of disease
Management of disease
Health maintenance
Disease prevention
Health determinants
Percent of respondents indicating that instruction was:
Inadequate
Appropriate
Excessive
4.4
95.6
0.0
8.2
91.8
0.0
7.5
88.1
4.5
7.5
91.8
0.7
17.9
81.3
0.7
Data from 2014 Graduation Questionnaire
For Canadian medical schools, provide data in the following table from the most recent AAMC CGQ on
respondents’ perceptions of the adequacy of instruction in the following areas:
Topic
Percent of respondents indicating that instruction was:
Inadequate
Appropriate
Excessive
Management of disease
Health promotion and
disease prevention
Determinants of health
including social
determinants
For Canadian medical schools, provide the percent of respondents to the AAMC CGQ who agree or
strongly agree that they have the knowledge and skills to:
% Strongly agree
and agree
(National %)
Develop a differential diagnosis
Develop an appropriate
management plan
ED-65
% of total students participating
in the survey
Albert Einstein College of Medicine
Academic Year 2014-2015
d. Describe how experiences in family medicine, internal medicine, obstetrics and gynecology,
pediatrics, preventive medicine, psychiatry, and surgery are provided. Are these experiences organized as
separate clerkships/clerkship rotations, as one or more integrated (longitudinal) clerkship rotations, or in
some other way?
Experiences in these core disciplines are provided through separate, stand alone, clerkships of
varying duration in the third year. The following are required clerkships for Einstein students:
Clerkship
Family Medicine
Internal Medicine
Obstetrics/Gynecology
Pediatrics
Psychiatry
Surgery
Duration
4 weeks
11 weeks
6 weeks
7 weeks
6 weeks
8 weeks
Preventive medicine is not a separate clerkship but is taught in all of these clerkships, as well as
during the required 4-week Ambulatory Care rotation in the fourth year.
Also see information for standards ED-5 and ED-10 and Required Clerkship Rotation Forms.
ED-66
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-17. Educational opportunities must be available in a medical education program in
multidisciplinary content areas (e.g., emergency medicine, geriatrics) and in the disciplines
that support general medical practice (e.g., diagnostic imaging, clinical pathology).
__________________________________________________________________________
List where in the curriculum the following subject areas are included (for example, as a separate
course/clerkship, as a curriculum thread) and provide the curriculum year(s) in which the subjects are
taught.
a. Emergency medicine
Students encounter and have experience in admitting and stabilizing patients who come to the ED
in essentially all required third-year clerkships. Examples of conditions include ectopic pregnancy
in the Ob/Gyn clerkship, transport of critically patients in the Family Medicine Clerkship and
ischemic heart disease in the Medicine Clerkship. Three dedicated emergency medicine electives
are offered in year 4.
http://www.einstein.yu.edu/education/student-affairs/registrar/default.aspx?id=42388
b. Geriatrics
A required two-week clerkship is in year 3.
http://www.einstein.yu.edu/departments/medicine/divisions/geriatrics/education/medical-studenteducation/geriatrics-clerkship.aspx
Many educational sessions in the first two years address geriatric topics. Examples include lectures
in dementia in Nervous System and Human Behavior, Osteoarthritis in the Rheumatology
(Musculoskeletal Diseases) course and case studies in which the patient is in the geriatric
population.
c. Diagnostic imaging/Radiology
Diagnostic imaging is introduced in conferences in Clinical and Developmental Anatomy in year 1
and extensively in organ system physiology courses in years 1 and 2. Radiology is a required thirdyear clerkship and is offered in nine electives for year 4.
http://www.einstein.yu.edu/education/student-affairs/registrar/visiting-students/elective-coursedescriptions/radiology.aspx
d. Clinical pathology
Clinical pathology is introduced in the first-year Histology and Cell Structure and in the Disease
Mechanisms courses in the first year.
Clinical pathology is also offered in ten electives for year 4.
http://www.einstein.yu.edu/education/student-affairs/registrar/visiting-students/elective-coursedescriptions/pathology.aspx
ED-67
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-17-A. The curriculum of a medical education program must introduce medical
students to the basic scientific and ethical principles of clinical and translational research;
including the ways in which such research is conducted, evaluated, explained to patients,
and applied to patient care.
The faculty of the medical education program should develop explicit learning objectives (knowledge, skills,
behaviors, and attitudes) to meet the requirements of this standard. One example of relevant objectives is contained
in Report IV of the AAMC's Medical School Objectives Project (Contemporary Issues in Medicine: Basic Science
and Clinical Research).
There are several ways in which the medical education program can meet the requirements of this standard. They
range from separate required coursework in the subject to the establishment of appropriate learning objectives and
instructional activities within existing patient-focused courses or clerkship rotations (e.g., discussing the application
of new knowledge from clinical research in bedside teaching activities, offering mentored projects, or conducting
journal club sessions in which medical students explore the development or application of clinical and translational
research).
______________________________________________________________________
a. List all required courses and clerkship rotations that include formal learning objectives that address
basic principles of clinical and translational research.
Year 1:
Molecular & Cellular Foundations of Medicine (MCFM)
Disease Mechanisms
Principles of Pharmacology
Bioethics 1
Year 2:
Hematology
Pulmonary System
Epidemiology, Population Health and Evidence-Based Medicine (EPHEM) 2
Year 3:
Medicine Clerkship
Pediatrics Clerkship
b. For each course and clerkship rotation listed, briefly summarize how student achievement of those
objectives is assessed.
Molecular & Cellular Foundations of Medicine (MCFM):
Student achievement is assessed by questions on multiple-choice examinations, which contribute to
the course grade. For an examination, students are assigned to read a translational research article
from the medical literature. Students are encouraged to discuss the article among themselves, but
there is no didactic or other discussion of the article in MCFM class or conferences. Exam questions
will typically show data from the article, in the form of graphs or tables, and ask the students what
conclusions can or cannot be drawn from the data. In addition, questions are asked about the
overall goal or translational objectives.
Disease Mechanisms:
ED-68
Albert Einstein College of Medicine
Academic Year 2014-2015
The Disease Mechanisms course introduces recent scientific advances in diagnoses and treatment.
In addition to material presented in lecture format, students are required to interpret clinical
research papers in the small-group sessions. Assessment is informal in the small groups, but
comprehension is demonstrated as the students are required to interpret the findings in
presentation to each other. Certain key objectives are included in the final exam.
Principles of Pharmacology:
Several formal objectives for the Principles of Pharmacology course involve clinical and
translational research. These are:
Summarize the drug development process and evaluate the risks and benefits of using newly
approved drugs.
Determine when it is necessary to make adjustments to the dose depending on patientspecific factors.
Relate knowledge of pharmacokinetics to clinical care.
Recognize the impact of drug toxicities on patient health.
List the types of adverse drug reactions and identify the patient-specific factors that can
increase the risk of these reactions.
Summarize the basis for rational prescribing, including selection of the appropriate drug
and dose for an individual patient.
These objectives are achieved through formal lectures, with 10-30 minutes of lecture time dedicated
to each of these objectives. The students’ achievement of these objectives is assessed by multiplechoice examinations (a midterm and a final). In addition, the course includes three small-group
sessions in which students discuss cases, many of which include the learning objectives listed above.
The faculty members who oversee these sessions provide immediate feedback to the students
regarding their achievement of the learning objectives.
Bioethics 1:
“Research Ethics Then & Now: Ethical Principles, Unresolved Problems” (lecture and small group
discussions)
Question from Bioethics 1 2012-13 Final Exam (essay)
You have finally completed your medical training (whew!). You are a physician scientist, and you
are working on a new form of gene therapy for hemochromatosis. You are ready to test the safety
and tolerability of this new gene therapy that you have developed in a clinical trial. A
pharmaceutical company approaches you and offers to partner with you on your research. Your
medical school enters into an agreement with the company, in which the company will own the
patent to the gene therapy. The school will get a 5% equity interest in the company, and you will
receive a 15% equity interest. The company would like you to serve as the principal investigator
for this trial.
1.
2.
3.
4.
5.
6.
7.
Define conflict of interest.
If you agree to serve as principal investigator, do you have a conflict of interest?
If so, what is the conflict of interest?
What is/are the primary interest (s)?
What is/are the secondary interest(s)?
What are some options for managing this situation?
Should you agree to serve as principal investigator for the trial? Defend your answer.
Question from Bioethics 1 2011-12 Final Exam (essay)
ED-69
Albert Einstein College of Medicine
Academic Year 2014-2015
The randomized, controlled trial is considered the “gold standard” in research design. In many
clinical trials, subjects in the control arm receive a placebo while those in the experimental arm
receive the study drug. Placebos controls are used even when an approved drug for that condition
exists outside the trial.
Some people argue that placebo controls are always unethical when an effective treatment exists
outside a clinical trial. Do you agree? Are there some types of studies in which placebo controls
would be ethically acceptable but other studies in which use of a placebo control would be
unethical? Justify your answer.
Hematology:
In Lecture 1, Introduction to Hematology and Introduction to Methods in Hematopathology, we
review methods in laboratory hematopathology, including flow cytometry, fluorescent in situ
hybridization (FISH), and molecular genetic methods, all of which are part of the standard
repertoire of translational research
In Lecture 7, Hereditary Hemolytic Anemias III: Sickle Cell Disease, we discuss current and future
therapeutic treatments and treatment strategies that make use of translational research
In Lecture 8, Acquired Hemolytic Anemias, we discuss a targeted therapy for Paroxysmal
Nocturnal Hemoglobinuria (PNH).
In Lecture 11, Stem Cell Disorders: Myeloproliferative Neoplasia (MPN) and Myelodysplastic
Syndromes (MDS) we discuss a targeted therapy for Paroxysmal Nocturnal Hemoglobinuria (PNH)
- eculizumab.
In Lecture 11, Stem Cell Disorders: Myeloproliferative Neoplasia (MPN) and Myelodysplastic
Syndromes (MDS) we discuss a targeted therapy for MPN - JAK2 inhibitors.
In Lecture 12, Myeloid Leukemias: Acute Myeloid Leukemia (AML) and Chronic Myelogenous
Leukemia (CML) we discuss a targeted therapies for CML – Tyrosine Kinase Inhibitors (TKIs).
In Lecture 16, Stem Cell Transplantation, the entire field is an example, or includes multiple
examples, of the applications of translational medicine, including prevention and treatment of graft
rejection, graft versus host disease, non-myeloablative conditioning, and non-HLA matched and
now haplo-identical allogeneic transplantation.
In Case Conference 2, A High WBC Count, the diagnoses and therapies considered include CML
and TKI therapy.
In Case Conference 3, Too Much Bleeding, the diagnoses and therapies considered include PNH
and eculizumab.
Pulmonary System:
The Pulmonary Systems course approaches this topic by providing examples of how translational
research has improved clinical practice (from lab to bedside). We do this generally in all of the
lectures that occur in January and February of the course. We provide specific examples in the
lectures on Asthma, COPD, Tobacco Cessation, Disaster Medicine lectures 1 and 2, Pulmonary
Embolism, Pediatric Lung Disease lectures
Epidemiology, Population Health, and Evidence-Based Medicine (EPHEM) 2:
ED-70
Albert Einstein College of Medicine
Academic Year 2014-2015
The following objectives in this course address the skills students need in order to read and
interpret clinical/translational research studies:
At the conclusion to this course, students are able to:
Interpret, use, and communicate measures of effect such as relative risk, relative risk
reduction, absolute risk reduction, and number needed to treat. (8 sessions)
Identify methodological difficulties of randomized trials used to evaluate complementary
and alternative therapies. (1 session)
Identify methodological issues and difficulties in the design and interpretation of active
control equivalence / non-inferiority trials. (1 session)
Identify both the limitations and advantages of observational studies and randomized trials
in the evaluation of screening strategies. (2 sessions)
Identify biases associated with the evaluation of screening strategies. (2 sessions)
Interpret diagnostic test results, and studies of diagnostic tests. (2 sessions)
Interpret the results of meta-analyses. (1 session)
Medicine Clerkship:
Objective: Continue to develop your skills in self-directed, lifelong learning including active reading
about medical diseases, identifying and utilizing high quality sources of information, critical
reading of the medical literature, application of evidence based medicine to patient care, and
utilization of technology to further patient care.
We assess the achievement of this objective with a formative evidenced-based medicine
presentation required of each student and evaluated by the site preceptor. Each student selects and
presents a paper detailing an original randomized, placebo-controlled, prospective study. The
student must evaluate the quality of the data and the application of the data to our patient
population to guide clinical treatment.
Pediatrics Clerkship:
Students are exposed to basic principles of clinical and translational research in two orientation
lectures: 1) From the Bench to the Bedside-Translational Research in Pediatrics and 2) Genomic
Pediatrics- The Future is Now. In addition, they can apply this knowledge in the “Molecular
Science” section of their two required patient write-ups in which students are expected to research
and explain an aspect of a clinical condition on their differential diagnosis at the molecular, cellular
or genetic level.
c. Briefly describe any required courses or clerkship rotations in which students are routinely exposed
to, or have the opportunity to apply, basic principles of clinical and translational research, even if there
are no formal objectives for such learning.
Disease Mechanisms:
ED-71
Albert Einstein College of Medicine
Academic Year 2014-2015
The papers presented in small-group case conferences allow students to acquire and share basic
principles of translational research. These include an introduction to epidemiology and laboratory
medicine.
Renal System – In this course, students discuss several recent findings from basic science and the
potential future application to clinical care, including the discovery of anti-phospholipase A2
receptor as the target antigen in idiopathic membranous nephropathy and the discovery of APOL1
risk alleles for development and progression of CKD in African-American patients.
Nervous System & Human Behavior – The current clinical and/or research findings are discussed
for several neurologic conditions including seizure disorders, pain management, autism, bipolar
disorders and Alzheimer’s disease. In several cases, the history of the key clinical trials, possible
flaws in the analysis and the strength of the findings are critically discussed. Examples include the
review of the evidence and side effects of Cox-2 inhibitors for pain and beta amyloid inhibitors for
Alzheimer’s disease.
EPHEM 2 – In this course, students learn how to read, evaluate, interpret clinical research results,
and how to apply and to explain these results to individual patients. Topics covered include
randomized trials of screening and therapy; principles of diagnostic testing and screening; metaanalysis; and non-inferiority trials.
ED-72
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-18. The curriculum of a medical education program must include elective
opportunities to supplement required courses and clerkship rotations.
Although electives permit medical students to gain exposure to and deepen their understanding of medical
specialties reflecting their career interests, they should also provide opportunities for medical students to pursue
individual academic interests.
_________________________________________________________________________________
a. Indicate the number of weeks of elective time that are expected of all medical students in each year of
the curriculum:
Year
Total Weeks of Elective Time
1
0
2
0
3
0
4
20
b. Indicate the maximum number of weeks that students may spend taking electives at another
institution that is not part of the medical school’s health system or affiliated with the medical school.
No
maximum
c. Provide the average number of weeks that students in the most recent graduating class spent taking
electives at another institution.
8
d. Describe any policies or practices that require or encourage students to use electives to pursue
interests outside of their chosen specialty.
There is no specific policy requiring or encouraging students to pursue electives outside their area
of career choice. Supervision of electives is individualized to maximize students’ career advisory
opportunities, fulfill their requirements, and help them meet their own educational needs. As such,
students have personal meetings with the deans for students and designated faculty advisors, as well
as with the Registrar to schedule the actual rotations. Students are informed about elective
opportunities via the Web, email communications, and mandatory class meetings specific to senior
year planning and registration, and specialty specific career nights held throughout the year. In
addition to approval by the Office of Student Affairs, students are encouraged to discuss their
elective selections with their faculty advisors. (See MS-20.)
e. Indicate whether the medical school has a policy that specifies a maximum number of electives (or
elective weeks) that students may take in the same specialty area, either at the medical school or at
another institution. [For Canadian medical schools, note whether the school follows the AFMC
UGME/PGME Policy on Diversification of Electives.]
While there is no policy specifying the maximum number of electives students may take in the same
specialty area, the student affairs deans meet individually with all fourth-year students to advise
them on choice of electives.
If a policy is in place, include an electronic copy in the Appendix and describe how the requirements of
the policy are enforced.
N/A
ED-73
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-19. The curriculum of a medical education program must include specific instruction
in communication skills as they relate to physician responsibilities, including
communication with patients and their families, colleagues, and other health professionals.
________________________________________________________________________________
Describe where in the curriculum (i.e., specific course[s] or clerkship rotation[s]) students gain experience
in the following areas. Specify the settings in which instruction occurs (e.g., classroom, clinical setting,
simulated setting) and the format(s) used (e.g., lecture, small group, standardized patient, role play).
a. Communicating with patients and patients’ families
Introduction to Clinical Medicine (ICM):
In the ICM program during their first and second years, students receive extensive teaching and
practice of communication with patients. For the Introduction to the Patient course, first-year
students meet every Wednesday afternoon from September through March in small groups with
faculty. Each week has a different theme and is accompanied by skills training and practice. Many
of the sessions take place in our Clinical Skills Center, where students interview both real and
standardized patients as well as utilize role play. Some sessions involve travel to a clinical site
where students interview both medical and psychiatric hospitalized patients.
In addition, on Monday afternoons (The Clinical Experience), the students travel to a clinical site to
which they have been assigned for the year. There they meet with their clinical preceptor who will
observe them interviewing patients and give them feedback. Depending on the site and specialty,
student-to-faculty ratio varies from 1:1 to 4:1. At their clinical sites, many students will have the
opportunity to communicate with the patients’ families as well.
In the second-year course, The Clinical Examination, one session focuses on communicating with
families. We recruit family members, many of whom have chronically ill children, who come in and
meet with each small group. The students will hear the stories of their interactions with the
healthcare system and will practice interviewing the family.
In the second year from January to April on Tuesday afternoons, students travel to clinical sites
where they are observed by faculty preceptors doing histories and physical exams on patients either
in the emergency room or on the hospital ward. The student-to-faculty ratio for this course is 4:1.
Patients Doctors and Communities (PDC):
PDC is a third-year seminar-like course where students are both asked to reflect on and critique
their clerkship encounters where communication skills are inherent and linked to patient
satisfaction and efficiency of care. We also have the opportunity to simulate encounters where there
is a communication that is difficult, in order to help students to build their skills and confidence.
In PDC, communication with patients and their families is both reflected upon and practiced. For
the following sessions, the students are given reading materials, write a reflection essay or critique
of a patient encounter, and discuss the barriers to effective communication in the small group.
Teams: (During Introduction to the Clerkships Day); Professionalism (session #1); Difficult DoctorPatient Encounters (session #3); Behavior Change (session #5); Goals of Care (session #6).
ED-74
Albert Einstein College of Medicine
Academic Year 2014-2015
Although not specifically an objective of the session, communication with patients and patients
families is routinely the object of discussion when health care outcomes and patient safety are
discussed during the following sessions: Team and Teamwork: Improving Patient Safety/Improving
Outcomes (session #9) and Medical Errors & Patient Safety: Quality Improvement (session #8).
Communication skills are practiced in the small-group session utilizing simulated exercises during
the following sessions: Shared Decision Making/Informed Consent (session #4) and Communicating
Bad News (session #7).
b. Communicating with physicians (e.g., as part of the medical team)
Introduction to Clinical Medicine (ICM):
The first-year ICM course includes a session on “Communicating with Colleagues.” Students learn
and practice the skills of presenting cases, and this skill is reinforced and further practiced on the
medical ward visits in the Wednesday course and at the clinical sites on Mondays. Students also
receive instruction on the standard case write-up format used in communicating with colleagues.
They have several required case write-ups on patients they have interviewed in class or at the
bedside and receive extensive written feedback from faculty.
Patients, Doctors & Communities:
Sessions include: Teams (During Introduction to the Clerkships); Professionalism (session #1);
Team and Teamwork: Improving Patient Safety/ Improving Outcomes (session #9) and Medical
Errors & Patient Safety: Quality Improvement (session #8). In addition, the session on the Health
Care System includes a discussion about the patients’ medical home and communication with
healthcare providers utilizing information systems.
c. Communicating with non-physician health professionals and members of the health care team
Introduction to Clinical Medicine (ICM):
During both first-year and second-year ICM courses, students communicate with non-physician
health professionals at their clinical sites.
Patients, Doctors & Communities:
The following sessions discuss communication with non-physician members of the health care team:
Teams (During Introduction to the Clerkships Day); Professionalism (session #1); Team and
Teamwork: Improving Patient Safety/Improving Outcomes (session #9) and Medical Errors &
Patient Safety: Quality Improvement (session #8).
Also see information for standards ED-10 and ED-28.
ED-75
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-19-A The core curriculum of a medical education program must prepare medical
students to function collaboratively on health care teams that include health professionals
from other disciplines as they provide coordinated services to patients. These curricular
experiences include practitioners and/or students from other health professions.
_____________________________________________________________________________
a. Provide several examples of required experiences where medical students are brought together with
students or practitioners from other health professions to learn to function collaboratively on health care
teams with the goal of providing coordinated services to patients. For each example, describe:
1) the objectives of the experience related to the development of collaborative practice skills;
2) the year in the medical curriculum where the experience occurs;
3) the setting, such as a clinic, simulation center;
4) the other health professions students or practitioners involved; and
5) the way(s) that the medical students’ attainment of the objectives of the experience is assessed.
All Clerkships: Einstein Educational Competency – “Physician as Colleague”
1. Objectives (Examples from three clerkships):
Students will –
Medicine Clerkship: “Communicate clearly with all members of the care team including
physicians, nurses, physical therapists, nutritionist, social workers, and support staff.
Communication skills include oral communication in person, on the phone, and via clearly
written, legible daily progress notes.”
Family Medicine Sub-internship: “Communicate clearly with all members of the health care
team and ancillary staff (including end of day and end of service coverage) to ensure the
optimum care of the patient.”
Pediatrics Clerkship: “Establish productive, respectful working relationships with all health
team members.” “Illustrate the role that pediatricians and other health professionals play as
advocates for children.”
2. Year:
In all third- and fourth-year required rotations, working effectively and collegially with
members of other health professions to promote positive patient health outcomes is stated as a
concrete student responsibility.
From the Medicine clerkship student manual: “Nursing staff is responsible for directly
delivering much of the patient care and for managing the unit. There is much the nursing staff
can teach students about how the hospital functions and how to care for patients. Introduce
yourself and get to know the nursing manager and staff by name. Be courteous and collegial,
never bossy or condescending. Other hospital staff such as social workers, technicians,
dieticians, and building service personnel all deserves friendly, respectful treatment as well.
Your ability to interact successfully with all members of the health care team forms part of the
final evaluation of the clerkship.”
3. Setting:
All clerkships have an ambulatory and inpatient component except Family Medicine,
Advanced Ambulatory Family Medicine, Ambulatory Pediatrics, and Ambulatory Medicine,
ED-76
Albert Einstein College of Medicine
Academic Year 2014-2015
which are all outpatient settings. The Medicine clerkship and all required sub-internships are
inpatient.
4. Health Professions:
Students work as part of a health care team in inpatient and ambulatory settings. Depending
on the setting, students work with a full spectrum of inter-professional members including
nurses, physician assistants, midwives, nursing assistants, patient care technicians, clerical
staff, referral coordinators, social workers, nutritionists, specialists and generalists, residents
and peer students.
5. Assessment of Student Attainment of Objectives:
On every clerkship and required sub-internship, students are evaluated by site directors and
clerkship directors on the following criteria: “RELATIONSHIP WITH CLINICAL STAFF /
TEAMWORK SKILLS: Establishes productive, respectful working relationships with all
health team members.” Site directors formulate their score for this competency by polling all
members of a health care team as appropriate. An “outstanding” score on this objective means
the student can “integrate smoothly and productively with the entire clinical team. Takes
exceptional initiative to contribute to the work and education of the team”.
Family and Social Medicine Clerkship: Community Health Project
1. Objectives:
Students will Create, implement, and evaluate community-oriented health interventions.
Communicate effectively with community partners, advocates and agencies.
Demonstrate effective communication with patients, families, and communities that takes into
account socioeconomic status, cultural background, and health literacy.
2. Year:
During the four-week Family and Social Medicine clerkship, third year students participate for
two half-days per week in a community-based service learning health project. This project
requires students, working in teams, to define and analyze a health problem in a specific
population.
3. Setting:
Teams work in existing community-based programs to develop brief health education
interventions to address an identified need. These programs include community centers, public
schools, community support groups, and community-based health centers.
4. Health Professions:
Students are assigned to community project site advisors who are community agency staff,
social workers, schoolteachers or administrators, and community health educators. These
advisors supervise the students’ projects at the community-based program.
5. Assessment of Student Attainment of Objectives:
Student performance on the community projects is worth 20% of the clerkship grade.
The project culminates in an oral presentation to the entire group of students, faculty, and
invited community members and faculty guests. The project presentation is assessed on a
ED-77
Albert Einstein College of Medicine
Academic Year 2014-2015
number of criteria, which includes several of the objectives for the experience. Faculty
assessment of the project presentation contributes to the clerkship grade.
All students are assessed by their community project site advisor on several criteria of which
some include:
1. Effective communication with community partners, advocates and agencies
2. Exhibiting dependability
3. Exhibiting commitment to the community projects
Microbiology and Infectious Diseases Course: Collaborative Practice between Physicians and
Microbiologists
1. Objective:
Accurately describe the roles, responsibilities and scopes of practice of clinical microbiologists.
2. Year:
This experience, which occurs in the second year Microbiology course, is related to the
development of collaborative practice skills. The participating microbiologists will describe
their roles, responsibility and scope of practice in contributing to positive health
outcomes. Additionally, the MD clinical microbiologists will share their career pathway into
their laboratory director positions. All involved will describe aspects of and opportunities in
laboratory medicine as a career.
3. Setting:
Hands-on laboratory session.
4. Health Professions:
Clinical microbiologists with degrees including MS, PhD and MD
5. Assessment of Student Attainment of Objectives:
There will be a minimum of 1 multiple-choice question evaluating aspects of interactive
collaboration between clinicians caring for a patient and a clinical microbiologist. Effective
patient care requires coordinated efforts between clinicians with direct patient interactions and
healthcare professionals providing laboratory assessments on diverse clinical samples. The
clinical microbiology laboratory provides support for patients with potential infectious
diseases. Appropriate coordination between clinicians and the clinical microbiologists increases
the appropriateness of testing (i.e., making sure that specimens are obtained appropriately
[such as what to collect samples in, how much sample is needed {i.e., volume of blood added to
blood cultures}, and how samples need to be maintained prior to arrival in the laboratory or
how much time can elapse for the samples to be useful) and the clinicians need to inform the
laboratory of what diseases they are suspecting to make sure that the samples are
appropriately tested as well as making sure that potential biological risks to the staff of the
laboratory are minimized.
Molecular and Cellular Foundations of Medicine course, Unit 3 “Cancer and Cell Growth”
1. Objectives:
To discuss ethical and counseling issues related to cancer genetic testing
To become exposed to different viewpoints on ethical and genetic counseling issues.
To become aware of the critical issues that enters into genetic counseling.
To accurately describe the roles, responsibilities and scopes of practice of genetic counselors.
ED-78
Albert Einstein College of Medicine
Academic Year 2014-2015
To utilize the scope of knowledge, skills and abilities of genetic counselors to provide care that
is safe, timely, efficient, effective, equitable and cost-effective, when appropriate.
2. Year:
Clinical genetics is a content area of MCFM Unit 3, with an explicit goal of teaching about
screening for mutations that lead to cancer predispositions and genetic counseling.
3. Setting:
Screening and counseling for BRCA mutations is the major example, presented to first year
students in a didactic lecture by a medical geneticist and small group conferences in which the
first year class is divided into eight groups. Each group is led by genetic counselors working at
Einstein hospital and our affiliates or by physicians who practice genetic counseling. The
conference room setting for the small group conferences includes video clips of persons who are
or have been counseled and of genetic counselors in counseling sessions. Our current conference
uses clips from the film, “In the Family” by Joanna Rudnick.
4. Health Professions:
In addition to trained genetic counselors, 1-2 of the conference groups will also include as an
observer a genetic counseling student from the Sarah Lawrence College program in genetic
counseling, where Einstein faculty teach.
5. Assessment of Student Attainment of Objectives:
Students are assessed in their grasp of genetic counseling in the context of breast/ovarian cancer
by multiple-choice questions on the Unit 3 exam. A typical Unit 3 exam of 62-65 questions
includes three questions that directly assess students in the principles of genetic counseling.
b. In the Appendix, include electronic copies of forms used in the assessment of medical students’
collaborative practice skills. See ED Appendix J for the following tools:
1. Assessment tools on student performance for the Family and Social Medicine clerkship’s
community-based health project;
2. Pre-clinical Professionalism Evaluation Tool (used by lab groups in special session during the
Anatomy course; results shared within each group and not with course directors);
3. Evaluation of student performance on clerkships on “Physician as Colleague” competencies.
c. Describe how the objectives related to collaborative practice skills are linked to the objectives of the
medical education program.
In August 2013, the Executive Committee charged a working group entitled the Population Health
and the Practice of Medicine (PHPM) Working Group with the goal of developing a new
longitudinal thematic program focused on enhancing the behavioral and socioeconomic education
of our medical students in courses and clerkships. One specific task of this working group was the
establishment of new learning objectives related to “Interprofessional (IP) Team Health Care and
Training.” The PHPM working group mapped each new IP learning objective to Einstein
competencies. These competency-based learning objectives will serve as the foundation for this new
integrated curriculum, which will begin in the 2014-15 academic year.
Einstein Competencies
ED-79
X
X
Life-long
Learner
Colleagu
e
Role
Model
Effectively describe their own role, responsibilities, and
scope of practice to patients, families and other
professionals.
Accurately describe the roles, responsibilities and
scopes of practice of other professionals.
Demonstrate recognition of one’s own limitations in
skills, knowledge and abilities.
Utilize the scope of knowledge, skills and abilities of
available health professionals to provide care that is
safe, timely, efficient, effective, equitable and costeffective, when appropriate.
Place the interest of patients and populations at the
center of IP health care team delivery.
Recognize how one’s own uniqueness and that of other
team members, including power and hierarchy within
an IP team may contribute to effective communication
and IP tension.
Contribute to effective and respectful IP
communication including giving and receiving clear
feedback, addressing conflict or differences in opinions,
and self-reflection.
Develop a trusting relationship with patients, families
and team members.
Describe IP practice theory with respect to the
teamwork.
Describe the context and culture of IP environment that
that facilitates and inhibits collaboration.
Identify instances where IP care will improve patient
and family health outcomes.
Participate in effective decision-making in IP teamwork
utilizing judgment and critical thinking to optimize
health outcomes and safety.
Contribute to team effectiveness through reflection on
IP team function.
Demonstrate openness to utilize effective IP
communication skills.
Identify IP ethical issues within a team context.
Reflect on own personal and professional values.
Demonstrate respect for the personal and professional
values of other IP team members, patients and families.
Guided by an ethics framework, contribute to IP
ethical reasoning and decision-making in order to
maximize quality and patient safety.
Educator
Advocate
Inter-professional (IP) Team Health Care and Training
Learning Objectives
Scientist
Academic Year 2014-2015
Healer
Albert Einstein College of Medicine
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
See ED Appendix K for a working draft of a curriculum map for Inter-professional (IP) Team Care
and Training.
ED-80
Albert Einstein College of Medicine
Academic Year 2014-2015
In order to promote further integration of inter-professional team training in medical education,
the 2014 Annual Clerkship Retreat was planned around this subject. This took place on May 29,
2014 (See Agenda, ED Appendix L). The guest speaker was Dr. Jo Ivey Boufford, president of The
New York Academy of Medicine, who spoke to clerkship directors, site directors and faculty on the
critical importance of inter-professional education in the health professions. All required clerkships
have been asked to design and implement new instructional sessions and assessments on interprofessional team health care and training based on the IP learning objectives set by the PHPM
Working Group.
ED-81
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-20. The curriculum of a medical education program must prepare medical students for
their role in addressing the medical consequences of common societal problems (e.g.,
provide instruction in the diagnosis, prevention, appropriate reporting, and treatment of
violence and abuse).
____________________________________________________________________________________
a. Indicate where in the curriculum students learn about the medical consequences of common societal
problems.
Introduction to Clinical Medicine: Introduction to the Patient:
The first-year ICM curriculum places considerable emphasis on helping students appreciate the
social, economic, cultural and other systemic effects on health, well-being, disease and illness.
Many class sessions (2.5 hours) are structured to focus on societal influences that impact health and
healthcare delivery, and students are encouraged to consider the social determinants related to
illness and poor outcomes. The following is a list of some related sessions.
1. HIV as a Paradigm for Chronic Illness – In each small group, students practice interviewing
patients from the local Bronx community with HIV+ diagnoses. The medical histories of these
patients highlight gaps and disparities in care and the social histories are often infused with
elements of extensive drug abuse, violence, incarceration and poverty.
2. What Makes a Patient Unique? – Each group watches a documentary-style video that portrays
difficulties and inadequate care resulting from religious, cultural, language barriers and probable
bias and stereotyping. The video is used as a trigger for a wide-ranging discussion. The session
also includes a role-play encounter with a simulated patient portraying an immigrant with
language, health literacy and cultural issues whose explanatory model produces long-standing
adherence complications. Students are challenged to tease out some of the root causes of the nonadherence.
3. Medical and Psychiatric Ward Visits – Students practice patient interviewing at the bedside and
experience firsthand the consequences or exacerbations of preventable conditions.
4. Health Behavior Change – Students interview patients about health behaviors that could be
changed as a pre-assignment, and then role play scenarios of patients who smoke and drink alcohol.
5. Communication Challenges – As described in ED-21, students interview patients with extensive
substance abuse histories that are often accompanied by histories of violence, criminality and
incarcerations.
6. Sexuality Workshops/Violence Workshops – Students attend workshops facilitated by faculty
with expertise in these topic areas, which encompass a range of issues related to societal problems.
Family Medicine Clerkship:
During the clerkship, all students are required to complete a community project, where identify the
social factors that contribute to health problems and design and implement a health education
intervention to address prevention of the problem. Unless exempt by religious observance, students
are also required to work two Saturdays at the student-run free clinic, which provides medical care
to the uninsured. They see firsthand the difficulties encountered by their patients, many of whom
are undocumented immigrants or the working poor who cannot afford insurance. The students
share the patients’ frustration as they try to get the patients needed medications or specialty
ED-82
Albert Einstein College of Medicine
Academic Year 2014-2015
referrals. They see the consequences of allowing a medical condition to get worse before seeking
medical help, or not having the timely follow-up once an illness is diagnosed. One of the required
didactic seminars during the Family Medicine clerkship is on Intimate Partner Violence (IPV),
including how to assess and help patients. In one of the required team-based learning sessions, the
preparatory online module includes information about screening for IPV; in another session, there
is a discussion about barriers to medical care, including financial constraints and the effects of low
health literacy.
Patients, Doctors & Communities (PDC):
Two of the societal problems that students are exposed to during their clerkships in the Bronx are
access to health care and the impact of homelessness on safe discharge and continuity of care.
Students are asked to consider what methods of advocacy they might engage in, individually and
through systems approaches, to aid in the betterment of health in our patient population. Often
students feel powerless dealing with the bureaucracy until suggested strategies for advocacy are
made by small-group members. This does not automatically translate into the provision of shelter
for the homeless patient with medical needs who continues to utilize in-hospital resources, but it
does raise awareness of the need to address more than the emergent health problem in patients who
do not have access to outpatient health care.
PDC also directly explores the community’s access to health care in the session on the health care
system. Health insurance, access to care, cost and quality of care are the focus of the session.
Pediatrics Clerkship:
At each Pediatrics Clerkship orientation, students are given a lecture on child abuse by a board
certified child abuse pediatrician. Topics covered include the history, epidemiology, definition,
evaluation and reporting of child abuse. Both physical abuse and sexual abuse are discussed.
Students are informed of their mandated reporter status.
Geriatrics Clerkship:
During the Geriatrics Clerkship the students receive a didactic session on Elder Abuse and
Mistreatment. They learn to identify different forms of mistreatment by identifying red flags from
both the history and the physical exam. The students learn to perform and document an assessment
of mistreatment, learn techniques for successful interviews, and review resources available for
reporting cases of elder abuse.
b. List the required courses and clerkship rotations in which the following aspects of domestic violence
and abuse are covered (see Glossary at the front of this section for definitions).
Content Area
Diagnosis
Prevention
Reporting
Required Course(s) in which
Topic is Addressed
Introduction to Clinical
Medicine
Introduction to Clinical
Medicine
Introduction to Clinical
Medicine
Treatment
ED-83
Required Clerkship Rotation(s)
in which Topic is Addressed
Family Medicine
Pediatrics
Geriatrics
Family Medicine
Geriatrics
Family Medicine
Pediatrics
Geriatrics
Geriatrics
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-21. The faculty and medical students of a medical education program must
demonstrate an understanding of the manner in which people of diverse cultures and belief
systems perceive health and illness and respond to various symptoms, diseases, and
treatments.
Instruction in the medical education program should stress the need for medical students to be concerned with the
total medical needs of their patients and the effects that social and cultural circumstances have on patients’ health.
To demonstrate compliance with this standard, the medical education program should be able to document
objectives relating to the development of skills in cultural competence, indicate the location in the curriculum where
medical students are exposed to such material, and demonstrate the extent to which the objectives are being
achieved.
________________________________________________________________________________
a. List the courses and clerkship rotations in which all students learn about issues related to cultural
competence in health care and describe the specific elements related to cultural competence that are
covered in each.
Introduction to Clinical Medicine: Introduction to the Patient:
In this course there is a session devoted to the following elements related to cultural competence:
health belief model, cultural and religious elements of healthcare, health literacy, patients’ use of
traditional/complementary and alternative medicine. In a small-group session, we use both a
videotaped case of a Muslim man undergoing treatment for cancer, which focuses on his health
beliefs and those of his family, as well as a role play of a Latina patient whose medication nonadherence involves issues of health literacy, health explanatory model, and the use of traditional
medications.
Another session, “Communication Challenges” emphasizes issues of diversity and incorporates
both simulated and actual patient encounters in the classrooms. Actors play simulated patients with
sexual chief complaints. The cases involve a male patient who identifies as bi-sexual and reports a
recent history of sex with men, and a female patient who self-identifies as straight but has a past
history of sex with a woman. Discussion about differences, biases and disparities follow the role
play. Actual patients interviewed in this session have long-standing poly-substance abuse histories.
The sociocultural, class, ethnic and other issues raised in these encounters add to the discussion of
diversity.
In addition to these sessions, throughout the course we utilize a Communication Skills Checklist for
both teaching and assessment purposes. It is used to guide feedback for all sessions. Shown below is
the item on that checklist that addresses cross-cultural communication skills.
Cross-cultural Communication Skills
Elicits and is
respectful of
patient’s
healing
traditions,
health beliefs
& practices
Does
Not
Employ
Does not elicit
and/or fails to
respect patient’s
traditional/cultural
health beliefs &
practices
Partially
Employs
May elicit but does not
fully explore cultural
healing traditions &
practices. Inconsistently
respectful of
beliefs/practices.
ED-84
Consistently
Employs
Fully explores and is consistently
respectful of patient’s traditional/cultural
healing traditions & practices
Albert Einstein College of Medicine
Academic Year 2014-2015
Family Medicine Clerkship:
The students see a very diverse patient population at their Family Medicine clinical sites. The
patients come from different ethnic and cultural backgrounds, and students learn from their
clinical preceptors about the importance of respecting the patients’ beliefs and values to form an
effective therapeutic relationship. Incorporating the patients’ preferences and negotiating mutually
acceptable treatment plans are important to ensure adherence and provide the optimal care.
We introduce the students to the ETHNIC (explanation, treatment, healers, negotiation,
incorporation, collaboration) framework during one of the team-based learning sessions, and
discuss how to incorporate this framework in formulating a culturally sensitive and patientcentered management plan. Cultural differences are also discussed as they pertain to the patients’
and families’ understanding of their illness and its management.
Patients, Doctors & Communities (PDC):
Many of the interview and communication skills that are reflected upon and practiced in PDC
involve the patient’s perspective of his/her illness; specific learning objectives are included in the
PDC sessions on: professional attributes; shared decision making/informed consent; behavior
change; goals of care and communicating bad news. Identifying the patient’s perspective and values
are of paramount importance in the student’s attitude and knowledge regarding these topics and is
very much expressed in the communication skill acquisition. Although it is a general consideration
rather than being consistent with cultural or religious beliefs, the importance of the patient’s values
in the decisions involving medical care is foundational to cultural competence.
b. Indicate the means by which students’ acquisition of the knowledge, skills, behaviors, and attitudes
related to cultural competence is assessed.
Introduction to Clinical Medicine: Introduction to the Patient:
The students are assessed twice during the first year using a videotaped interview with a
standardized patient (SP). The simulated/standardized patients complete the communication skills
checklist on the students, which includes an item evaluating the students’ ability to address their
concerns in the context of their lives, including their health beliefs.
One of the standardized patient (SP) cases used in the student evaluations portrays an
undocumented immigrant seeking health care with a variety of social, cultural and economic
factors that highlight the interplay between medicine, diversity and barriers to care. A second case
features a patient with asthma whose disease is now out of control and negatively impacting his/her
life because of the loss of health insurance and inability to purchase the medicines used in the past.
In addition, there are two quizzes and a final written exam that include multiple-choice questions
specifically addressing health beliefs of patients from different cultures. In general, the first-year
ICM course strives for diversity and inclusivity in quizzes and written examinations by including
diverse representation of patients described in the clinical scenarios in exam question vignettes.
Family Medicine Clerkship:
During the required observed clinical encounter (OCE), the faculty not only evaluates traditional
clinical competencies and skills, but also observes students’ personal connection with the patients
and the their attention to social and cultural issues. In the standardized Evaluation of Clinical
Performance and Professional Attributes, there are three competencies that assess students’ cultural
ED-85
Albert Einstein College of Medicine
Academic Year 2014-2015
competency knowledge and skills and how they incorporate these into patient care: Communication
with Patients and Families; Relationship with Patients and Families; and Patient Management
(must be culturally sensitive and consider the patient’s values and preferences). Two of the 50
multiple-choice questions on the Family Medicine final exam are on cultural competency.
Patients, Doctors & Communities (PDC) – Students take the Implicit Association Test (IAT) as part
of the course. Their participation in written reflection and in small-group discussion is the
assessment tool.
c. Provide evidence that educational program objectives and course or clerkship objectives addressing
cultural competence are being met.
Introduction to Clinical Medicine: Introduction to the Patient:
Four questions on the written exam address various aspects of cultural competence, and these
questions have an average of 90% correct response rate. In addition, the faculty complete the endof-course student evaluation, which includes an item linked to the following ICM competency: To
recognize, understand, and adapt to patient differences (age, gender, cultural factors). Students
must achieve a grade of “Meets Competency” or higher to pass the course.
Family Medicine Clerkship:
One of the two family medicine exam questions on cultural competency is answered correctly by
100% of students, and the second is answered correctly by 71%. Students complete an evaluation at
the end of the rotation, rating different components and objectives on a Likert scale (1, strongly
disagree, through 5, strongly agree). One of the items is: “Able to identify the role of psychosocial
and cultural factors in health and illness.” Students’ response is an average of 4.3/5 (2012-2013
data)
ED-86
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-22. Medical students in a medical education program must learn to recognize and
appropriately address gender and cultural biases in themselves, in others, and in the
process of health care delivery.
The objectives for instruction in the medical education program should include medical student understanding of
demographic influences on health care quality and effectiveness (e.g., racial and ethnic disparities in the diagnosis
and treatment of diseases). The objectives should also address the need for self-awareness among medical students
regarding any personal biases in their approach to health care delivery.
___________________________________________________________________________________
a. Describe where in the curriculum (in formal teaching sessions and/or indirectly through clinical
experiences for all students) students receive instruction addressing the following topics:
1. Demographic influences on health care quality and effectiveness (including disparities in health
care delivery)
Introduction to Clinical Medicine Program:
In the first-year ICM Clinical Experience course, one session is devoted to Public Health and
Preventive Medicine. The Bronx Assistant Commissioner for the New York City Department of
Health presents a lecture that includes elements of disparity in health care delivery. This session
also includes small-group discussions about selected health care topics identified in the Healthy
People 2020 Initiative. While each discussion group touches on disparity and barriers to health and
healthcare, one group explicitly focuses on “Health Care Disparities.” Many of the small groups
also discuss culture and bias as significant factors within health care delivery.
Another session in The Clinical Experience course, “Health Care Finance,” focuses on the political
and economic factors that impact health care delivery, including Medicare, Medicaid, private
insurance, and the Affordable Care Act. Experts in health care finances, systems and demographic
issues related to consumers, providers and cost analyses share lecture time. Small-group discussions
encourage students to analyze aspects of health care delivery that seem to be working, and critique
those aspects which have proved to be ineffective.
The ICM Introduction to the Patient course has sessions addressing gender and gender bias in
which students interview patients with non-normative sexual histories, and a session dedicated to
multiple aspects of sexuality given in workshop format.
Elective Courses in Year 1:
Health Disparities – Course Description: Disparities in health and healthcare are pervasive within
the United States. As physicians, it is our professional responsibility to provide equitable healthcare
to all. This elective addresses these disparities at the level of patient-physician interactions, health
systems, and society at large. Learners will confront bias, gain advocacy skills and develop
strategies for a more just health care system.
2. Students’ self-awareness of their own biases and those of their peers and teachers/supervisors
Family Medicine Clerkship:
During the clerkship, students conduct daily assessments of their outpatient clinical preceptors,
including an item on showing concern and respect for patients. For the clerkship community
project, pairs of students conduct a series of educational sessions in a community setting (e.g.,
ED-87
Albert Einstein College of Medicine
Academic Year 2014-2015
clubhouse for the mentally ill, methadone clinic). Students complete a self-reflection sheet at the
beginning of the community project that solicits student concerns and expected challenges. At these
sites, students have to address any pre-existing biases and stereotypes they may have regarding
specific patient populations before they can effectively interact with their audience. The
community site adviser gives feedback and evaluates students on their professional interaction that
includes showing respect and compassion, and demonstrating sensitivity and responsiveness to
diverse patients.
Patients, Doctors & Communities (PDC): One PDC session explores health care disparities.
Students are asked to consider their clinical encounters during their third-year clerkships and
identify management decisions that differ based on physician perceptions rather than patients
choices. Of these, the students are asked to consider whether there is bias involved in those
decisions. The students also take the Implicit Association Test (IAT) in order to raise awareness
about implicit bias. The students reflect on what they learned about themselves and the impact of
disparity in their final essay.
b. Provide evidence that educational program objectives or course and clerkship rotation-specific
objectives related to gender and cultural biases in health care are being met. For example, include data
from the most recent AAMC GQ (Questions 12, 13) or AAMC CGQ.
Family Medicine Clerkship:
During the clerkship, there is a monthly didactic session titled, Advocacy for Vulnerable
Populations: Optimizing LGBT Health, to assure that the health needs of these patient populations
are addressed with culturally sensitive care. This session is well-received by the students and our
internal survey results reveal that students’ understanding of and comfort level with LGBT health
issues markedly increase after the didactic. Of the exam questions on this topic, 89% of students
answer the first one correctly, and 100% of students answer the second one correctly (2012-2013
data). According to the 2013 GQ, 87.5% of students agreed or strongly agreed they could counsel
someone with a different sexual orientation on safe sex (comparable with the national average).
Family Medicine Elective - Research-Based Health Activism:
The month includes three major curriculum segments to aid in developing a project proposal. The
first segment is background on US health policy and politics. The second segment is epidemiology
and biostatistics in order to develop the skills needed to create credible data that will have an
impact. Finally, the segment on advocacy skills will give students the tools they need to make use of
their findings effectively. Students participate in hands-on learning about media relations, coalition
building, and public speaking. Learning experiences also include talks given by nationally
renowned policy experts, interactive seminars with physician and non-physician activists, journal
clubs and discussion groups, site visits to advocacy organizations, and direct advocacy experiences
such as media contracts or lobbying elected officials.
Percent of Einstein students with:
Experience related to health disparities
Experience related to cultural awareness and cultural competency
Experience with a free clinic for the underserved population
(Data from the 2014 GQ)
ED-88
69.8%
71.9%
71.9%
Albert Einstein College of Medicine
Academic Year 2014-2015
Percent of Einstein students rating their instruction in the following areas:
Women’s health
Culturally appropriate care for diverse populations
*Health and healthcare disparities
(Data are from 2013 GQ)
Health determinants
(Data from the 2014 GQ)
* Question not asked in 2014 GQ
ED-89
Inadequate
8.1%
11.9%
8.8%
Appropriate
90.4%
84.4%
83.5%
Excessive
1.5%
3.7%
7.6%
11.9%
81.3%
0.7%
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-23. A medical education program must include instruction in medical ethics and
human values and require its medical students to exhibit scrupulous ethical principles in
caring for patients and in relating to patients' families and to others involved in patient
care.
The medical education program should ensure that medical students receive instruction in appropriate medical
ethics, human values, and communication skills before engaging in patient care activities. As students take on
increasingly more active roles in patient care during their progression through the curriculum, adherence to ethical
principles should be observed, assessed, and reinforced through formal instructional efforts.
In medical student-patient interactions, there should be a means for identifying possible breaches of ethics in patient
care, either through faculty or resident observation of the encounter, patient reporting, or some other appropriate
method.
The phrase "scrupulous ethical principles" implies characteristics that include honesty, integrity, maintenance of
confidentiality, and respect for patients, patients' families, other students, and other health professionals. The
program's educational objectives may identify additional dimensions of ethical behavior to be exhibited in patient
care settings.
____________________________________________________________________________
a. Identify each course and clinical clerkship rotation that includes an explicit educational objective
related to ethical issues and human values.
All clinical clerkships
PDC Patients Doctors & Communities (PDC)
b. In the Appendix, provide electronic copies of formative or summative instruments used to assess the
acquisition or demonstration of medical students’ ethical behavior during the preclinical and/or clinical
phases of the curriculum. How and in what format is information about student ethical behavior
collected?
Clerkships
See Evaluation of Clinical Performance and Professional Attributes and faculty guide (Appendix EDC). This form assesses student performance in the clerkships in achieving the seven school-wide
competencies. Most relevant to this ED is Competency F, Physician as Role Model, subcompetencies F1 and F2.
Patients Doctors & Communities (PDC):
The PDC course does not have formal instruments for assessing acquisition or demonstration of
ethical behavior. The curriculum of Patients Doctors and Communities is focused on the ongoing
development of the students’ professional identity. This includes the nurturing of the students’
humanism and development of strategies for them to navigate the system when ethical tensions
exist. The goals for students as outlined in the course description are as follows:
Students will develop:
1. A personal understanding of and commitment to the professional values and roles of a
physician.
2. The knowledge, skills, and attitudes to care for individual patients in the context of the
communities and populations of which they are part.
3. The skills needed to sustain you as a physician who strives to practice the highest ideals of
doctoring.
ED-90
Albert Einstein College of Medicine
Academic Year 2014-2015
In each PDC session, the human values and responsibilities of care are discussed. There is constant
tension that the students negotiate/participate in when considering the benefit, risk and burdens
associated with helping patients become better.
The principal venue where assessment of acquisition or awareness of ethical behavior occurs is in
the debriefing of students’ clerkship experiences. Students are quick to identify non-ideal behaviors
and are challenged by their facilitators to describe approaches to improving their own responses to
challenging encounters with patients and with the health care system in general. Faculty and
students of each small group challenge students to recognize bias. The PDC course occurs in a
classroom setting. Thus there is no opportunity to directly observe the students’ behavior with
patients. Nevertheless, both the small-group setting and the structure of PDC allow students to
expose their reflection of encounters that they have witnessed and/or participated in.
c. Describe the methods used to identify and remediate any breaches of ethics in patient care made by
medical students.
PDC Patients Doctors and Communities Course:
On the rare occasion that an individual student writes about or discusses a behavior that faculty
find concerning with respect to demonstrating injustice, imminent harm to patients or others, or
the lack of adherence to professional standards, the faculty facilitator will contact the PDC course
director to discuss how to approach the situation. When this occurs, faculty members and/or the
course director meet with the student to discuss the behavior, and a program of follow-up
procedures is scheduled. If there is consistency with concerns, the course director informs the deans
of students directly. The students are made aware of the preceding process from the first
identification of any concern.
Office of Student Affairs (OSA):
Generally, breaches of ethics are reported by the faculty or other personnel to the course director
(in the first two years of the curriculum). In the clinical years, breaches of ethical behavior are most
likely reported to the clerkship director and/or the assistant dean at that clinical site. The course
director or clerkship director then writes a “letter of concern” to the Office of Student Affairs. The
student is called in to meet with the deans, and a note summarizing the incident and subsequent
action is placed in the student’s OSA file. Depending on the breach of ethics, the deans for students
may require that the student appear before a sub-committee of the Committee on Student
Promotions and Professional Standards. In all instances, a breach of ethics always can be reported
directly to the Office of Student Affairs.
ED-91
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-24. At an institution offering a medical education program, residents who supervise or
teach medical students and graduate students and postdoctoral fellows in the biomedical
sciences who serve as teachers or teaching assistants must be familiar with the educational
objectives of the course or clerkship rotation and be prepared for their roles in teaching
and assessment.
The minimum expectations for achieving compliance with this standard are that: (a) residents and other
instructors who do not hold faculty ranks (e.g., graduate students and postdoctoral fellows) receive a copy
of the course or clerkship rotation objectives and clear guidance from the course or clerkship rotation
director about their roles in teaching and assessing medical students and (b) the institution and/or its
relevant departments provide resources (e.g., workshops, resource materials) to enhance the teaching and
assessment skills of residents and other non-faculty instructors. There should be central monitoring of the
level of residents’ and other instructors’ participation in activities to enhance their teaching and
assessment skills.
There should be formal evaluation of the teaching and assessment skills of residents and other non-faculty
instructors, with opportunities provided for remediation if their performance is inadequate. Evaluation
methods could include direct observation by faculty, feedback from medical students through course and
clerkship rotation evaluations or focus groups, or any other suitable method.
_________________________________________________________________________________
a. Provide information in the following table for each required course or clerkship rotation where
residents, senior medical students, graduate students, or postdoctoral fellows teach, assess, or supervise
medical students.
Course or
clerkship/clerkship
rotation
Advanced Ambulatory
Family Medicine
Ambulatory Medicine
Ambulatory Pediatrics
Bioethics 1
Bioethics 2
Cardiovascular
Physiology
Cardiovascular System
Clinical &
Developmental
Anatomy
List the type(s) of trainee(s) who
provide teaching/supervision:
Nurse
Nutritionist
Physician Assistant
Physician Without Faculty
Appointment*
Resident
None
Social Worker
Nurse
Medical Technician
Physician Without Faculty
Appointment*
Physician Without Faculty
Appointment*
None
None
MD/PhD Student
Medical Student
Describe how objectives are
provided
(e.g., orientation sessions, e-mail,
syllabus)
Email linked to online portal
N/A
Email linked to online portal
Email linked to online portal
Email linked to online portal
N/A
N/A
Email linked to online portal
ED-92
Albert Einstein College of Medicine
Disease Mechanisms
Endocrine Systems
Epidemiology
Population Health &
Evidence-based
Medicine 1
Epidemiology
Population Health &
Evidence-based
Medicine 2
Family Medicine
Clerkship
Family Medicine Subinternship
Geriatrics Clerkship
GI & Liver Systems
Hematology
Histology & Cell
Structure
ICM – Introduction to
the Patient
ICM – The Clinical
Examination
ICM – The Clinical
Experience
Medicine Clerkship
Academic Year 2014-2015
Physician Without Faculty
Appointment*
Nurse
Nutritionist
Resident
Medical Student
Email linked to online portal
Medical Student
Email linked to online portal
Community Worker
Nurse
Nutritionist
Physician Assistant
Physician Without Faculty
Appointment*
Resident
Resident
Email linked to online portal
Attending
Nurse
Nutritionist
Physician Assistant
Resident
Social Worker
None
Medical Student
Post-doc clinical fellow w/o faculty
appointment
Post-doc research fellow w/o faculty
appointment
MD/PhD Student
PhD Student
PhD - Non Faculty
Physician Without Faculty
Appointment *
Physician Without Faculty
Appointment*
Resident
Physician Without Faculty
Appointment*
Physician Without Faculty
Appointment*
Fellow
Physician Without Faculty
Appointment*
Resident
Email linked to online portal
ED-93
Email linked to online portal
Email linked to online portal
Email linked to online portal
N/A
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Albert Einstein College of Medicine
Medicine Sub-internship
Microbiology and
Infectious Diseases
Molecular & Cellular
Foundations of Medicine
Musculoskeletal
Disorders
Neurology
Nervous System/Human
Behavior
Obstetrics & Gynecology
Clerkship
Parasitology
Patients Doctors &
Communities
Pediatrics Clerkship
Pediatrics Sub-internship
Pharmacology
Psychiatry Clerkship
Pulmonary System
Radiology Clerkship
Renal
Reproductive Systems &
Human Sexuality
Surgery Clerkship
Academic Year 2014-2015
Physician Without Faculty
Appointment*
Resident
Microbiologist
Post-doc clinical fellow w/o faculty
appointment
Post-doc research fellow w/o faculty
appointment
Post-doc clinical fellow w/o faculty
appointment
Physician without faculty appointment*
Resident
Physician Without Faculty Appointment
Email linked to online portal
Resident
Resident
Email linked to online portal
Email linked to online portal
Resident
Email linked to online portal
Post-Doc Clinical Fellow W/O Faculty
Appointment
Physician Without Faculty
Appointment*
Other
Resident
Resident
Nutritionist
Other
Nurse
Resident
None
Resident
Physician Without Faculty
Appointment*
Clinical Fellows
Resident
Resident
Fellow
Medical Student
Physician Without Faculty
Appointment*
Physician Without Faculty
Appointment*
Post-Doc Research Fellow W/O Faculty
Appointment
Resident
Resident
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
N/A
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
Email linked to online portal
*This includes newly hired faculty or faculty from new affiliates whose faculty appointments are in process.
b. Describe any institution-level policies that require participation of residents and others (e.g., graduate
students) in orientation or faculty development sessions related to medical student teaching or assessment.
ED-94
Albert Einstein College of Medicine
Academic Year 2014-2015
Institutional policies in courses:
1. Einstein requires each course director(s) or designee (e.g., another faculty member appointed
by the course director) to conduct an annual teaching development session for residents and/or
non-faculty instructors who teach and/or supervise medical students in their course. This session
must occur before the teaching/assessment activity involving residents and/or non-faculty teachers
commences within the course.
2. Course directors must inform the Office of Instructional Support Services when this teaching
development session for residents/non-faculty instructors is scheduled. Notification must occur no
later than two weeks prior to the start of the instructional/assessment activity (e.g., small-group
sessions, observed structured clinical exam, etc.) in the course.
3. Attendance at this session is required, and a sign-up sheet must be collected at the teaching
development session and a copy provided to the Teaching Office demonstrating resident/nonfaculty instructor participation. The Office of Instructional Support Services sends an electronic
copy to the assistant dean for medical education.
Institutional policies for PGY1s in required clerkships/sub-internships:
1. Einstein requires the Office of Medical Education to coordinate annual teaching development
sessions for PGY-1s who teach and/or supervise medical students in required clinical rotations.
2. The assistant dean for medical education, together with the assistant deans at each clinical
affiliate, designate specific Einstein faculty to conduct these teaching sessions at each clinical
affiliate site at an appropriate venue (e.g., intern orientation, retreat day).
3. These sessions are tailored to the specific needs of the PGY-1s and clinical affiliate site. The
emphasis of these sessions should be on creating a productive and effective learning climate.
4. Attendance at this session is required, and a sign-up sheet must be collected by the faculty
facilitator at each teaching development session demonstrating PGY-1 participation and delivered
to the assistant dean for medical education.
Institutional policies for senior residents and other non-faculty instructors in required
clerkships/sub-internships:
1. Einstein requires each clerkship director or designee (e.g., site director, faculty member) to
conduct an annual teaching development session for senior residents (e.g., PGY-2 level or greater)
and/or non-faculty instructors who teach and/or supervise medical students in their course. These
sessions should occur each year at each clinical site where senior residents and/or non-faculty
instructors teach and supervise medical students.
2. Each clerkship director must provide an updated list of these proposed annual teaching
development sessions at each appropriate clinical site and specify the name of the faculty designee
facilitating these sessions. This list should be delivered to the assistant dean for medical education
by October 1st of every year.
3. These sessions should be tailored to the specific needs of the clerkship depending on their
clinical setting(s), teaching/assessment methods, and audience (e.g., senior resident, midwives, etc.).
The emphasis of these sessions should be on creating a productive and effective learning climate.
ED-95
Albert Einstein College of Medicine
Academic Year 2014-2015
4. Attendance at this session is required, and a sign-up sheet must be collected by the faculty
facilitator at each teaching development session demonstrating senior resident/non-faculty
instructor participation and returned to each clerkship director. The clerkship director must also
provide a copy of this attendance sheet to the assistant dean for medical education.
c. Describe any institution-level and department-level programs to enhance the teaching and assessment
skills of graduate students or postdoctoral fellows who teach or assess medical students. If such programs
are the same as those provided for faculty, indicate that fact and refer to the responses for standards FA-4
and FA-11 in Section IV: Faculty.
Einstein has established a centralized teaching development program for all non-faculty instructors
and residents known as the Einstein Teaching Star program. This program features an annual
teaching development session, which occurs in all courses and clerkships/sub-internships where
residents and non-faculty instructors teach and supervise medical students. Attendance at these
sessions is required.
This session integrates the following core teaching development topics, which are standardized
across all Einstein courses, clerkships and at all clinical sites:
a. The roles and attributes of an effective teacher
b. Setting clear expectations with learners
c. The principles of effective feedback
d. The micro-skills of learner-centered teaching
e. Avoiding mistreatment of medical students
The Office of Medical Education provides the PowerPoint presentation and the Teaching Star
manual for faculty facilitators leading these teaching development sessions with non-faculty
instructors and/or residents (See ED Appendix M and ED Appendix N). The session is tailored to
the specific needs and teaching/assessment methods to be used by the course or clerkship (e.g., casebased teaching, team-based learning, problem-based learning, observation, observed structured
clinical examination, etc.).
At the end of each teaching development session, faculty facilitators must provide the non-faculty
instructors and/or residents with access information to secondary online resources and programs
hosted on an Einstein webpage: www.einstein.yu.edu/teachingstar.
Another Einstein teaching development program is offered by Dr. Michael Risley, Professor,
Department of Anatomy & Structural Biology, to advanced graduate students, postdocs and
faculty. This optional program is the “Fundamentals of Course Design and Teaching.” This course
meets once a week for two hours over 17 sessions. The course is designed to integrate lecture and
discussion sessions regarding pedagogical principles and research findings with group-based
projects that provide attendees with direct experience in planning courses and lessons and
implementing appropriate teaching methods to achieve their learning objectives. Learning teams
(4-6 participants each) are formed at the beginning of the course and are maintained throughout.
Each team cooperatively completes a series of projects, each of which contributes to the overall
objective of designing a single course of their choosing. The project is presented to the class at
multiple points in its development for formative feedback. At the completion of all projects, a
course syllabus with learning objectives, detailed lesson plans and teaching methods is produced
based on established educational research. All participants receive an institutional certificate of
successful completion, and graduate students also receive two credits.
ED-96
Albert Einstein College of Medicine
Academic Year 2014-2015
d. In the following table, supply the types of sessions available to residents to prepare them for their
role(s) in teaching and assessment of medical students:
Required
Clerkship
Family
Medicine
Are there programs (departmental or
institutional) available to residents to prepare
them as teachers/supervisors? (Yes/No and
summarize)
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Geriatrics
Medicine
Departmental: Residents-as-Teachers
Series
A series of 3 to 5 workshops a year
offered by faculty development
fellows for Family Medicine residents
at Montefiore and Jamaica Hospital.
Topics include setting clear learning
expectations, feedback skills and time
management skills.
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Department: Resident-as Teacher
Programs
Series of workshops on effective
teaching skills at Jacobi Medical
Center, Long Island Jewish-North
Shore, and Beth Israel Medical
Center.
ED-97
Indicate if the
program is
required or
optional
Note if resident
participation is
centrally monitored
(Yes/No and by
whom)
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required of all
available
residents.
Yes, via attendance
monitored by the
program director.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required of all
available secondyear residents.
Attendance
monitored by the
departments.
Albert Einstein College of Medicine
Obstetrics/
Gynecology
Pediatrics
Academic Year 2014-2015
An annual retreat and online modules
on teaching skills at Maimonides
Medical Center.
Retreat required
of all secondyear residents.
Online modules
required.
A “Residents-as-Teacher” elective at
Montefiore-Weiler Medical Center.
Optional elective
for third-year
residents.
Yes
Institutional: Einstein “Teaching Star”
Program (See description in c., above.)
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Departmental: Clerkship director meets
with Ob-Gyn residents to review basic
teaching principles once a year.
Required
annually of all
residents.
Yes, via clerkship
director.
Departmental: National APGO/ CREOG
conference on education
Optional. Highly
rated resident
teachers are
invited to attend
national meeting.
Yes, via clerkship
director.
Departmental: Residents-as-Teacher
Seminars
Bi-monthly seminars at Long Island
Jewish - North Shore on feedback
skills, time management skills, and
setting clear goals with learners.
Required of
available
residents.
Yes, via attendance
monitored by the
program director.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required of
available senior
residents. Senior
Seminar Series is
offered 6 – 8
times a year.
Yes via attendance
monitored by the
program director.
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Yes
Departmental: Senior Seminar Series
Workshops for Pediatric residents
at the Children’s Hospital at
Montefiore focusing on various
teaching and leadership skills.
Departmental: Residents-as-Teacher
ED-98
Albert Einstein College of Medicine
Academic Year 2014-2015
Program
Program for Pediatric residents at
Jacobi Medical Center, which
teaches practical skills, strategies
for teaching on a busy inpatient
service, feedback skills, how to
assess medical students, and Adult
Learning Theory.
Psychiatry
Radiology
Departmental: Residents-as-Teacher
Conferences
2-3 summer conferences at Bronx
Lebanon on medical student roles
and giving feedback
Departmental: Residents-as-Teacher
Program
A monthly Pediatric resident
conference at LIJ/Cohen’s
Children’s Hospital covering
topics on teaching and
assessment.
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Required at
PGY-1
orientation;
Pediatric noon
conference every
other month.
Yes via attendance
monitored by the
program director.
Required of all
available
residents
Yes via attendance
monitored by the
program director.
Required of all
available
residents once a
month
Yes via attendance
monitored by the
program director.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Departmental: Residents-as- Teachers
Workshop
Session conducted at Bronx
Psychiatric Center during annual all
day retreat for Psychiatry residents.
Topics include teaching microskills,
overcoming barriers to teaching,
feedback skills, and establishing goals
and expectations.
Required
annually of all
residents.
Yes, via attendance
monitored by the
program director.
Department: Resident-as Teacher
Programs
Workshops offered 2 times a year on
effective teaching skills at Long
Island Jewish-North Shore.
Required
annually of all
available
residents.
Yes, via attendance
monitored by the
program director.
Required
annually of all
residents and
Yes, via attendance
sheet collected by
faculty facilitator
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
ED-99
Albert Einstein College of Medicine
Surgery
Academic Year 2014-2015
Department: Resident-as Teacher
Programs
Series of workshops offered 3 times a
year on effective teaching skills at
Long Island Jewish-North Shore.
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Yes
Advanced
Ambulatory Institutional: Einstein “Teaching Star”
Family
Program (See description in c., above.)
Medicine
Departmental: Residents-as-Teachers
Series
A series of 3 to 5 workshops a year
offered by faculty development
fellows for Family Medicine residents
at Montefiore. Topics include setting
clear learning expectations, feedback
skills and time management skills.
Ambulatory No residents or non-faculty instructors are
teaching or supervising students.
Medicine
Ambulatory Yes
Pediatrics
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Family
Medicine
Subinternship
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
ED-100
non-faculty
instructors.
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required
annually of all
residents.
Yes, via attendance
monitored by the
program director.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required of all
available
residents.
Yes, via attendance
monitored by the
program director.
N/A
N/A
Required
annually of all
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required
annually of all
residents and
Yes via attendance
sheet collected by
faculty facilitator
Albert Einstein College of Medicine
Medicine
Subinternship
non-faculty
instructors.
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Required of all
available
residents.
Yes, via attendance
monitored by the
program director.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Assist. Dean for
Medical Education.
Department: Resident-as Teacher
Programs
Series of workshops on effective
teaching skills at Jacobi Medical
Center, Long Island Jewish-North
Shore, and Beth Israel Medical
Center.
Required of all
available secondyear residents.
Attendance
monitored by the
departments.
An annual retreat and online modules
on teaching skills at Maimonides
Hospital.
Retreat required
of all secondyear residents.
Online modules
required.
A “Residents-as-Teacher” elective at
Montefiore-Weiler Medical Center.
Departmental: Residents-as-Teachers
Series
A series of 3-5 workshops a year
offered by faculty development
fellows for Family Medicine residents
at Montefiore. Topics include setting
clear learning expectations, feedback
skills and time management skills.
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
Neurology
Academic Year 2014-2015
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
ED-101
Optional elective
for third-year
residents.
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director,
the Neurology
Education Director,
and Asst. Dean for
Medical Education.
Albert Einstein College of Medicine
Obstetrics
Subinternship
(starting in
2014-15)
Pediatrics
Subinternship
Academic Year 2014-2015
N/A
Yes
Institutional: Einstein Teaching Star
Program (See description in c., above.)
N/A
N/A
Required
annually of all
residents and
non-faculty
instructors.
Yes, via attendance
sheet collected by
faculty facilitator
and monitored by
clerkship director
and Asst. Dean for
Medical Education.
Teaching development session focusing
on roles and attributes of an effective
teacher; setting clear expectations with
learners; principles of effective feedback;
micro-skills of learner-centered teaching;
avoiding mistreatment of medical
students.
Required of
available senior
residents. Senior
Seminar Series is
offered 6-8 times
yearly.
Yes, via attendance
monitored by the
program director.
Departmental: Senior Seminar Series
Workshops for Pediatric residents at
Children’s Hospital at Montefiore
focusing on various teaching and
leadership skills.
Required at
PGY-1
orientation;
Pediatric noon
conference every
other month.
Yes, via attendance
monitored by the
program director.
N/A
N/A
Surgery
Subinternship
(starting in
2014-15)
Departmental: Residents-as-Teacher
Program
Program for Pediatric residents at
Jacobi Medical Center, including
practical skills, strategies for teaching
on a busy inpatient service, feedback
skills, how to assess medical students,
and adult learning theory.
N/A
Also see the Required Course Forms and Required Clerkship Rotation Forms and information for
standard ED-47 on the evaluation of residents as teachers.
ED-102
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-25. Supervision of medical student learning experiences at an institution that offers a
medical education program must be provided throughout required clerkship rotations by
members of the institution’s faculty.
ED-25-A. At a medical education program, students in clinical learning situations
involving patient care must be appropriately supervised at all times. While students learn
through graded responsibility as their skills progress, supervision at all times must ensure
patient and student safety.
The accountability of physicians and non-physicians who supervise medical students in clinical learning
settings will be clearly described in the program’s policies and procedures. The level of responsibility
delegated to the student by the supervisor will be appropriate for the student’s level of training, and the
activities supervised will be within the scope of practice of the supervising health professional.
____________________________________________________________________________________
The following questions relate to standards ED-25 and ED-25-A.
a. Describe how the departments and the central medical school administration ensure that medical
students are appropriately supervised during required clinical clerkship rotations and other required
clinical experiences in order to ensure student and patient safety. Provide electronic copies of policies in
the Appendix describing the accountability of physicians and non-physicians who supervise medical
students.
Pre-clerkship Courses:
ICM-Introduction to the Patient:
In the context of this largely classroom-based course students and small group faculty make 3 visits
to clinical sites for the practice of medical interviewing. Two of these visits are to medical inpatient
wards and one of them is to a psychiatric inpatient hospital. Students receive direct observation and
supervision from their small group faculty during these sessions.
ICM-The Clinical Experience:
In this course, students are at their clinical sites for 2.5 hours on each of 14 sessions spread out
over five months. Some preceptors have dedicated teaching time when their students are present, so
they are not involved in patient care during the session and can spend more concentrated time in
direct observation and feedback with higher preceptor/student ratios (1:4). Preceptors involved in
clinical work when students are present are likewise expected to directly supervise the students, and
so the preceptor to student ratio is lower at 1:1 or 1:2. With the exception of eliciting history and
taking vital signs, students are not directly involved in patient care.
ICM-The Clinical Examination, Part 2:
In this course, students are at their clinical sites for 2.5 hours for 10 sessions between January and
April each year. All of our preceptors have dedicated teaching time for this part of the
course. Thus, preceptors provide direct observation and feedback to students during the time when
they are actually eliciting the history and performing a physical examination on a patient. Students
work in pairs; the student/preceptor ratio is two pairs of students to one preceptor. As mentioned
before, preceptors are trained and required to follow our bedside teaching model, which assures a
universality of instruction throughout this part of the course.
ED-103
Albert Einstein College of Medicine
Academic Year 2014-2015
Clerkships:
During inpatient portions of the required clerkships, students are vital members of the health care
team comprising house staff, attendings and fellows on some services, as well as non-physician
health providers. All student activities on the floors are supervised by faculty and house staff.
Students follow patients in partnership with interns or residents. Attendings listen to patient
presentations and review patient notes. Patient notes may also be reviewed by senior residents.
Procedures performed by students are done under direct supervision. Certain procedures and
invasive examinations, e.g., breast and pelvic exams, are directly observed.
In outpatient settings, students generally work one-on-one with faculty. Students may see patients
with an attending or more often perform their medical history and general physical exams
independently, then present the case to the attending. Attendings are required to personally
evaluate the patient as well and then finalize a plan with the student. Attendings review student
notes.
In addition, it is Einstein’s policy that every student on every required clerkship have an observed
clinical encounter (OCE) performed by a faculty member. Students are directly observed during a
full patient encounter and are given immediate formative feedback on performance of their history,
physical exam, patient education and communication skills. Finally, students log all patients they
care for and document the faculty member and house officer (if applicable) who supervised them
for the encounter.
b. List any required clerkship rotations in which students may be supervised (assessed or graded) by
physicians who are not medical school faculty members (do not include residents/fellows). What steps
are taken to provide faculty appointments to those physicians participating as teachers/supervisors in
required clinical clerkship rotations?
Clerkships:
Physicians supervising and teaching medical students in all clerkships are faculty of the Albert
Einstein College of Medicine. Departments work closely with new faculty and faculty at affiliated
institutions to facilitate application for faculty appointments.
c. Where direct teaching of students is carried out by individuals (physicians and non-physicians) who
do not hold faculty appointments at the medical school, describe how the teaching activities provided by
these individuals are supervised by medical school faculty members.
All course directors, clerkship directors, clinical site directors and attending physicians are
required to have a faculty appointment. All house staff, nurse practitioners, midwives, physician
assistants, community service organization directors and other non-faculty instructors who may not
have faculty appointments are supervised by site directors, course directors, clerkship directors
and/or attending physicians with faculty appointments. All non-faculty instructors and residents
are provided course and clerkship objectives and teaching roles and an annual review of effective
teaching strategies and avoidance of mistreatment of students (as described in ED-24). In addition,
non-faculty instructors and residents have their teaching skills evaluated by students, and those
identified with deficiencies are offered remediation (as described in ED-47).
ED-104
Albert Einstein College of Medicine
Academic Year 2014-2015
d. How do the clinical department and/or the central medical school administration ensure that the level
of responsibility delegated to a student within the clinical setting is appropriate to that student’s level of
training?
Pre-clerkship Courses:
The Introduction to Clinical Medicine courses – by their titles and by their placement within the
first and second year of the overall curriculum – establish the foundation of students’ fund of
clinical knowledge and preliminary skill development. Emphasis on students’ status as beginning
learners is prominent in course instructional materials and is stressed in the orientation meetings
with students. This is also clearly communicated to faculty in both in-person meetings as well as in
the faculty guide. Students receive actual instruction and practice in defining the limitations of their
skills and knowledge in clinical settings and in how to articulate these limitations to superiors if
requested to assume responsibilities beyond their level of training. Assessment of this competency
is included in the evaluation completed by the faculty of the students.
Clerkships:
The general expectations for students’ level of responsibility on clinical rotations are set both
centrally and by departments. Each clerkship and sub-internship has developed learning objectives
directly linked to the Einstein Educational Competencies that define the overall educational
experiences including the clinical responsibilities for students.
In May 2013, a final map of common conditions and procedures all Einstein students must
encounter in required clerkships and sub-internships was established and approved by the Clinical
Directors’ Subcommittee for use starting in 2013-2014. This map is known as the Einstein 203. The
appropriate level of student responsibility has been set for each condition and procedure. See ED
Appendix D for the table, which maps all the common conditions and procedures all Einstein
students must encounter in specific clinical rotations effective in 2013-2014. This table also lists the
level of student responsibility for each condition and procedure on each required rotation.
The Clerkship Faculty Guide posted on eMED is available to all clerkship and clinical site directors.
It defines a number of policies related to student responsibilities on clinical rotations. The policies
include site leader’s and clerkship director’s responsibilities (See ED Appendix O), student work
hours, absences, professionalism and assures that the student’s level of responsibility for patient
care must be consistent with clerkship objectives, suitable to the students’ developmental level, and
under appropriate supervision by attendings and residents.
ED-105
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-26. A medical education program must have a system in place for the assessment of
medical student achievement throughout the program that employs a variety of measures
of knowledge, skills, behaviors, and attitudes.
Assessments of medical student performance should measure the retention of factual knowledge; the development of
the skills, behaviors, and attitudes needed in subsequent medical training and practice; and the ability to use data
appropriately for solving problems commonly encountered in medical practice. The system of assessment,
including the format and frequency of examinations, should support the goals, objectives, processes, and expected
outcomes of the curriculum.
ED-29. The faculty of each discipline should set standards of achievement in that discipline
and contribute to the setting of such standards in interdisciplinary and inter-professional
learning experiences, as appropriate.
___________________________________________________________________________________
The following questions relate to standards ED-26 and ED-29.
a. Describe the role the central curriculum management structure in setting standards of achievement
(e.g., establishing the grading policy for individual courses and clerkship rotations). If there are no
institutional policies regarding assessment of student performance, describe the means by which standards
of achievement are set for individual required courses and clerkship rotations.
The Executive Committee of the Medical Education Council reviews the grading policy and any
changes proposed from the Course Directors Sub-committee and the Clinical Directors
Subcommittee. Prior to that review, policies are discussed at the Course Directors Subcommittee
and the Clinical Directors Sub-committee.
Pre-clinical Courses:
Course grades in the first two years are either Pass or Fail. School policy defines a passing grade as
65.00% or higher, or 1.5 standard deviations below the course mean, whichever is lower. A course
grade may include components from mid-course exams, final exams and quizzes. This information
is detailed on each course’s eMED home page.
Variations to this policy are listed below:
Some courses have a single exam, and there are no variations.
Other exams have written and visual/lab components that are combined to reach a final
grade.
Other courses may have quizzes that contribute to the course grade.
For some courses, students need to pass the last/final exam; although a student may achieve
an average over all exams that is >65%, he/she will need to make up that exam failure.
According to a recent policy adopted by the Executive Committee of the Medical Education
Council, for courses using an active learning component that incorporates assessment (e.g., teambased learning), the student must pass this component in order to pass the course. (ED Appendix
P.)
The ICM courses use a competency-based evaluation system. Students are assessed with
behaviorally anchored evaluations (see below c) and in order to achieve a passing grade in the
course students must meet the standard in all the competency areas.
ED-106
Albert Einstein College of Medicine
Academic Year 2014-2015
Clerkships:
In the clinical years, direct oversight of grading policies and standards of achievement is the
responsibility of the Clinical Directors Sub-committee of the Medical Education Council. The Subcommittee in turn reports to the Executive Committee, which must provide final approval.
The Einstein Evaluation of Clinical Performance and Professional Attributes form used to evaluate
students in all clinical rotations has undergone a staged revision process over the last several years.
During the 2010-11 academic year, a working group comprising members, mostly clerkship
directors, of the Clinical Directors Subcommittee made the first changes by adding a clear objective
for each evaluated item, then writing verbal anchors for the lowest, middle, and highest levels of
achievement for each. The form was put into use at the start of the 2011-12 academic year. (See ED
Appendix C).
The working group reconvened in June 2012 and was charged reviewing clerkship grading policies,
ensuring standardization of certain grading guidelines, and further modifying the student
evaluation form. The group worked throughout the academic year, made multiple
recommendations on grading policy, and enhanced the student evaluation form; all of these
changes were ultimately approved by both the full Clinical Directors Sub-committee and Executive
Committee.
A major change to institutional clerkship grading policy was the reduction in the grading scale
from a 7-point to 5-point scale (H/HP/P/LP/F). Major components of clerkship grades were defined,
including knowledge, clinical performance, and other graded activities. In most clerkships, the
NBME shelf exam is administered at the end of the clerkship and is used for assessment of
knowledge. Family Medicine has its own non-NBME final exam, drawn from a bank of questions
shared with Columbia University’s College of Physicians and Surgeons and updated jointly;
Surgery and Ob/Gyn have oral exams to further assess knowledge. Clinical performance is based
on cumulative evaluations by faculty and house staff who directly supervise students on the rotation
using the Evaluation of Clinical Performance and Professional Attributes form. Finally, other types
of graded activities used in various clerkships, such as OSCEs, patient write-ups, evidence-based
essays, community projects, problem-based learning, team-based learning, observed encounters,
and oral presentations used to assess students, make up the final portion of the grade.
Determination of the weight of the three components: (clinical evaluation, exam, and other) is left to
the individual clerkships. (ED Appendix Q contains the general clerkship grading policies and two
examples of clerkship-specific grading policies.) These grading policies only apply to clerkships of
four weeks or longer. Two-week clerkships, such as Radiology and Geriatrics, are graded on a
Pass/Fail basis.
In addition, the working group further revised the institutional form for evaluation of students. The
evaluated items were carefully reviewed and updated, becoming more competency-based and
aligned with the Einstein Educational Competencies. The scale for evaluated items was, similarly to
the overall grade, reduced from seven to five levels, and numbers for these levels were removed.
Instead, verbal anchors were written for each level of each competency evaluated. Guidelines for
use were attached for distribution to all individuals evaluating students including site leaders,
faculty and house officers (See ED Appendix C). The new evaluation form was introduced for use in
all third-year clerkships at the start of the 2013-14 academic year and will be used for all fourthyear rotations at the start of the 2014-15 academic year.
Finally, the group recommended a policy that over the course of an entire academic year, the goal is
for a maximum of 20-33% of students within a clerkship to be awarded a grade of honors. Changes
ED-107
Albert Einstein College of Medicine
Academic Year 2014-2015
to grading policies to reach this goal can only be made at the start of a new academic year. This
policy took effect with the start of the 2013-14 academic year. Based on the experience of past years,
it is anticipated that of the entire class at the end of each year, approximately 25-30% of student
will have earned Honors, 50% High Pass, 20% Pass, and 1-2% Low Pass. Individual clerkships
have the ability to work within these guidelines.
b. Describe any policies related to the scheduling of examinations in the preclinical years. How are
examination schedules determined?
The schedule for the preclinical years, including the timing and placement of all course exams is
drafted by the senior associate dean for medical education, with the assistance of the director of the
Office of Instructional Support Services. This draft is shared with all course directors prior to
finalizing to ensure that the schedule meets course objectives and assessment strategies. A
minimum of one study day or weekend is built into the schedule so that students have adequate
study time for each mid-term and final exam. Almost all mid-terms and finals are scheduled at
9:30 AM, and usually last for 2-3 hours. After the exam students usually have a free afternoon for
rest and relaxation.
All course directors are required to post the grading policy for their courses and the weights for
each component on our electronic learning management system, eMED. The placement of this
information is standardized in all courses, and posted under the “grading and evaluation” tab on
the course home page.
The exam schedule is posted prior to the start of the academic year. Make-up exams are scheduled
in advance with one date per course. First-year make-up exams are scheduled to ensure that
students can complete prior to entry to year 2. Second-year make-up exams are scheduled so that
students can enter the clinical clerkships at the beginning of year 3. The final make-up exam
schedule is shared with the Office of Student Affairs for review so that all students on customized
schedules will be able to take the make-up exams on the scheduled dates.
c. Include PDFs in the Appendix of examples of standard form(s) used by faculty members or resident
physicians to assess students in small-group settings during the preclinical years and during required
clinical clerkship rotations. Describe the purpose of each form (i.e., what is being assessed).
The following forms appear in ED Appendix R:
Preclinical:
ICM: Introduction to the Patient:
1. The Communication Skills Checklist is provided as a formative assessment tool for course faculty
to use with students to provide guided feedback on the student’s interpersonal and communication
skills throughout the course (in-class interviews; medical ward interviews; and the reviews of
digitally recorded standardized patient encounters).
2. The Case Write-Up Rubric is provided to course faculty in their review of submitted written case
write-ups by the students. It was developed by our faculty to establish greater consistency in our
formative assessment and feedback to students.
ED-108
Albert Einstein College of Medicine
Academic Year 2014-2015
3. The Mid-Year Course Evaluation is provided as a formative assessment tool for course faculty to
provide feedback on the student’s progress with knowledge and application of interviewing
technique, written and oral case presentations; interpersonal and communication skills; and
professionalism prior to their winter break (end of December). Each student receives a single
evaluation completed by both faculty collaboratively.
4. The Reflective Writing Evaluation Rubric is provided to course faculty in their review of
submitted narrative essays by the students. It was developed by our faculty to establish greater
consistency in our formative assessment and feedback to students regarding their reflective writing
abilities.
ICM: Clinical Examination:
5. The Part I Evaluation is provided as a summative assessment tools for clinical faculty to provide
feedback on the student’s understanding of the techniques and ability to properly conduct a
physical examination in their peer-practice group prior to their winter break (end of December).
6. The Part II Evaluation is provided as a summative assessment tool for clinical preceptors at the
end of the course (March). Students who work with more than one clinical preceptor may have
either multiple evaluations submitted or their preceptors may elect to collaborate and submit one
evaluation for the student. Evaluations focus on student’s progress with knowledge and application
of interviewing technique, written and oral case presentations; understanding and application of
physical examination maneuvers; clinical reasoning; interpersonal and communication skills; and
professionalism
Clerkships:
7. Pediatrics Clerkship - PBL Evaluation Form. Groups of 5-10 students work collectively through 67 cases and are evaluated on such items as clinical reasoning, knowledge, self-directed learning,
participation, contribution to group learning, and collegiality.
8. Medicine Clerkship - GOSCE Evaluation Form. Groups of 4 students rotate through four
encounters with standardized patients, with students taking turns as the interviewing physician.
Students are evaluated on their communication skills.
9. Family Medicine Clerkship – Team-Based Learning Readiness Assurance Test (i.e., quiz).
Students review online modules prior to the session. During the session, the individual quiz assesses
the individual student’s ability to recall and apply concepts from the modules. The quiz is then
retaken by groups of 4-7 students, allowing students to learn from each other, and demonstrate
their ability as a group to recall and apply concepts. The scores on the group quizzes, compared to
individual quizzes, indirectly measure group effectiveness.
10. Family Medicine Clerkship - Community Project Evaluation Form. Groups of 2-3 students
provide a 15-minute presentation to their peers on their project at the end the rotation. An
evaluation form with specific behavioral anchors tied to community health-related clerkship
objectives is completed independently by 3 faculty members while viewing the presentations.
Objectives include knowledge about and application of community health concepts, and
presentation skills, including partnership and engagement of the audience.
ED-109
Albert Einstein College of Medicine
Academic Year 2014-2015
See information for standards ED-1 and ED-33 and Required Courses and Clerkship Rotations, Part A,
item (B). Also, refer to the information for standard MS-33 in Section III: Medical Students relating to
assessment of student performance.
ED-110
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-27. A medical education program must include ongoing assessment activities that
ensure that medical students have acquired and can demonstrate on direct observation the
core clinical skills, behaviors, and attitudes that have been specified in the program's
educational objectives.
_____________________________________________________________________________________
a. Is there a list of core clinical skills, behaviors, and attitudes that students must demonstrate? (select
one response)
X
Yes, included as part of the institutional educational
objectives
Yes, as a separate list for each required clinical clerkship
rotation
No (please explain)
b. List each OSCE or standardized patient assessment that occurs outside of individual courses or
clerkship rotations, including when in the curriculum it is offered, and describe the general content areas
each covers. For each, indicate whether the purpose of the OSCE or standardized patient assessment is
formative (i.e., to provide feedback to the student) or summative (i.e., to inform decision-making about
academic progression or graduation).
A Clinical Skills Assessment (CSA) is scheduled in the spring (March-May) of the third year and is
independent of any course or clerkship. The CSA is overseen by the Clinical Skills Assessment Task
Force of the Medical Education Council, which meets monthly and is chaired by the director of the
Clinical Skills Center. The CSA is an 8-station OSCE with an encounter with a standardized
patient at each station (15 minutes), followed by a post-encounter written exercise (10 minutes).
The format is much the same as the USMLE’s Step 2 CS.
The cases cover a wide variety of clinical areas, including internal medicine, adolescent medicine,
geriatrics, surgery, psychiatry, behavioral counseling, and a pediatric telephone case. The postencounter note is designed to fit the case but is most commonly the same format as Step 2 CS.
Students are asked to list up to three diagnoses, in order of likelihood, and then to defend these
diagnoses with data from the history and physical exam. Students are evaluated by the
standardized patients (SPs) who complete history, physical exam and communication skills
checklists. The standard for passing is non-compensatory and normative. In order to pass, students
must achieve a score above 2 SD below the mean in overall score and on all three components
(history, physical exam and communication). We are currently working on the use of a global
rating scale that can be used to create a criterion-based passing standard.
The purpose of the CSA is both summative and formative. If a student fails, he/she must complete
a self-assessment assignment and meet with a faculty reviewer to review the videos, notes and
scores. The faculty member will help the student identify strengths and weaknesses and develop a
plan for improvement. During the summer there is a 4-station retest that the student must take. If
the student fails the retest, there will be a review of his/her academic record.
Students who pass the CSA meet in groups of four with faculty reviewers. Each student comes
prepared to review one or two video segments with faculty facilitating the discussion of the cases
and clinical skills. Faculty will also give the students feedback on their post-encounter notes based
on a grading rubric created by the CSA subcommittee.
ED-111
Albert Einstein College of Medicine
Academic Year 2014-2015
c. Complete the following table with data from the AAMC GQ, the AAMC CGQ and/or other schoolspecific sources (e.g., clerkship evaluations) that indicate whether students’ clinical skills are being
directly observed by faculty members in each required clinical clerkship rotation.
Rotation
% agreeing they were observed
History
Family Medicine
Internal Medicine
Neurology*
Obstetrics-Gynecology
Pediatrics
Psychiatry
Surgery
Data from the 2014 GQ
* Added to 2014 GQ
92.3
97.8
87.6
92.0
96.4
97.8
71.7
Physical
Examination
89.9
97.1
96.5
94.9
96.4
97.8
77.4
National % agreeing they were
observed
History
Physical
Examination
85.8
88.3
91.5
92.8
76.1
86.5
77.9
88.7
89.0
91.3
89.0
87.6
66.4
74.9
d. Provide data from the AAMC GQ (Question 16), the AAMC CGQ, the independent student analysis
or other internal data sources that address students’ perceptions of their ability to perform core clinical
skills (for example):
From AAMC GQ
I am confident that I have the
clinical skills to begin a residency
program
Data from the 2014 GQ
% strongly agree or
agree
(National %)
91.0%
% of students
participating in the
survey
75% (for this question)
94.1% (overall survey
response)
Also see Required Courses and Clerkship Rotations, Part A, item (B.).
ED-112
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-28. A medical education program must include ongoing assessment of medical
students’ problem solving, clinical reasoning, decision-making, and communication skills.
__________________________________________________________________________________
In the Appendix, provide electronic copies of a representative sample of the materials and methods (e.g.,
written or oral examination questions, research paper assignments, problem-based learning cases)
specifically designed to assess students’ skills in the following:
1) problem solving,
2) clinical reasoning, and
3) communication.
Indicate the courses or clerkship rotations that employ such materials or methods.
1. Problem Solving:
Molecular & Cellular Foundations of Medicine (MCFM):
Case of Boy with Developmental Delay – This case-based exercise asks students to search
OMIM and GeneReviews, asking if symptoms implicate a genetic disease. (ED Appendix S)
Epidemiology, Public Health, and Evidence-Based Medicine (EPHEM 1and 2):
Observational Studies: Mammographic Screening for Breast Cancer: Based on a clinical case,
students are asked to identify both the limitations and advantages of observational studies and
randomized trials in the evaluation of screening strategies, identify biases associated with the
evaluation of screening strategies. (ED Appendix S)
Bioethics 2 Mid-course Essay: (ED Appendix S-1)
Radiology Clerkship:
Reading of radiologic studies on either iPads or through simulation with monitors and dictation
equipment- assess problem solving and communication skills.
2. Clinical Reasoning
ICM: The Clinical Examination: Bedside Teaching Model Preceptor Guide
The overall objective of this bedside teaching model is to improve second-year students’ history
taking and physical examination skills through direct observation and feedback. In addition to
increasing history taking and PE skills performance at the clinical sites, this model also includes
an opportunity to teach students the skills of oral case presentation and clinical reasoning.
(ED Appendix S-2)
Pediatrics Clerkship:
Summary statement project - assesses clinical reasoning through analysis of summary
statements. Feedback provided electronically on summary statements for online cases (CLIPP)
or directly based an OSCE case.
Pediatrics Clerkship:
Patient write-ups – assess communication (written) problem solving and clinical reasoning in
two comprehensive patient case write-up assignments, including thorough documentation of
ED-113
Albert Einstein College of Medicine
Academic Year 2014-2015
history, physical and studies, plus in depth analysis of each item on the student’s differential
diagnosis (See Appendix S-2).
Pediatrics Clerkship:
PBL - assesses problem solving and clinical reasoning skills through collective analysis of 6-7
cases, with 5-10 students per group (ED Appendix S-2)
Medicine, Family Medicine, Surgery, Radiology and Pediatrics Clerkships:
MedU online interactive cases assess both problem solving and clinical reasoning skills.
Family Medicine Clerkship:
Team-based Learning provides the opportunity to assess problem-solving, clinical reasoning,
and decision making through the individual/group quiz questions based on modules reviewed
by students prior to the session.
3. Communication:
Introduction to Clinical Medicine:
ICM utilizes several methodologies to assess communication skills through years 1 and 2. These
include small-group interviews with real and standardized patients, videotaped interviews with
standardized patients and real patient interviews in the clinical setting with direct observation
and feedback from faculty. All these exercises utilize the Communication Skills Checklist
developed at Einstein. This checklist is used by students to self-assess, do peer assessment and
by faculty to assess students communication skills (See ED Appendix S-3).
Medicine Clerkship:
GOSCE - assesses communication skills using a four-station group OSCE: 1) Tobacco
dependence 2) Difficult doctor/patient encounter 3) Shared decision making 4) Delivering bad
news (See ED Appendix S-3).
Medicine Sub-internship:
OSCE- assesses advanced communication skills through 2 OSCE cases on 1) Refusal of care
and 2) Delivering bad news (See ED Appendix S-3)
Pediatrics Clerkship:
OSCE - Adolescent case assesses communication and professionalism skills in an outpatient
encounter with an adolescent, through an OSCE using standardized patients. (See ED
Appendix S-3).
When answering the question, limit the response to a few appropriate examples of assessment materials
and methods that illustrate how the relevant skills are assessed. Additional information or examples can
be provided to the survey team on site, if requested.
Also see the Required Course and Clerkship Rotation Forms and the information for standards ED-6/7
and ED-19.
ED-114
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-30. The directors of all courses and clerkship rotations in a medical education
program must design and implement a system of fair and timely formative and summative
assessment of medical student achievement in each course and clerkship rotation.
Faculty of the medical education program directly responsible for the assessment of medical student
performance should understand the uses and limitations of various test formats, the purposes and benefits
of criterion-referenced vs. norm-referenced grading, reliability and validity issues, formative vs.
summative assessment, and other factors associated with effective educational assessment.
In addition, the chief academic officer, curriculum leaders, and faculty of the medical education program
should understand, or have access to individuals who are knowledgeable about, methods for measuring
medical student performance. The medical education program should provide opportunities for faculty
members to develop their skills in such methods.
An important element of the medical education program’s system of assessment should be to ensure the
timeliness with which medical students are informed about their final performance in courses and
clerkship rotations. In general, final grades should be available within four to six weeks of the end of a
course or clerkship rotation.
____________________________________________________________________________________
a. Describe the availability of individuals knowledgeable about educational assessment who can assist
faculty in developing formative and summative assessments of students (e.g., experts in test development
or educational measurement). Describe the organizational placement of such individuals (e.g., medical
school office, university office, department).
1. William Burton, Ph.D., Associate Director of the Office of Educational Resources, has extensive
training and expertise in evaluation methodology and educational measurement. He is readily
available for consultation with faculty and has presented a variety of faculty development
workshops on these topics (see below).
2. Joshua Nosanchuk, M.D., Director of the second-year Microbiology and Infectious Diseases
course, has worked with the NBME on the development and review of questions for the USMLE
Step examinations. Dr. Nosanchuk has assisted course faculty in the development of “board-type”
questions for course examinations and presented a workshop demonstrating effective questionwriting techniques to the Course Directors Subcommittee in the 2011-2011 academic year.
3. Felise Milan, M.D. and Sharon Parish, M.D. have developed a behaviorally anchored
Communications Skills checklist that has been in use for a number of years in the Introduction to
Clinical Medicine program in years 1 and 2. In year 3 it is used to assess the students in the end of
3rd year clinical skills assessment (see further description ED 27).
b. List any workshops or similar activities for faculty that were given during the most recent academic
year that addressed methods of assessing student performance.
Workshops given during the 2013-2014 academic year and scheduled for 2014-2015:
1.
-
Classroom Assessment
Define formative and summative assessment, and describe their interrelationship
Define the key terms and concepts used in the assessment of teaching and learning
ED-115
Albert Einstein College of Medicine
2.
-
Academic Year 2014-2015
Construct tests that are valid, reliable, and fair
Use classroom assessment techniques to enhance your students’ learning
Become educated consumers of assessment data
Writing and Analyzing Multiple-Choice Questions
Describe the strengths and limitations of multiple-choice questions (MCQs).
Define the difference between norm-referenced and criterion-referenced tests.
Create a test blueprint to guide your item writing.
Review MCQs for technical item flaws (most importantly, avoid unintended barriers
and clues).
Conduct test-item analyses to assess and improve your MCQs.
The following workshops were presented in the 2011-2012 academic year:
3.
Classroom Assessment Techniques
Describe how CATs can help you answer two fundamental questions: How well are my
students learning? How effectively am I teaching?
Utilize CATs to measure: Course-related knowledge and skills; Learner attitudes;
Learner reactions to instruction
4.
-
Evaluating Instructional Effectiveness
Learn some common terms and concepts used in instructional evaluation
Describe the four levels of Kirkpatrick’s model of instructional evaluation
Develop skill in writing effective learning objectives
Utilize readily available tools to integrate evaluation into your teaching
Use evaluation data to improve your teaching and your students’ learning
Einstein has made an ongoing commitment to training faculty to improve their skills in student
assessment. In addition to the in-house training provided to faculty listed above, the Office of
Medical Education has been sending 1-2 faculty members each year to programs providing
significant training on assessment, including the Harvard Macy Program for Educators in Health
Professions and the Systems Approach to Assessment in Health Professions Education, as well as
the Primary Care Faculty Development Program at Michigan State University. Faculty members
trained in these programs are listed below:
Dr. Martha Grayson, Senior Associate Dean for Medical Education;
Dr. Pablo Joo, Assistant Dean for Medical Education;
Dr. Penny Grossman and Dr. William Burton, former Assistant Dean and current Associate
Director, Office of Educational Resources;
Dr. Maria Santos, Clerkship Director for Family Medicine;
Dr. Yvette Calderon, Associate Dean for Diversity Enhancement;
Dr. Felise Milan, Director of the Ruth L. Gottesman Clinical Skills Center;
Dr. Elizabeth Kitsis, Director of Bioethics Education;
Dr. Lisa Auerbach (Medicine), Dr. Andrea Littleton (Family Medicine), and Dr. Elizabeth
Ihler (Medicine), three faculty members who train and assess students in ambulatory care
sites.
In addition, the assistant dean for medical education attended the FAME (Fundamentals of
Assessment in Medical Education) course sponsored by the NBME and the Foundation for
Advancement of International Medical Education and Research in the summer of 2014.
ED-116
Albert Einstein College of Medicine
Academic Year 2014-2015
c. Provide information on the average length of time for preclinical course grades to be made available
to medical students. List courses where any students received their grades in more than six weeks.
The completion of evaluations is considered an important component of each course and clerkship
As such, after the completion of an exam period in each course, students are required to complete
the online evaluations for the courses ending during that period. Students have one week from the
date of the last exam of the period to log on and complete the evaluations. An email reminder is sent
to students clearly indicating this deadline. Although exam grades are “posted” electronically
generally a few days after the exam, they are made accessible to students on the next business day
after completion of the course evaluation.
Those students who have not completed the evaluation by the end of the one-week deadline receive
a second e-mail giving them one additional week in which to complete the evaluation. Virtually all
evaluations are completed by the end of the first week, as students are eager to receive their grades.
By the end of the two-week deadline, all evaluations have been completed and all grades released.
d. Complete the following table for each required clinical clerkship/clerkship rotation during the last
completed academic year. (Updated for 2013-2014)
Required clerkship
Medicine
Pediatrics
Psychiatry
Obstetrics/Gynecology
Surgery
Family Medicine
Geriatrics
Radiology
Neurology
Medicine Sub-internship
Medicine Ambulatory Care
Pediatrics Sub-internship
Pediatrics Ambulatory Care
Family Medicine Sub-internship
Family Medicine Ambulatory Care
Average time (in
weeks) for
students to
receive clerkship
grades
4.41
4.32
3.97
2.92
3.57
5.43
3.91
0.56
2.22
5.25
3.44
4.35
2.99
5.90
5.93
Minimum and
maximum number
of weeks (range)
for students to
receive clerkship
grades
3.00-5.29
3.14-5.43
2.14-7.43
1.29-4.57
1.43-7.43
3.29-5.71
1.29-8.71
0.14-2.29
0.43-6.00
3.39-8.57
1.00-11.14
0.14-5.57
0.14-4.57
4.86-6.86
5.71-6.14
Number (percent) of
students who did not
receive grades
within six weeks
0 (0%)
0 (0%)
2 (1.1%)
0 (0%)
4 (2.1%)
0 (0%)
13 (13.9%)
0 (0%)
0 (0%)
1 (0.8%)
1 (0.9%)
0 (0%)
0 (0%)
1 (33%)
1 (50%)
List clerkship rotations (or clerkship rotation sites) that are significant outliers.
Geriatrics Clerkship.
e. Describe how and by whom the timing of provision of clerkship grades is monitored? How does the
medical school ensure that course and clerkship rotation grades are released to students in a timely
manner?
ED-117
Albert Einstein College of Medicine
Academic Year 2014-2015
Einstein’s policy on the release of grades to students, adopted by the Executive Committee in 2010,
is as follows:
“In compliance with the Liaison Committee on Medical Education (LCME) Standard ED-30. The
Albert Einstein College of Medicine has adopted a policy requiring that course and clerkship grades be
made available to students no later than six weeks after the end of the course of clerkship.”
In accordance with this policy, clerkship directors are provided with a chart created by the
Registrar’s Office, which lists the grade submission due dates prior to the start of the academic
year (See Example 1). Site leaders and clerkship directors are sent email notifications once a
clerkship rotation has concluded informing them that evaluations are ready for completion. Email
reminders are sent every two weeks to site leaders and clerkship directors until each evaluation has
been submitted to the Registrar’s Office (See Example 2).
Grades are released to each student once the Registrar’s Office receives authorization from the
Office of Educational Resources that the student has submitted his evaluation of the rotation.
Grades are typically released within 1-2 days after submission from the clerkship directors.
Students receive an automated email informing them that their grades are available to view.
The Registrar’s Office provides each clerkship director with a timeliness of grade submission
report during the monthly Clerkship Director’s meeting to discuss any issues with grade
submission.
Example 1:
Example 2:
Subject: E*Value Incomplete Reminder Notice
Dear Clerkship Leadership,
This is an automated notification to remind you that you have pending evaluation(s) for completion
posted to your E*Value Pending List for the Medicine clerkship, rotation period of _______ to
_______.
ED-118
Albert Einstein College of Medicine
Academic Year 2014-2015
You will receive an automated e-mail reminder approximately every 14 days until the evaluation is
finalized and submitted. Please be reminded, in accordance with LCME accreditation standards, all
final grades should be submitted within four to six weeks of the end of a course/clerkship.
To complete pending evaluations please log in to the E*Value Evaluation System at the following
website https://www.e-value.net/index.cfm.
Please do not hesitate to contact the Office of the Registrar at registrar@einstein.yu.edu if we may
be of assistance to you.
Thank you,
Office of the Registrar
Registrar@einstein.yu.edu
Example 3:
Subject: Yeshiva University Academic History Grade
Dear Student:
A final grade has been recorded for the following course(s) Medicine Clerkship (Subject MED,
Course ME3) from term Fall _____. If you have received a grade of Incomplete, it is your
responsibility to resolve the Incomplete with your professor.
You can view your grades at www.yu.edu/myyu.
Questions? Contact your campus registrar: http://www.yu.edu/registrar/contact
** Please DO NOT reply to this email. It is being sent by an automatic process. **
Also see information for standards ED-26 and ED-31 in this section, MS-33 in Section III: Medical
Students, Required Courses and Clerkship Rotations, Part A, item (B.), and individual Required Course
and Clerkship Rotation Forms.
ED-119
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-31. Each medical student in a medical education program should be assessed and
provided with formal feedback early enough during each required course or clerkship
rotation to allow sufficient time for remediation.
Although a course or clerkship rotation that is short in duration (e.g., less than four weeks) may not have
sufficient time to provide a structured formative assessment, it should provide alternate means (e.g., selftesting, teacher consultation) that will allow medical students to measure their progress in learning.
_____________________________________________________________________________
a. Describe the institutional policies and procedures that are in place to ensure that students receive
feedback by at least the mid-point of courses and of clerkships/clerkship rotations (of four weeks duration
or longer). Describe the means by which the occurrence of mid-course and mid-clerkship rotation
feedback is monitored within individual departments and at the curriculum management level.
Pre-clerkship courses give mid-course feedback in the form of quizzes and mid-course
examinations. These courses (first and second year) give quizzes: Histology (1st), Molecular and
Cellular Foundations of Medicine (1st), Clinical and Developmental Anatomy (1st), EPHEM (1st
and 2nd) and GI System (2nd).
The following courses give one mid-course exam: Histology, Clinical and Developmental Anatomy,
Pharmacology (1st), Renal System (1st), Bioethics 2 (2nd), Pulmonary System (2nd) and Infectious
Disease (2nd).
The following courses give more than one mid-course exam: Molecular and Cellular Foundations of
Medicine and Nervous System and Human Behavior (2nd).
In the ICM course the faculty complete mid-course evaluation forms and meet with the students
individually to give them formative feedback on their communication skills, participation in class
and their professionalism.
For the required third- and fourth-year clerkships which are > 4 weeks in duration, there is a
school-wide policy with guidelines for mid-cycle feedback, developed by the Clinical Directors
Subcommittee of the Medical Education Council. First, the policy requires that the site leader or a
designated faculty member give the mid-cycle feedback. In addition, the mid-cycle feedback session
must include the following components:
a. Review of progress in completion of required elements of the rotation
b. Review of patient log
c. Meaningful review of clinical performance.
i. If the person giving feedback does not have direct knowledge of student’s
performance, he/she must obtain it through written or verbal reports from
those who do.
ii. Student self-assessment; format determined by rotation
iii. Identification of areas of strength and areas needing improvement
d. Setting of learning goals for remainder of rotation
Furthermore, all these components of mid-cycle feedback must be documented for the student’s onsite file, using, at a minimum, the Einstein Clinical Rotation Mid-cycle Feedback Meeting
documentation form or an equivalent clerkship specific form. Both the student and faculty member
giving feedback sign the form.
ED-120
Albert Einstein College of Medicine
Academic Year 2014-2015
It is the responsibility of the site leaders to ensure that the mid-cycle feedback sessions take place,
and to record this in a designated box on the students’ final evaluation forms. All evaluation forms
are submitted to the clerkship directors and to the Registrar. Clerkship directors work with site
leaders with deficiencies to ensure compliance with this requirement.
Also, students evaluating each clerkship are asked if they have met with a preceptor for mid-cycle
feedback during the clerkship. The composite results are reported biannually in the clerkship
evaluation reports compiled by the Office of Educational Resources and sent to clerkship directors,
site leaders, the senior associate dean for medical education, department chairs, the deans for
students, and the assistant dean for the site. Clerkship directors present the data during their
annual clerkship review by the Clinical Directors Sub-committee (See ED Appendix G for midcycle feedback guidelines and forms).
b. Provide data, by clerkship/clerkship rotation, from the AAMC GQ (Question 8) or the AAMC CGQ,
clerkship evaluations, and/or the independent student analysis that illustrate the percentage of students
agreeing that they received sufficient feedback during their clerkships/clerkship rotations.
Clerkship
% of respondents agreeing
that they received sufficient
feedback
Family Medicine
93.8%
Internal Medicine
100%
*Neurology
94.7%
Obstetrics-Gynecology
96.4%
Pediatrics
98.5%
Psychiatry
97.1%
Surgery
84.1%
Data from 2014 GQ
*Neurology was included in 2014 GQ
National % of
respondents agreeing
(if data from the AAMC
GQ are used)
93.3%
96.8%
83.7%
91.1%
95.0%
90.7%
88.4%
c. Provide data from clerkship evaluations or other sources on the percent of students reporting that they
received mid-clerkship feedback.
Percent of Students Reporting Mid-Clerkship Feedback:
Clerkship
Medicine
Pediatrics
Psychiatry
Obstetrics & Gynecology
Surgery
Family Medicine
Neurology
June-November 2012
91.7%
91.3%
95.7%
100.0%
73.5%
100.0%
89.2%
December 2012-May 2013
95.2%
94.1%
89.1%
98.9%
89.5%
97.8%
92.8%
Data from 2012-2013 clerkship evaluations – Office of Educational Resources
ED-121
Albert Einstein College of Medicine
Academic Year 2014-2015
d. Provide information regarding students’ perceptions of the utility of feedback and its relationship to
the criteria that will be used for summative grading in the clerkship/clerkship rotation.
Percent of Students Reporting that Mid-Clerkship Feedback Was Constructive:
Clerkship
Medicine
Pediatrics
Psychiatry
Obstetrics & Gynecology
Surgery
Family Medicine
Neurology
June-November 2012
87.8%
92.4%
100.0%
96,9%
79.4%
98.8%
92.3%
December 2012-May 2013
87.4%
97.6%
97.8%
94.4%
88.2%
100.0%
98.0%
Data from 2012-2013 clerkship evaluations – Office of Educational Resources
Also see information provided in Required Courses and Clerkship Rotation Forms for the types of
formative assessments that are available in individual courses and clerkships.
ED-122
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-32. A narrative description of medical student performance in a medical education
program, including non-cognitive achievement, should be included as a component of the
assessment in each required course and clerkship rotation whenever teacher-student
interaction permits this form of assessment.
___________________________________________________________________________________
a.
List the courses in the preclinical phase of the curriculum that include narrative
descriptions as part of the final assessment where the narratives are:
i. provided only to students as a formative assessment
ICM: Introduction to the Patient (mid-year evaluation)
ICM: Introduction to the Patient (reflective writing rubric)
ICM: Introduction to the Patient (case write-ups)
Patients, Doctors & Communities (PDC)
Bioethics 1
ii. used as part of the final grade/assessment in the course
ICM: Clinical Experience (end-of-course evaluation)
ICM: Introduction to the Patient (end-of-course evaluation)
ICM: Clinical Examination (student evaluation – Part I)
ICM: Clinical Examination (student evaluation– Part II)
Patients, Doctors & Communities (PDC)
b. List the clinical clerkship rotations that include a narrative description as part of the final assessment
where the narratives are:
i.
provided only to students as a formative assessment
In all required clinical clerkships in the third and fourth years, there are several opportunities to
provide a narrative description of a student’s performance for use in formative feedback.
First, at mid-cycle feedback meetings (for clerkships of four weeks or longer), the site leader (or
faculty member) providing feedback uses a standard form to document the feedback session, which
includes a section for comments or details of the discussion. Next, all students on required
clerkships > 4 weeks are required to be directly observed by a faculty member during an observed
clinical encounter (OCE). This is used for formative purposes only, and students receive immediate
feedback. The attending must also document the student’s performance on a standard Einstein
form, which includes an area for narrative comments. Finally, on the Evaluation of Clinical
Performance and Professional Attributes form, there is a space for formative feedback, which is
shared only with the student and the Office of Student Affairs. It is not part of the final narrative
used in MSPE letters but provides the opportunity to give private constructive feedback to the
student. The OSA may use this section to monitor for any concerning patterns across clerkships.
.
ED-123
Albert Einstein College of Medicine
Academic Year 2014-2015
ii. used as part of the final grade/assessment in the course
In all required clerkships in the third and fourth year, a narrative assessment is a mandatory
component of the student’s final evaluation form. The narrative includes a compilation of
comments made by supervising residents and faculty, as well as descriptions of the student’s
performance on clerkship-specific, and an overall assessment of the student’s performance.
ii. used as part of the Medical Student Performance Evaluation (MSPE) or Medical Student
Performance Report (MSPR)
The narrative summaries on the final clerkship evaluation form (Evaluation of Clinical
Performance and Professional Attributes form) for all required clerkships are included, with minor
edits, in the student’s MSPE letter to residency programs.
c. Describe any institutional policies that include the requirement for narrative assessment, where
feasible.
Einstein requires that all clerkships provide narrative descriptions on the final clerkship evaluation
form. This form was recreated for the 2013-2014 academic year so that student performance could
be more closely aligned with the Einstein Educational Competencies. Narrative comments include
feedback from many members of the health care team, including attendings and residents.
Clerkship directors are also required to complete a mid-clerkship feedback form, which includes
both a checklist and a narrative section. This form is utilized by the director when meeting with
each student at the mid-point of the clinical rotation.
This policy also applies to the yearlong course, Patients, Physicians and Communities (PDC). This
course meets monthly throughout the third year, for a total of 24 contact hours. Faculty facilitators
provide narrative feedback on each written assignment and also provide narrative comments on a
final written evaluation form. Narrative descriptions focus on professional attributes, motivation
and preparedness, responsiveness to feedback and communication skills.
Narrative descriptions are incorporated into the final evaluation forms for all units of the
Introduction to Clinical Medicine (ICM) courses in both the first and second year, as these courses
provide sufficient student-faculty contact allowing for this type of assessment. In the Introduction
to the Patient course component in year one, small group facilitators spend approximately 45 hours
with 12-14 students during the seven months of the course. The groups meet in the classroom and
clinical settings. The reflective natures of this skill-building course requires faculty to comment on
students’ knowledge, skills and attitudes. The faculty members are encouraged to comment on noncognitive issues relevant to professional development. Students spend about 35 hours over five
months in clinical seating with physician preceptors in the first-year ICM Clinical Experience
course. Preceptors are encouraged to comment on students’ interpersonal/professional
characteristics, including relationship with patients, preceptors and the clinical team, and the
students’ ability to accept direction. In the second year ICM course students meet for 10 afternoons
during the fall semester in groups of 8 with faculty preceptors who teach them physical diagnosis.
In the second semester students go to clinical sites for 11 afternoons to meet in groups of 4 with
faculty preceptors. All of these faculty will create narratives in their assessment of the students.
Beginning in the 2013-2014 academic year, another course with ongoing faculty-student interaction,
the Bioethics 1 course provides formative narrative assessment at mid-course. In this course,
students spend 9.5 hours with one or two small-group faculty leaders over eight months. Since the
course focuses on enabling students to identify ethical issues and on ethical reasoning skills, faculty
ED-124
Albert Einstein College of Medicine
Academic Year 2014-2015
members provide feedback in these areas, as well as on student professionalism. Mid-course
formative narrative assessment will be extended to the Bioethics 2 course for the following year.
Also see information provided on the Required Course and Clerkship Rotation Forms.
ED-125
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-33. There must be integrated institutional responsibility in a medical education
program for the overall design, management, and evaluation of a coherent and coordinated
curriculum.
The phrase "integrated institutional responsibility" implies that an institutional body (commonly a curriculum
committee) will oversee the medical education program as a whole. An effective central curriculum authority will
exhibit the following characteristics:
iii.
iv.
v.
Faculty, medical student, and administrative participation.
Expertise in curricular design, pedagogy, and evaluation methods.
Empowerment, through bylaws or decanal mandate, to work in the best interests of the institution
without regard for parochial or political influences or departmental pressures.
The phrase "coherent and coordinated curriculum" implies that the medical education program as a whole will be
designed to achieve its overall educational objectives. Evidence of coherence and coordination includes the
following characteristics:
Logical sequencing of the various segments of the curriculum.
Content that is coordinated and integrated within and across the academic periods of study (i.e., horizontal and
vertical integration).
Methods of pedagogy and medical student assessment that are appropriate for the achievement of the program's
educational objectives.
Curriculum management signifies leading, directing, coordinating, controlling, planning, evaluating, and reporting.
Evidence of effective curriculum management includes the following characteristics:
Evaluation of program effectiveness by outcomes analysis, using national norms of accomplishment as a frame
of reference.
Monitoring of content and workload in each discipline, including the identification of omissions and unplanned
redundancies.
Review of the stated objectives of each individual course and clerkship rotation, as well as the methods of
pedagogy and medical student assessment, to ensure congruence with programmatic educational objectives.
Minutes of the curriculum committee meetings and reports to the faculty governance and deans should document
that such activities take place and should report on the committee's findings and recommendations.
_________________________________________________________________________________
a. Provide an organizational chart for the management of the curriculum that includes the curriculum
committee and its subcommittees, other relevant committees, the chief academic officer, and other
individuals or groups involved in curriculum design, implementation, and evaluation.
(See ED Appendix T.)
b. Supply the title of the faculty committee with primary responsibility for the curriculum:
Executive Committee of the Medical Education Council (MEC)
c. Provide the charge or terms of reference for this committee and the source of its authority (e.g.,
bylaws, mandate from the dean or faculty executive committee).
In 2010, the dean empowered the new senior associate dean for medical education to analyze the
structure for the management of the curriculum, formerly called the Division of Education (DOE).
A new table of organization based on this analysis was proposed in the spring of 2010 for the
ED-126
Albert Einstein College of Medicine
Academic Year 2014-2015
upcoming academic year. The rational for restructuring was based on a need to streamline, avoid
redundancy, and encourage greater accountability while preserving faculty involvement. The
objectives for the overall reorganization of all committees, subcommittees and task forces within
the organization chart were based on a need to:
Provide centralized oversight and management of the program leading to the MD degree;
Empower committees, sub-committees and task forces to become more action oriented with
clearly defined goals and outcomes;
Define roles and responsibilities for each committee, subcommittee and task force;
Develop a clear table of organization for the committee structure and a method to enhance
communication between all components;
Realign faculty membership to enhance educational goals.
The proposal was presented to the Division of Education Executive Committee in June 2010, and
was approved for the 2010-2011 academic year. The reorganization and reconstitution of all
committees, subcommittees and task forces was organized under the authority of the dean.
The new committee charged with the overall responsibility for the oversight and management of
the curriculum became the Executive Committee of the Medical Education Council (MEC) in July
2010. The charge for the new Executive Committee is as follows:
Provide leadership and direction for centralized oversight and management of the four-year
undergraduate education program;
Review the medical school curriculum, teaching and assessment methods;
Ensure that the content of the curriculum is coordinated and integrated within and across
academic periods of study;
Ensure that appropriate didactic methods are utilized for each course and clerkship;
Ensure the use of appropriate methods to evaluate both student performance and program
effectiveness;
Review the activities of all subcommittees and task forces;
Approve all institutional policies relating to undergraduate medical education;
Provide ongoing review of instructional objectives and competencies;
Approve the academic calendar and curricular changes;
Approve new course directors, clerkship directors, site directors and assistant deans at
affiliated sites;
Review all teaching program outcomes;
Review all outcome measures and develop plans to address findings.
d. Describe the composition of this committee and the mechanisms for selecting its members and chair.
There is a total of 18 members on the Executive Committee, 16 faculty and 2 students. Faculty
members of the Executive Committee are a diverse group representing both basic and clinical
sciences and are chosen for their expertise and extensive involvement in undergraduate medical
education. Nominations for members are solicited by the chair of the Executive Committee in the
spring of each academic year. The standing committee members choose the new members for the
ED-127
Albert Einstein College of Medicine
Academic Year 2014-2015
upcoming year. The Executive Committee is chaired by Dr. Jeffrey Avner, co-director of the
Pediatrics clerkship. All faculty members of the Executive Committee, including the chair, serve for
a three-year term, with an option to serve for a second three-year term.
Additional members include the chairs of three of the standing MEC sub-committees, the chair of
the Faculty Advisory Board, the senior associate dean and assistant dean for medical education, the
senior associate dean and two assistant deans for Student Affairs, and the Dean, who serves exofficio. Two fourth-year student members serving in elected leadership positions are also members
of the Executive Committee. The names of student leaders who have served on MEC committees
for the past few years are reviewed by the current membership of the Executive Committee, and
two students are chosen. Since the students are in their senior year, the student term is for one year.
e. Indicate the frequency of regularly scheduled committee meetings during a typical academic year:
(check)
X
Weekly
Biweekly
Monthly
Bimonthly
Other (describe)
f. If this committee has standing subcommittees, describe their charge or role, membership, and
reporting relationships to the parent committee.
There are four standing sub-committees of the Executive Committee, a Faculty Advisory Board
and five administrative task forces.
Sub-committees of the MEC:
The Course Directors Sub-committee consists of all directors of courses in the first two years, the
chair of the Clinical Directors Sub-committee, and four student elected representatives, two for the
first year and two from the second year. The deans for education, educational information
resources, student affairs and faculty development all serve ex-officio on this committee. The
Course Directors Sub-committee is chaired by Dr. Howard Steinman, assistant dean for biomedical
science education, who also serves as the course director for the Molecular & Cellular Foundations
of Medicine course in year 1. The sub-committee meets monthly.
The Clinical Directors Sub-committee consists of all required clerkship and course directors in the
third and fourth year of medical school, the assistant deans at all university and affiliated hospitals,
the chair of the Course Directors Sub-committee, four student elected representatives, two from
year 3 and two from year 4. The deans of medical education, educational information resources,
student affairs and faculty development also serve in an ex-officio capacity on this subcommittee.
The Clinical Directors Sub-committee is chaired by Dr. Miriam Schechter, who also serves as codirector of the Pediatrics clerkship. The subcommittee meets monthly.
The chairs of both the Course and Clinical Directors Sub-committees sit on the Executive
Committee and report to it. Both are charged with making recommendations to the Executive
Committee and implementing Executive Committee decisions regarding:
ED-128
Albert Einstein College of Medicine
Academic Year 2014-2015
Course/clerkship content
Teaching methodologies
Evaluation and assessment strategies
Scheduling and policies
Faculty development
The Evaluation Sub-committee was chaired since its creation in 2010 by Dr. Penny Grossman, who
also served as assistant dean for educational resources. The committee met 7-8 times per year. As of
October 2013, the committee is chaired by Dr. Terence Ma, currently assistant dean for educational
information resources. The committee consists of six faculty members who are involved with
medical student education but do not currently serve as a course or clerkship directors. For the
academic year 2013-2014, the membership was expanded, medical students will be added to the
subcommittee, and the frequency of the committee meetings has increased to monthly. The assistant
dean for medical education also was named to the sub-committee as a voting member. The charge
for the sub-committee is to develop and revise, as needed, the online course and clerkship
evaluation forms, analyze the ratings and comments completed by students, and summarize
strengths and areas for improvement. The sub-committee will also develop and implement a new
system for the intensive review of required courses and clerkships that was approved by the
Executive Committee. When the new members are chosen, the charge will be reviewed and any
proposed changes will be submitted to the Executive Committee for approval.
The Curricular Themes Sub-committee was created in January 2013 to provide oversight for
educational content themes that will be integrated throughout all four years of medical school. At
present, there is one curricular theme that is being formally addressed in a task force, the Clinical
Prevention and Population Health Task Force, chaired by Dr. Cristina Gonzalez. There are 15
faculty members, three members from the dean’s office and three students on this task force. Its
charge is to develop, assess, and provide oversight for the education in prevention, epidemiology,
community dimensions of medical practice, and health services organization and delivery
throughout the four years of the curriculum. Dr. Gonzalez reports to the Executive Committee
annually. As other curricular themes are approved by the Executive Committee, the theme chairs
will join this sub-committee. Dr. Gonzalez will serve as the chair of this sub-committee as it
expands.
The Faculty Advisory Board (FAB) is a forum that allows for bi-directional flow of information and
ideas between a diverse group of faculty and students and the educational leadership. This monthly
meeting is utilized to update FAB members about educational programs at both the main campus
and affiliated sites. The FAB receives regular reports from MEC committee chairs and task forces.
This group is also used to vet ideas for educational innovations relating to curricular content,
teaching and assessment methods. Chaired by Dr. Barbara Birshtein, the FAB comprises 39 faculty
members and four students, one from each year of medical school. Faculty members are chosen
based on their involvement in medical education, but do not serve as course or clerkship directors.
In the academic year 2012-2013, several course directors requested to join the FAB and were
added. The FAB also has representatives from key offices within the medical school, including
directors or deans from the library, admissions, diversity, faculty development, student affairs,
diversity enhancement, student activities, and graduate medical education. The FAB was put on
hold for the first part of the 2013-2014 academic years, as committee members were all asked to
work on the various committees for the LCME self-study.
Task Forces of the MEC:
ED-129
Albert Einstein College of Medicine
Academic Year 2014-2015
In addition to the above subcommittees, there are five administrative task forces: the Clinical Skills
Assessment Task Force, the Faculty Development Task force, the SOAR (Student Opportunities in
Academic Research) Task Force, the Medical Student Research Task Force and the Educational
Informatics Task Force. The charge for each of these task forces is to monitor and provide
oversight for areas that play a key role in the education of medical students. The chair of each of
these task forces meets monthly with the senior associate dean for medical education, and reports
annually to the Executive Committee. Additional updates and reports are given, as appropriate, to
selected subcommittees and/or the FAB.
The responsibilities of the Clinical Skills Assessment Task Force include making recommendations
for policies and procedures for the end of the third-year Clinical Skills Assessment (CSA), which
takes place at the Clinical Skills Center. The primary purpose of the CSA program is to provide
summative assessments of students’ knowledge and skills across multiple cases reflecting an array
of disciplines. These policies and procedures include setting standards, remediating students who
fail and providing feedback on performance. Proposed recommendations are brought to the
Executive Committee for approval. The task force is chaired by Dr. Felise Milan, who is director of
the Ruth L. Gottesman Clinical Skills Center. There are 11 faculty members from several clinical
departments including medicine, pediatrics, neurology, family medicine, psychiatry and Ob/Gyn.
Members are solicited for their interest and/or expertise in clinical skills teaching and assessment.
The task force meets monthly.
The SOAR Task Force brings together faculty members with vision and expertise in areas of
concentration suitable for medical student research. The task force functions in an advisory
capacity to the Office of Medical Student Research (OMSR) under the auspices of the Office of
Medical Education. It focuses on admission to SOAR, mentor selection, curricular elements and
student project evaluation in order to develop a unified program encompassing each of the distinct
concentrations. The task force meets monthly and is chaired by Dr. Ellie Schoenbaum, the director
of medical student research. The frequency of meetings reflects the fact that this is a new program.
The group comprises the eight faculty members who direct the concentrations and three ex-officio
deans (medical education, research education and student affairs). The administrator of the Office
of Medical Student Research is also a member.
The Medical Student Research Task Force focuses on polices and resources related to medical
student research, research mentoring and the Scholarly Paper requirement. The task force
functions in an advisory capacity to the Office of Medical Student Research under the auspices of
the Office of Medical Education and is co-chaired by Drs. Ellie Schoenbaum and Joan Berman. In
addition, the committee reviews selected scholarly papers and adjudicates the applications for
Einstein Research Fellowships (i.e., for 12 months of dedicated research time). The 13 faculty
members include social scientists, clinical researchers, basic and translational scientists and the
OMSR administrator. The task force meets quarterly except during the spring semester when it has
one or two extra meetings to evaluate scholarly papers and research fellowships.
The former Computer-Based Education Task Force has been renamed the Educational Informatics
Task Force. Members for this task force are currently being selected and will include students,
faculty, and staff from Information Technology Services and Audio-visual Systems. This task force
will meet regularly to review issues of educational technology and develop strategies for the
implementation of instructional technology at the College. The task force will be chaired by Dr.
Terence Ma, Assistant Dean for Educational Information Resources and will function in an
advisory capacity to the Office of Educational Informatics and to the Office of Medical Education.
ED-130
Albert Einstein College of Medicine
Academic Year 2014-2015
The Faculty Development Task Force was established in 2012 to provide oversight of initiatives
related to enhancing the skills and career development of faculty devoted to medical education.
Chaired by Dr. Christina Coyle, assistant dean for faculty development, this task force meets four
times each year and includes 33 faculty members and nine members from the dean’s office. The
task force’s mission also includes evaluating programs and workshops to ensure that they offer
meaningful and useful tools to improve the teaching experience at Einstein. The task force serves in
an advisory capacity to the Offices of Faculty Development and Medical Education.
g. Describe the roles of the curriculum committee and any subcommittees, the chief academic officer or
associate dean for educational programs and their staffs, interdisciplinary course committees (if relevant),
and the departments in each of the following areas:
i. Developing and reviewing the institutional objectives for the educational program
A time-limited task force, appointed by the dean, was charged with developing a new set of
educational competencies for the program leading to the MD degree. The chair of the task force
was Dr. Julia Arnsten, chief of the division of general internal medicine. Members were chosen
based on their expertise in areas that were deemed critical for preparing students for the future
practice of medicine. Task force members represented the basic and clinical sciences and key
affiliated institutions; the senior associate dean for medical education served as staff to the task
force. The task force met monthly beginning in September 2011, and the set of Einstein
Educational Competencies was approved in October 2012. The Executive Committee of the
MEC is charged with the ongoing review of the competencies and sub-competencies
(objectives).
ii. Reviewing the objectives of individual courses and clerkship rotations to ensure that they
are written in competency-based/outcomes-based terms
The Office of Medical Education is charged with ensuring that all objectives are written in
competency-based/outcome-based terms. A member from the office and an educational
specialist worked with each course and clerkship director to edit their objectives (as needed)
and link them to the new competencies.
iii. Ensuring that course and clerkship objectives are linked to the educational program
objectives
After the approval of the Einstein Educational Competencies, the next step was to introduce
them to key faculty, and ensure that all course and clerkship objectives were mapped to the
competencies. The annual Davidoff Education Day, on January 25, 2013, was used for this
purpose. During the afternoon session, course and clerkship directors began the process of
linking the objectives to the overall educational program, under the guidance of faculty
members that had served on the Educational Competency Task Force and members of the
Office of Medical Education. Directors continued to work with the senior associate dean for
medical education and a specialist in education to further refine course and clerkship
objectives, which were put in place for the 2013-2014 academic year.
iv. Ensuring the use of appropriate teaching methods or instructional formats
The MEC and its sub-committees, the Course Directors, the Clinical Directors, and the
Evaluation Sub-committees, are all involved in discussing the appropriateness and effectiveness
of teaching methods and strategies for piloting new methods. All course and clerkship
evaluation forms have questions relating to teaching methods and instructional formats. The
Evaluation Sub-committee reviews the annual course and clerkship evaluations, and a
summary of strengths and areas for improvement is sent to the directors for their response.
Each course and clerkship director presents the findings and their responses to the appropriate
ED-131
Albert Einstein College of Medicine
Academic Year 2014-2015
sub-committee. Any proposals for utilizing new formats are brought to the Executive
Committee. With the scheduled opening of the new Educational Center in 2014-2015, there will
be a new initiative to convert some of the traditional classroom experiences to one or more
variations of the “flipped classroom,” including team-based learning and “just-in-time”
learning. The senior associate dean for medical education has a budget to send faculty to
meetings and workshops focusing on new pedagogical methods. There is also a competitive
internal grant process, the Grants for Excellence in Medical Education (GEME) program
administered by the Office of Medical Education, that provides stipends for 5-10 faculty
members who have submitted worthy proposals for piloting new formats for teaching.
v. Ensuring that content is coordinated and integrated within and across academic periods of
study
The Executive Committee and sub-committees of the MEC are responsible for ensuring that
there is appropriate horizontal and vertical integration of curricular content within and across
academic periods of study. All course and clerkship reviews by the Evaluation Sub-committee
are presented to the sub-committee responsible for that part of the curriculum. The Course
Directors Sub-committee provides oversight for horizontal integration in the first two years,
and the Clinical Directors Subcommittee for the third and fourth years. The implementation of
“The Einstein 203,” the patient log implemented for the academic year 2013-2014, ensures that
all medical students experience the same conditions and procedures in the clinical years, a
process that has greatly contributed to the coordination of content among clerkships.
All course and clerkship directors are granted “administrative rights” to the learning
management system, eMED. This allows them to search educational content and edit materials
in their courses or clerkships based on coverage throughout the curriculum. Starting with the
academic year 2013-2014, all directors must submit in writing any proposals for the addition or
deletion of significant content within their course and clerkships on their course review forms.
These proposals are reviewed by the senior associate dean for medical education and, if deemed
significant, are brought to the Executive Committee for approval.
vi. Ensuring the use of appropriate methods to assess student performance
The Executive Committee and sub-committees of the MEC are responsible for ensuring that
appropriate methods are utilized for assessing student performance. The Course Directors Subcommittee monitors and makes recommendations for the courses in the first two years, and the
Clinical Directors Sub-committee for the clinical rotations. The Clinical Directors Subcommittee created a new Evaluation of Clinical Performance and Professional Attributes form
mapped to the competencies, as well as a new grading scale, both of which were implemented in
2013-2014. Faculty development sessions organized by the Offices of Faculty Development and
Medical Education are designed to keep faculty members up to date on the latest tools for
assessment.
vii. Monitoring the quality of individual faculty members’ teaching
The on-line course and clerkship evaluations completed by every student at the end of all
courses and clerkships have questions pertaining to the quality of teaching by individual faculty
members. The statistical data and comments for each course or clerkship are shared with the
course or clerkship director, the department chair, the Evaluation Sub-committee and the
senior associate dean and assistant dean for medical education. The course and clerkship
directors have the ongoing responsibility for ensuring the quality of teaching within their
courses and counseling faculty members with unsatisfactory ratings. Ongoing faculty
development sessions on teaching methods are offered by the Office of Faculty Development.
ED-132
Albert Einstein College of Medicine
Academic Year 2014-2015
viii. Monitoring the overall quality and outcomes of courses/clerkship rotations
The overall quality and outcomes for each course and clerkship are monitored at the annual
review by the Evaluation Subcommittee (See ED-35). The strengths and areas for improvement
are identified, and this information is presented to the respective sub-committee, either the
Course Directors or Clinical Directors.
ix. Monitoring the outcomes of the curriculum as a whole
The ultimate responsibility for the monitoring of the outcomes of the curriculum rests with the
Executive Committee of the MEC. Information from all MEC sub-committees and the Office of
Medical Education is brought to this committee. All internal measures, such as course/clerkship
evaluations, student surveys and performance on internal exams, and external measures, such
as the results of the AAMC GQ and performance on NBME exams, are reviewed.
ED-133
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-34. The faculty of a medical education program must be responsible for the detailed
design and implementation of the components of the curriculum.
Faculty members’ responsibilities for the medical education program include, at a minimum, the development of
specific course or clerkship rotation objectives, selection of pedagogical and assessment methods appropriate for the
achievement of those objectives, ongoing review and updating of content, and evaluation of course, clerkship
rotation, and teacher quality.
___________________________________________________________________________________
Provide examples of the types of changes that can be implemented at the level of the course or clerkship
rotation and the types of changes that require curriculum committee or other central approval prior to
implementation.
Directors and faculty are encouraged to be creative and integrate innovative instructional and
assessment methods into course and clerkships. Any innovations or changes are submitted on the
annual director’s response to the Evaluation Sub-committee. The senior associate dean for medical
education reviews the proposed change and if deemed significant, it is forwarded to the Executive
Committee for review and discussion.
Examples of changes at the central level:
Requested changes in course hours or length of clerkships.
Changes of a major content area for a course or clerkship.
A change to the current grading rubric for the course or clerkship, including the addition,
deletion, timing or frequency of summative exams.
Request for introduction of a new teaching method or changes to an existing teaching
method.
Changes in methods to evaluate student performance.
Approval of new course directors, clerkship directors, clinical sites, site directors and
assistant deans at affiliated sites.
Approval of new required courses, clerkships, electives or thematic programs.
Approval of any requested changes to the patient logs (“Einstein 203”) involving conditions,
procedures, level of student responsibilities, alternate experiences, the clinical setting for
each educational experience, the number of patients required to pass a clerkship, or any
changes to logging policies and procedures.
Examples of changes at the course and clerkship level:
Annual revision of goals and objectives for the course/clerkship.
Changes in the sequence of content within a course or clerkship.
Updating content on an annual basis for the course/clerkship.
The introduction of a new topic occurring within an individual teaching session (e.g.,
didactic or small group session).
Changes in the required reading materials and resources for a course/clerkship.
Changes in faculty members and other non-faculty instructors who teach in individual
instructional sessions.
Changes in specific clinical services available to students within a clinical site (e.g., removal
or addition of a hospital sub-specialty unit or ward).
Also see the information for standards ED-33 and ED-46/47.
ED-134
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-35. The objectives, content, and pedagogy of each segment of a medical education
program’s curriculum, as well as of the curriculum as a whole, must be designed by and
subject to periodic review and revision by the program’s faculty.
________________________________________________________________________________
a. Describe the process of formal faculty review for each of the listed curriculum elements. Include in
the description the frequency with which such reviews are conducted, the means by which they are
conducted, under whose auspices (e.g., the department, the curriculum committee) they are reviewed, the
administrative support that exists for such reviews (e.g., through an office of medical education), and the
individuals and groups (e.g., the curriculum committee) that receive the results of the evaluations.
i. Required courses
ii. Required clerkships / clerkship rotations
All required courses and clerkships undergo the same review process. This process was instituted in
November 2013 to supplement the previously existing process. There are two phases for
evaluations. In Phase 1, each course and clerkship is reviewed yearly by the Evaluation Subcommittee, a standing committee of the Medical Education Council (MEC). In Phase 2, each course
and clerkship is reviewed every four to five years by ad hoc task forces organized by the Assistant
Dean for Educational Information Resources.
The membership of the Evaluation Sub-committee consists of:
Terence Ma, PhD, Assistant Dean for Educational Information Resources, Chair.
William Burton, PhD, Associate Director for Educational Resources.
Pablo Joo, MD, Assistant Dean for Medical Education.
Rachel Katz, MD, Associate Professor of Clinical Pediatrics.
Herbert Lachman, MD. Professor of Psychiatry and Behavioral Sciences and Medicine
(Hematology).
Hannah Lipman, MD, Associate Professor of Clinical Medicine (Geriatrics).
Fernando Macian-Juan, Associate Professor of Pathology
Zoon Naqvi, MBBS, Assistant Professor of Family Medicine.
Sheira Schlair, MD, Assistant Professor of Medicine (General Internal Medicine).
Two medical students.
Allison Ludwig, MD, Assistant Dean for Student Affairs, ex officio.
The membership of Phase 2 review committees consists of:
One member of the Executive Committee of the MEC
One course director
One clerkship director
One member of the Evaluation Sub-committee
One member from the Office of Student Affairs
One member selected from a list provided by the Office of Medical Education.
A new review committee is selected for each Phase 2 review.
Phase 1 Reviews:
ED-135
Albert Einstein College of Medicine
Academic Year 2014-2015
The goal of these annual reviews is to provide an overview of the strengths and areas need
improvement in a particular course or clerkship and evaluate how well the course or clerkship
has addressed the competencies identified in the course or clerkship. Additionally, for
clerkships, the review assesses how well the clerkship has met the requirement for
comparability of student experiences across clerkship sites.
Evaluations for courses are posted for student response at the time of the final examination or
predetermined major examination in each course. Students are required to complete the
evaluations as part of their course obligations within two weeks after the end of the course.
Once course obligations are completed, their exam score and/or course grade will be released to
the student. Within this construct, student response rate is near 100% for every course. If a
student does not complete a course evaluation within the allowed period, he/she is referred to
the Office of Student Affairs, which works with the student to ensure compliance with this
course obligation. In the unlikely event that a student fails to complete a course evaluation by
two weeks after the end of the course, that student receives a grade of Incomplete for the course
until the Office of Student Affairs has determined that a resolution has been met.
Evaluations for clerkships are posted for student response on the final day of the clerkship,
which usually coincides with the scheduling of the shelf exam. Students are required to
complete the evaluations as part of their clerkship obligations. Once clerkship obligations are
completed, the shelf exam score and/or clerkship grade will be released to the student. Within
this construct, student response rate is near 100% for every clerkship. If a student does not
complete a clerkship evaluation within the allowed period, he/she is referred to the Office of
Student Affairs, which works with the student to ensure compliance with this clerkship
obligation. In the unlikely event that a student fails to complete a clerkship evaluation by six
weeks after the end of the clerkship, that student receives a grade of Incomplete for the
clerkship.
Course/clerkship evaluations are supported by the staff of the Office of Educational Resources,
an office under the Office of Medical Education reporting to the assistant dean for educational
information resources.
Upon close of course evaluations, the Office of Educational Resources provides the raw data
(frequencies and means of numerical items, and a complete listing of student comments) to each
course/clerkship director for review. Twice each year, the Office of Educational Resources
provides the raw data (frequencies and means of numerical items, and a complete listing of
student comments) to each clerkship director for review. The raw data, some basic analyses,
copies of the Evaluation Sub-committee reports for that course or clerkship from the previous
three or four years, the course/clerkship objectives, the mapping of course/clerkship objectives
to the Einstein Educational Competencies, the annual site comparability report (for clerkships),
and any additional data required for the review are provided to the members of the Evaluation
Sub-committee. One faculty member of the sub-committee is selected as the primary reviewer
and generates a draft report. The sub-committee will review the course/clerkship using the
draft report and produce a final consensus approved report that is provided to the
course/clerkship director and to the Course or Clinical Directors Sub-committee, as
appropriate. The course/clerkship director responds to the report in his/her respective subcommittee and documents any proposed changes in the curriculum for review.
Phase 2 Reviews:
ED-136
Albert Einstein College of Medicine
Academic Year 2014-2015
Beginning in the 2014-2015 academic year, the Executive Committee of the MEC will determine
which courses and clerkships are to be reviewed. The goal is to review every course and
clerkship every four to five years. The assistant dean for educational information resources,
working with the chair of the Executive Committee of the MEC, selects the members of each
task force.
The Office of Educational Resources provides the review committee with the raw data for the
course/clerkship since its last review, the Evaluation Sub-committee reports and
course/clerkship director’s responses, data related to the course/clerkship from USMLE Step 1,
Step 2, Step 3, as appropriate, data related to the course/clerkship from the AAMC Graduation
Questionnaire and the Program Directors Surveys, student performance on standardized
patient assessments, NBME shelf examination results, and any other pertinent information.
The review committee analyzes the data, meets with the course/clerkship director, and delivers
a written report to the Executive Committee of the MEC focused on the trends in student
performance in the course/clerkship, the comparison with national norms, identified strengths
and weaknesses, identified gaps and overlaps, and student outcomes for the Einstein
competencies in that course. The Executive Committee of the MEC will discuss and review the
report and take appropriate actions as necessary.
iii. Individual years or segments of the curriculum
Segments of the curriculum – preclinical and clinical – are reviewed annually. The Office of
Educational Resources is responsible for collecting, reviewing, analyzing, and disseminating
information to the Executive Committee and relevant subcommittees of the Medical Education
Council (MEC) and to the Office of Medical Education.
Each year, students who have just taken USMLE Step 1 are surveyed to identify areas of
strength and weaknesses in their education and preparation for USMLE Step 1. Additionally,
the results of the Step 1 examination and its subcomponents are analyzed, summarized, and
reviewed by the Office of Educational Resources. These data are used to inform the Course
Directors Subcommittee of areas in which students have performed well or showed deficiencies
within the preclinical curriculum. The Course Directors Subcommittee and the Executive
Committee of the MEC discuss these results to assess what modifications might be required in
the curriculum.
Near the end of the third year, students participate in an all-day Clinical Skills Assessment
(CSA) using standardized patients. The results of this assessment are used to determine the
effectiveness of our clinical skills educational programs. Additionally, the results of USMLE
Step 2 (CK and CS), the clerkship reviews in the AAMC Graduation Questionnaire, and the
results of the annual Program Directors Survey are used to inform areas of strength and
deficiency in the clinical curriculum. These data are reviewed by the Clinical Directors Subcommittee to assess what modifications might be required in the curriculum.
iv. The entire curriculum
The curriculum as a whole is reviewed on a regular basis. Each year, the results of the AAMC
Graduation Questionnaire are reviewed in detail by the Executive Committee of the MEC. We
recognize that the GQ contains information that lags behind curricular changes that were
implemented on the basis of course/clerkship evaluations performed by the Evaluation Subcommittee, the Course/Clinical Directors Sub-committees, and by the Executive Committee of
ED-137
Albert Einstein College of Medicine
Academic Year 2014-2015
the MEC. Thus, the annual review takes both prospective and retrospective views of courses
and clerkships to identify areas of strength and weakness.
Additionally, the senior associate dean for medical education and the Office of Medical
Education perform ongoing review of the curriculum in terms of individual courses, and
identification of gaps and overlaps across the curricular content. Course/clerkship directors
meet regularly with the members of the Office of Medical Education to discuss curricular
modifications to meet the needs of our students.
Lastly, there are several task forces that are formed around educational themes that the
Executive Committee or the Course/Clinical Directors Subcommittees of the MEC have
identified as areas of weaknesses. These task forces develop recommendations of how the
content can be incorporated into the courses and clerkships. For example, students identified
that they needed more dermatology content in their preclinical coursework. A task force was
established by the Course Directors Subcommittee to identify areas where dermatology content
can be strengthened in the preclinical curriculum. Similarly, through analysis of the
Graduation Questionnaire and other data, the Office of Medical Education recognized that
there was a gap in the information provided to our students regarding population health and
practice of medicine. The Executive Committee of the MEC established a task force whose
mandate is to develop an integrated theme about population health and practice of medicine
into the four-year medical school curriculum.
Major curricular changes must be reviewed and approved by the Executive Committee of the
MEC prior to implementation.
b. Provide an electronic copy of any standardized templates used for course and clerkship rotation
reviews in the Appendix. Also include an electronic copy of a sample review of a course or clerkship in
the Appendix.
ED Appendix U includes:
Standard course evaluation form
Standard clerkship evaluation form
Lecturer Evaluation form
Small group facilitator evaluation form
Clinical teaching evaluation form (clerkships)
Clinical teaching evaluation form (ICM)
ED Appendix V includes:
Sample Phase 1 Course review – Histology 2013-3014.
Sample Phase 2 Course Review - Histology
Also see information for standards ED-33, ED-46, and ED-47.
ED-138
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-36. The chief academic officer of a medical education program must have sufficient
resources and authority to fulfill his or her responsibility for the management and
evaluation of the curriculum.
The dean often serves as the chief academic officer, with ultimate individual responsibility for the design and
management of the medical education program as a whole. He or she may, however, delegate operational
responsibility for curriculum oversight to a vice dean or associate dean.
Examples of the kinds of resources needed by the chief academic officer to ensure effective delivery of the medical
education program include:
Adequate numbers of teachers who have the time and training necessary to achieve the medical education
program's objectives.
Appropriate teaching space for the methods of pedagogy employed in the medical education program.
Appropriate educational infrastructure (e.g., computers, audiovisual aids, laboratories).
Adequate educational support services (e.g., examination grading, classroom scheduling, faculty training in
methods of teaching and assessment).
Adequate support and services for the efforts of the curriculum management body and for any interdisciplinary
teaching efforts that are not supported at a departmental level.
The chief academic officer must have explicit authority to ensure the implementation and management of the
medical education program and to facilitate change when modifications to the curriculum are determined to be
necessary.
_______________________________________________________________________________
a. Provide the name and title of the chief academic officer responsible for the medical education
program. If the dean has delegated responsibility for the medical student educational program to an
associate dean or other individual, provide the name and title of the latter individual.
Name:
Title:
Martha S. Grayson, MD
Senior Associate Dean for Medical Education
b. Provide a position description for the individual responsible for the medical education program
leading to the M.D. degree, if this person is not the dean. Include the percent of time this individual
devotes to management of the medical education program.
The senior associate dean for medical education is responsible for the oversight of the educational
program leading to the MD degree. Dr. Martha Grayson is supported full-time and devotes roughly
80% of her time to management of the educational program. She is a general internist and devotes
20% of her time to clinical activities and teaching. She reports directly to the dean and works
closely with the senior leadership within the dean’s office. Her responsibilities include:
1) Providing leadership, guidance, and support for the development, implementation, and
evaluation of the College of Medicine’s educational competencies and curriculum, including
courses, clerkships, interdisciplinary themes, and extracurricular academic programs.
2) Providing leadership, guidance, and support for the development, implementation, and ongoing
evaluations of methods utilized for teaching and student assessment.
3) Ensuring that faculty has sufficient expertise and protected time to carry out their educational
responsibilities, and that faculty development programs align with the educational program.
ED-139
Albert Einstein College of Medicine
Academic Year 2014-2015
4) Ensuring that appropriate technological support, educational infrastructure, and educational
space are available to meet educational responsibilities.
5) Ensuring that course and exam scheduling are in alignment with overall educational goals.
6) Developing and managing a budget for all of the units within the Office of Medical Education
(see “c” below).
7) Collaborating with the Office of Institutional Advancement, the Office of Alumni Relations, and
the Department of Communications and Public Affairs to enhance philanthropic support for
educational resources and physical facilities.
c. Briefly describe the infrastructure that is under the authority of the chief academic officer (e.g., an
office of medical education) whose primary purpose is to provide administrative or academic support for
the planning, implementation, evaluation, and oversight of the curriculum. List the individuals, with their
titles, in this administrative structure and the percent FTE contribution of each individual to this effort.
Note the reporting relationships of the director(s) of any such office.
The Office of Medical Education (OME) provides centralized oversight for planning, implementing,
and evaluating the curriculum. In addition to Dr. Grayson, there is an assistant dean for medical
education, Dr. Pablo Joo, who works closely with the senior associate dean on the overall
educational program and selected educational projects. Dr. Joo is a family physician and receives
.75 FTE support for his work within the office. There also is a full-time senior administrator
responsible for preparing the budget, monitoring expenditures, coordinating personnel issues,
ensuring ongoing compliance with regulatory requirements, guiding staff in the annual
performance review process, and training staff on new university sponsored administrative
programs. There are two full-time administrative assistants for the Office of Medical Education.
The assistant dean for biomedical science education, Dr. Howard Steinman, reports to the senior
associate dean for medical education and devotes 20% of his time to oversight and strengthening of
the teaching of biomedical science during the first and second years. He also assists basic science
course leaders in efforts to improve instructional strategies and knowledge assessments.
We are currently recruiting to fill a vacancy for another assistant dean, reporting to the senior
associate dean for medical education, who will be supported 100% by the Office of Medical
Education. The responsibilities will include working with faculty to: a) promote active learning
instructional methods that will be utilized in new state-of-the-art large- and small-group active
learning studios and b) design medical education research projects for enhancing competencybased outcomes.
Other components of the Office of Medical Education are the following:
Ruth L. Gottesman Clinical Skills Center
Dr. Felise Milan, director of the Ruth L. Gottesman Clinical Skills Center (CSC), who is
supported 75% by the Office of Medical Education, reports to the senior associate dean for
medical education. The CSC serves the medical school by providing a setting for clinical
skills training and assessments that span all four years of school. The CSC provides a
simulated clinical setting for formative assessments of students. The Office of Medical
Education also provides 100% support for an assistant director and an administrator of the
CSC.
Office of Diversity Enhancement
ED-140
Albert Einstein College of Medicine
Academic Year 2014-2015
Dr. Yvette Caldron, the associate dean for diversity enhancement and an emergency
medicine physician, is supported 10% and reports to the senior associate dean for medical
education. The Office of Diversity Enhancement’s objective is to provide an environment of
diversity, professionalism, and excellence for the students at the College of Medicine.
Functions of the office include: recruitment efforts that increase the number of the qualified
underrepresented students who demonstrate a commitment to the excellence, integrity, and
dedication to providing the best health care; provide pipeline initiatives for the Bronx
community, like the Einstein Enrichment Program; academic monitoring that ensures early
identification of students requiring academic resources; and develop student leadership
initiative, which fosters academic success and provides career development support. Ms.
Nilda Soto, the assistant dean for diversity enhancement who is 100% supported, focuses on
recruitment efforts for the pipeline programs. Dr. Maria Marzan, director of the
Community-Based Service Learning program (CBSL) is .5 FTE. The office also has one
full-time assistant and one full-time administrator, as well as two program coordinators,
one .8 FTE and one .3 FTE. Dr. Melvin Stone, an associate professor of clinical surgery, is a
part-time advisor offering guidance and support to underrepresented minority students.
Offices of Educational Informatics & Educational Resources
Dr. Terence Ma, assistant dean for educational information resources, is fully supported by
the Office of Medical Education and reports to the senior associate dean for medical
education. Dr. Ma directs both the Office of Educational Informatics and the Office of
Educational Resources. A manager and two professionals devoting 100% of their time
comprise the Office of Educational Informatics, whose functions include: developing and
maintaining electronic learning and curriculum management systems; dealing with all
matters pertaining to acquisition and applications of information technology to teaching
and assessment at all levels of the curriculum; educating and providing guidance to faculty
in uses of information technology in their teaching; managing computer-based testing for
courses and clerkships. The Office of Educational Resources organizes and manages
student evaluations of all courses and clerkships, develops annual reports for each course
and clerkship, and prepares global evaluation reports using current and historical data.
The Office of Medical Education provides 100% support for an associate director and two
administrators to this department.
Office of Faculty Development
Dr. Christina Coyle, assistant dean for faculty development, is supported 20% by the Office
of Medical Education and reports to the senior associate dean for medical education.
Functions of the office include: planning, developing, organizing, and implementing
programs that aim to improve faculty teaching and assessment skills. In addition, the Office
of Faculty Development manages a career development series of workshops that provides
skills necessary for academic promotion. The office also runs full-day events that offer
faculty the opportunity to hear about the latest innovations in medical education and
presents inspirational speakers to discuss career development topics. One full-time
administrative coordinator is supported 100% by the Office of Medical Education.
Office of Instructional Support Services
Ms. Ingrid Brown, the office director who reports to the senior associate dean for medical
education, is supported full-time. Functions of the office include: providing logistical
support for uploading basic science course material into eMED, Einstein’s learning
management system; preparing draft course and exam schedules for first- and second-year
students; managing the electronic version of the course schedules in eMED; overseeing
ED-141
Albert Einstein College of Medicine
Academic Year 2014-2015
classroom/lab scheduling via the online reservation system; managing the setup of
classrooms and labs used in basic science courses; scheduling proctors for exams; providing
to course directors item analyses and summary reports of student performance on
assessments; preparing the make-up exam schedules; and scoring basic science course
examinations using ExamSoft. Ms. Brown is the Executive Chief Proctor for NBME
examination services at Einstein. Three full-time professionals as well as one administrator,
100% paid by the Office of Medical Education, provide support for this office.
Office of Medical Student Research
Dr. Ellie Schoenbaum, Professor of Epidemiology and Population Health, is the director of
this office. She reports to the senior associate dean for medical education and devotes 75%
of her time to this program. Dr. Schoenbaum oversees student research fellowship
programs, including Summer Research, Senior Research, and Einstein Research. One fulltime administrator and one .5 FTE secretary are supported by the Office of Medical
Education.
Global Health
Jill Raufman, an associate in the Department of Pathology, is the director and devotes 30%
of her time to managing the Global Health Fellowship. In this role she reports to the senior
associate dean for medical education. The Global Health Fellowship programs were
established to encourage Einstein students to participate in clinical, public health or
research experiences in less developed and emerging nations in order to gain deeper
understanding of how economic and sociocultural factors influence the health of individuals
and populations; acquire knowledge about diseases that are unique or especially prevalent
in these nations; and obtain insight into the organization and effectiveness of these nations'
health care delivery and public health systems.
d. Indicate whether there is a specific budget for the medical education program. If so, describe how
the budget is determined and how and by whom the budgeted funds are allocated to departments and/or
individual faculty. Note if this funding allocation is done according to a formula (e.g., based on the
amount of teaching done by a department) or is based on some other method.
The senior associate dean for medical education allocates the budget to the different departments
that report to the Office of Medical Education. The budget for the Office of Medical Education is
partially determined based on prior years’ histories. Adjustments and enhancements to the
educational mission based upon updated compliance requirements also inform the budget process.
In addition, new technologies and innovations within the curriculum as well as extra-curricular
academic programs factor into the operating budget. Salary support for course and clerkship
directors is provided based on the type and length of course and clerkship.
Also see information for standards ED-33 and ED-35 and Required Course and Clerkship Rotation
Forms.
ED-142
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-37. A faculty committee of a medical education program must be responsible for
monitoring the curriculum, including the content taught in each discipline, so that the
program's educational objectives will be achieved.
The committee, working in conjunction with the chief academic officer, should ensure that each academic period of
the curriculum maintains common standards for content. Such standards should address the depth and breadth of
knowledge required for a general professional education, the currency and relevance of content, and the extent of
redundancy needed to reinforce learning of complex topics. The final year should complement and supplement the
curriculum so that each medical student will acquire appropriate competence in general medical care regardless of
subsequent career specialty.
__________________________________________________________________________________
a. Describe the frequency with which and the means by which curricular content is monitored and the
ways in which the results of the monitoring are used.
The Medical Education Council (MEC) is responsible for monitoring the medical education
program and reviewing the curriculum. The Executive Committee of the MEC, which meets
monthly for two hours, provides leadership and direction for centralized oversight and
management of the four-year undergraduate education program. This committee is composed of a
diverse group of medical school faculty members (representing both basic science and clinical
clerkships) who have demonstrated longstanding experience and commitment to the medical
student education program. There are also two student members who have previously served on
other MEC committees. In addition, there are several administrative faculty on the committee
representing the offices of student affairs, medical education, and educational resources.
Additionally, the dean of the medical school is a standing member of the Executive Committee. The
Committee is chaired by one of the faculty members all of whom serve a 3-year term that can be
renewed once.
The Executive Committee has a variety of functions including:
1. Review the medical school curriculum, teaching and assessment methods;
2. Ensure that the content of the curriculum is coordinated and integrated within and across
academic periods of study;
3. Ensure that appropriate didactic methods are utilized for each course and clerkship;
4. Ensure the use of appropriate methods to evaluate both student performance and program
effectiveness;
5. Review the activities of all sub committees and task forces;
6. Approve all institutional policies relating to undergraduate medical education;
7. Provide ongoing review of instructional objectives and competencies;
8. Approve the academic calendar in curricular changes;
9. Approve new course, directors, clerkship directors, site directors and assistant deans at
affiliated sites
The curriculum is reviewed by the Executive Committee in a variety of ways. The committee
reviews all teaching program outcomes and other outcome measures and develops plans to address
curriculum needs, redundancy, integration, development and innovation. Results of these standard
outcome measures, including but not limited to the Graduation Questionnaire, Step 1, Step 2-CS,
Step 2-CK, clerkship subject examinations, internal course and clerkship evaluations by the
students, program director’s surveys of graduated students who are now interns, and the match
ED-143
Albert Einstein College of Medicine
Academic Year 2014-2015
results. Based on the results of these outcomes, part of the monthly meetings may be devoted in
part to a presentation and discussion of a major curricular initiative or a focused review of a
particular course or clerkship. These reviews constitute one of the ways that the curriculum is
monitored by the committee.
Another method of curriculum oversight occurs during the annual review of each course and
clerkship. Each course and clerkship director is given a summary of their respective student
evaluations and comments prepared by the Evaluation Sub-committee under the auspices of the
Office of Educational Resources. The course/clerkship director then presents these findings to the
respective sub-committee (i.e., Course Directors or Clerkship Directors sub-committee) with a
review of proposed changes or modifications to address particular strengths or weaknesses in the
manner that the curriculum is covered. This past year, The Executive Committee modified the
form to include any proposed changes in the curriculum content of the course/clerkship as well as
any planned curricular innovations. Any proposed modifications would then be approved by the
Executive Committee.
Monitoring of the details of each course/clerkship curriculum is also done at the level of the Course
or Clerkship Directors Sub-committees. The chairs of these subcommittees, as well as the chair of
the Evaluation Sub-committee, are members of the Executive Committee and serve as liaisons for
specific curricular discussions. The minutes of all of the MEC Committees are available to
members of all the committees in order to assure faculty input into the discussion of all educational
activities.
As noted above, the Executive Committee also approves new course directors, clerkship directors,
site directors and assistant deans at affiliated sites. This process involves a proposal to the
Executive Committee by the leadership of the respective course or clerkship. New clinical sites are
reviewed by a team of Executive Committee members to ensure that the curricular content
required for that clerkship can be met by the new site. The site is then proposed to the full
Executive Committee for review and approval.
b. If there is a curriculum database, describe what is included in it. List the titles of individuals who
have access to it and those who have responsibility for monitoring and updating its content. Note which
individuals, committees, and units (such as departments) receive the results of the reviews of curriculum
content.
eMED is Einstein’s learning management system and curriculum database used to support faculty
and students in teaching and learning. eMED provides a portal to an integrated body of knowledge
and ways to personally organize the array of health information through its online curricular
materials and related applications. eMED is Einstein’s version of TUSK (Tufts University Sciences
Knowledgebase), which allows for a comprehensive platform to maintain tools in the areas of
curriculum management, course management, content management, clinical teaching, personalized
knowledge management and student/faculty management.
All appropriate educational content is uploaded into the eMED database, allowing users to access
and search for existing content across the curriculum. For the pre-clinical years, this includes
course hours, structure, objectives, PowerPoint presentations, outlines, handouts, related articles,
lecture capture presentations, audio presentations, associated images, review materials and other
related educational content. In the clinical years, this includes clerkship objectives, hours, sites and
site leaders, contact information, clerkship requirements, handouts, lecture notes, write-up
examples, evaluation methods, evaluation tools and other educational related information.
ED-144
Albert Einstein College of Medicine
Academic Year 2014-2015
Customized patient-encounter logs that are devised to help monitor the curriculum requirements at
all the clinical sites are based in eMED.
Students can personalize their tools for learning medical content by maintaining and managing
their own folders of educational resources, e.g., slides, handouts, images or other content. Flash
cards can also be created if needed. Students can also review the PowerPoint slides of each lecture
and use the notes feature to record their notes and then save them in their own database. Students
can add notes to individual pieces of content or to folders of content.
eMED is maintained by the Office of Educational Informatics in conjunction with the Office of
Medical Education. In addition to the deans in OEI and OME, administrative rights are granted to
course and clerkship directors, who can edit or change content material for their respective
course/clerkship and are responsible for monitoring and updating the content. Once registered,
Einstein faculty have the ability to access educational content on eMED. Students in each year have
access to all the educational content relevant to their particular year of training.
Discussion of curricular content and review are detailed in committee minutes and are made
available all MEC committee members, to assistant deans at each clinical site, and to all course and
clerkship directors. In addition, department chairs are provided with results and reviews of their
respective clerkships.
c. Describe how the monitoring of curriculum content is used to identify gaps and unwanted
redundancies and to support horizontal and vertical curriculum integration (e.g., through longitudinal
content themes). Provide one or more recent examples of changes that were made to curriculum content
as a result of such monitoring.
The monitoring of the medical school curriculum by the Executive Committee in late 2011
identified certain redundancies and deficiencies in the curriculum regarding the ability of medical
students to identify and define the distribution and determinants of disease and to locate, interpret,
and implement research results. This was also highlighted by in the 2011 GQ, where 20-30% of the
Einstein students reported that there was inadequate instruction in the areas of Epidemiology,
Biostatistics and Public Health. In light of these findings, the Executive Committee charged the
course leaders of the Principles of Preventive Medicine and Clinical Research and the EvidenceBased Medicine courses to review their curricula. At the December 2011 Executive Committee
meeting, they proposed a formal integration of the two courses into a single, two-year course,
ensuring a comprehensive, developmentally appropriate approach to population health and
evidence-based medicine in the pre-clinical curriculum. They proposed renaming the course,
Epidemiology, Population Health, and Evidence-based Medicine (EPHEM), with the first- and
second-year courses named EPHEM 1 and EPHEM 2, respectively.
The goal of EPHEM 1 is to introduce students to the science of preventive medicine and clinical
research methods, providing a foundation that will enable them to become critical consumers of the
medical literature. Basic methodology of epidemiology and biostatistics are introduced from the
perspective of population-based approaches to preventive medicine and public health/prevention.
The application of population-based evidence to the care of individual patients is introduced as a
base for EPHEM 2. The goal of EPHEM 2 is for students to acquire the tools needed to locate and
critically appraise the medical literature, interpret the results, apply these results to the care of
individual patients, and communicate them to patients.
The Executive Committee reviewed the details of the course objectives, curriculum components,
teaching methodology and evaluation. An EPHEM Course Advisory Committee was proposed and
the members were reviewed. Finally, formal course status for EPHEM was approved by the
ED-145
Albert Einstein College of Medicine
Academic Year 2014-2015
Executive Committee, allowing for its own assessment and evaluation, grade, and place on the
transcript.
Another area recently identified by the Executive Committee through review of the curriculum was
a gap in addressing the domains related to core competencies in disease prevention and health
promotion. As a result, the Executive Committee charged the Clinical Prevention & Population
Health Task Force to review the curriculum as it related to these domains and propose methods for
reorganization and integration across the four years of medical student training. In December
2012, Dr. Cristina Gonzalez, chair of the Clinical Prevention & Population Health Task Force,
listed each of the four domains being addressed – Clinical Prevention, Quantitative Skills,
Community Dimensions of Medical Practice, and Wellness and Interactive Medicine – and detailed
the steps the task force had taken to query course leaders about whether they are teaching material
in these four domains, survey students about what they believe they are learning in the domains,
identify deficiencies or redundancies, conduct searches for these topics in the curriculum in eMED
when possible, and propose changes to existing courses and clerkships. Dr. Gonzalez also proposed
that an “independent” CPPH faculty member sit in on both the Course Directors and Clinical
Directors Sub-committee meetings, and that the current community electives be integrated into the
required curriculum.
The Executive Committee then discussed how implementation and oversight of curricular themes,
such as those proposed by CPPH would be handled in the MEC structure. To that end, the
Executive Committee voted to have the CPPH become a member (to be joined by others) of a new
Curricular Themes Sub-committee of the MEC. This new sub-committee would report to the
Executive Committee, but would act as liaison with the Course Directors Subcommittee and the
Clinical Directors Subcommittee, which are responsible for integrating themes into their respective
curricula. Since then, the sub-committee has begun working on curriculum mapping of the CPPH
domains and has formed a working group to address two of the domains: Health Systems and
Health Policy, and Population Health and Community Aspects of Practice. This work is ongoing.
d. Illustrate how the curriculum committee would know where in the curriculum “health disparities” and
“genetic counseling” are covered. For example, if there is a curriculum database, provide electronic
copies of printouts of the results of searches for these two topics in the Appendix. If a curriculum
database is not used, illustrate the information on that is available and describe the sources of the
information that can be used to identify the presence of these topics in the curriculum.
In the eMED database, the key word(s) or phrase can be entered as a search term with the option of
selecting the appropriate related phrases in the UMLS dictionary. The results are then displayed
sequentially. For each result the type of document (file, document, URL, HTML, slide, etc.), title of
document (or slide), date created, date modified, and the course where the result is located will be
displayed. The result is hyperlinked to the actual content so that one-click access is available.
eMED has been undergoing significant changes and upgrades, including in the area of content
search. As these improvements are made, they become available to the Einstein educational
community.
The searches for “health disparities” and “genetic counseling” were performed. There were 85
results for health care disparities and 108 results for genetic counseling. These results appear as ED
Appendix W.
Also see information for standard ED-33.
ED-146
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-38. The committee responsible for the curriculum at a medical education program,
along with program’s administration and leadership, must develop and implement policies
regarding the amount of time medical students spend in required activities, including the
total number of hours medical students are required to spend in clinical and educational
activities during clinical clerkship rotations.
Attention should be paid to the time commitment required of medical students, especially during the clinical years.
Medical students' hours should be set after taking into account the effects of fatigue and sleep deprivation on
learning, clinical activities, and health and safety.
_____________________________________________________________________________________
a. Describe the means by which the curriculum committee or the relevant subcommittee(s), as well as
course and clerkship rotation leaders, monitor the academic and clinical workload of medical students
within and across individual courses and clerkship rotations.
The responsibility for monitoring the academic and clinical workload falls on several groups and
individuals.
The schedule of educational events for first and second year students is the framework for
monitoring the workload in the pre-clerkship years. The schedule is prepared by the senior
associate dean for medical education and the director of the Office of Instructional Support Service
and vetted by the directors of the pre-clerkship courses. The current policy is one of “zero net
change” in scheduled course hours. Any increase in time of classes or exams must be balanced by a
decrease in scheduled time of equal or greater magnitude. Requests for changes in scheduled time
are made by the course director to the senior associate dean and the director for approval.
Approved changes are reflected in the schedule, through actions of the staff in the Office of
Instructional Support Service.
In the clinical years, the Clinical Directors Sub-committee of the Medical Education Council sets
policy on work hours covering all clinical and didactic activities. The clerkship directors and site
leaders are responsible for enforcing the work-hour policies. In addition, clinical workload may be
addressed at the monthly clerkship directors meeting, based on any concerns raised with the Office
of Student Affairs.
Ultimate responsibility for monitoring students’ academic and clinical workload rests with the
senior associate dean for medical education.
b. Describe any formal policies limiting the amount of scheduled time for medical students in a given
week during the preclinical phase of the curriculum. Include electronic copies of relevant policies in the
Appendix.
While there is no written policy regarding maximum weekly class hours for the preclinical years,
the total hours have been previously set and cannot be exceeded. They remain the same from year
to year. The maximum number of weekly class hours for the first-year class is 26.75 and for the
second-year class is 30 hours. The typical weekly hours are between 19-24 hours with some weeks
having a lower number and some having a higher number of hours.
c. Summarize any medical school policies on medical student duty hours, including on-call
requirements for clinical rotations. Describe the means by which these policies are disseminated to
faculty, residents, and students.
ED-147
Albert Einstein College of Medicine
Academic Year 2014-2015
For the clinical rotations, there are several components to the duty hour policy. Students across
sites within a clerkship must have comparable work hours, although total work hours and
distribution of work hours across clerkships may vary. All clerkships are limited to a maximum of
80 total work hours per week (which includes clinical and educational activities). Sub-interns work
hours mimic intern work hours and may not exceed the ACGME policy and NYS 405 regulations.
The work hours policy for the clinical years is posted in several locations on eMED, including in
sections for students, faculty, and site leaders. The site leaders are responsible for disseminating
the policy and the actual work schedule (including on-call) to faculty, residents, and students at
their respective sites.
d. Describe the mechanisms by which the implementation and effectiveness of duty hours policies is
monitored. Describe the steps taken if duty hours limits are exceeded.
In the preclinical years, the Office of Instructional Support Service tabulates the total time
scheduled for each first- and second-year course and compares it with prior years where the total
times were approved. Any increase in scheduled time is reported to the course director and to the
senior associate dean for medical education for readjustment of duty hours to the prescribed
number for that course.
Implementation and effectiveness of duty hours policies within clinical rotations are monitored by
clerkship directors through their site leaders. (See ED Appendix X.)
e. Describe the mechanisms that exist for reporting violations of duty hours policies. How and to whom
can students report violations?
Students have several options for reporting violations of duty hour policies. Students can report via
an “anonymous drop box,” online, which is directed to the Office of Student Affairs. Anonymous
evaluations of courses and evaluations of clerkships include opportunities for general comments or
criticisms of the educational experience, which can include reports of duty hour violations.
There are several direct mechanisms for student reporting of duty hours violations. The Medical
Student Council is a clearinghouse for student issues, which are presented in several venues.
Violations of duty hours, discussed at Council meetings, could be presented by the student members
who sit on the Clinical Directors Sub-committee, the Course Directors Sub-committee or the
Executive Committee of the MEC. Other venues are the scheduled meetings of the senior associate
dean for medical education with members of the Council or the regular town hall meetings held by
the senior associate dean with classes at large. Students also have the opportunity to report duty
hours violation through the anonymous end-of-course or clerkship evaluations. In addition,
students may report work hours violations at any time directly to their course or clerkship director,
or to the Office of Student Affairs.
ED-148
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-46. A medical education program must collect and use a variety of outcome data,
including national norms of accomplishment, to demonstrate the extent to which its
educational objectives are being met.
The medical education program should collect outcome data on medical student performance, both during program
enrollment and after program completion, appropriate to document the achievement of the program’s educational
objectives. The kinds of outcome data that could serve this purpose include performance on national licensure
examinations, performance in courses and clerkship rotations and other internal measures related to educational
program objectives, academic progress and program completion rates, acceptance into residency programs, and
assessments by graduates and residency directors of graduates' preparation in areas related to medical education
program objectives, including the professional behavior of its graduates.
_________________________________________________________________________________
a. Check all indicators used by the medical school to evaluate educational program effectiveness:
X
X
X
X
X
X
X
X
X
Results of USMLE/MCC or other national examinations
Student scores on internally developed examinations
Performance-based assessment of clinical skills (e.g., OSCEs)
Student responses on AAMC GQ or the AAMC CGQ
Student evaluation of courses and clerkship rotations
Student advancement and graduation rates
NRMP match results or CARMS match results for Canadian medical
schools
Specialty choices of graduates
Assessment of residency performance of graduates
Licensure rates of graduates
Practice types of graduates
Practice location of graduates
Other (specify)
For each checked item, indicate
i.
The means by which the data are collected (including response rates for questionnaires).
ii. The groups or individuals that review the data (e.g., curriculum committee, department chairs)
and the frequency with which the reviews occur.
Results of USMLE examinations:
These data are regularly obtained from the NBME website by the Office of Student Affairs and
distributed to the deans in the Office of Medical Education. The data are kept on file by the
assistant dean for educational information resources, who prepares reports and graphs indicating
trends in pass rates and mean scores. These data are distributed and discussed at the Executive
Committee of the Medical Education Council, as well as to the relevant MEC subcommittees. For
example, the graph showing student performance in the various subject areas on the Step 1
examination is discussed at the Course Directors Sub-committee, which can recommend
strengthening the curriculum in particular areas of weakness. Similarly, the Clinical Directors
Sub-committee reviews student performance on the Step 2 CK and CS examinations. Individual
clerkship directors, as well as the deans mentioned above, receive the annual reports provided by
the NBME of student performance in subject area exams administered at the end of each clerkship.
ED-149
Albert Einstein College of Medicine
Academic Year 2014-2015
These reports allow them to determine whether the content in their respective clerkships matches
what is tested on the subject exams. In addition, the above-named reports become part of the
comprehensive Phase 2 review of all courses and clerkships conducted by the MEC Evaluation Subcommittee and reported to the Executive Committee.
Student scores on internally developed examinations:
All courses in the first two years use internally developed exams. Scores on these exams are
generated in the Office of Instructional Support Services and made available to the respective
course directors, the Office of Student Affairs and the Director of the Office of Academic Support
and Counseling. Scores are posted for students, who are able to access them once they have
completed the course evaluation.
As the examinations are sequestered, students who pass do not see copies of their exams. Only
those students who fail or are deemed “borderline pass” are invited to review their exams
individually with the professional staff of the Office of Academic Support and Counseling.
By tagging questions and associating them with school-wide competencies in the ExamSoft
software, the deans of education are able to measure the degree to which the competencies are
achieved. In addition, using computer-based exams course leaders with the ability to determine how
well the exam questions tested the material taught in the course and to make the needed
adjustments.
Performance-based assessment of clinical skills:
A Clinical Skills Assessment (CSA), independent of any course or clerkship, is scheduled in the
spring (March-May) of the third year. The CSA is overseen by the Clinical Skills Assessment Task
Force of the Medical Education Council, which meets monthly and is chaired by the director of the
Ruth L. Gottesman Clinical Skills Center. The CSA is an 8-station OSCE with each station
including an encounter with a standardized patient (15 minutes) followed by a post-encounter
written exercise (10 minutes). The format is much the same as the USMLE Step 2 CS (See ED-27b
for full description of the CSA). The students are evaluated by the standardized patients (SPs) who
complete history, physical exam and communication skills checklists. The passing standard is noncompensatory and normative. In order to pass, students must achieve a score above 2 SD below the
mean in overall score and all three components (history, physical exam and communication skills).
The purpose of the assessment is both summative and formative. Students who pass the CSA will
meet in groups of four with a faculty reviewer. If the students fail, they must complete a selfassessment assignment and meet with a faculty reviewer to review their videos, notes and scores.
The faculty member will help the student identify strengths and weaknesses and develop a plan for
improvement. During the summer there is a 4-station retest that the student must take. If a student
fails the retest, there will be a review of his/her academic record.
Data on student pass rates for this exercise are presented to the Executive Committee and the
Clinical Directors Subcommittee of the MEC in aggregate form only. Clerkship directors on the
committee use the performance data on individual cases to identify areas of weakness in students’
clinical skills and are then able to enhance or add the teaching of those skills in the appropriate
clerkship. The Office of Student Affairs is notified of any student failures on this exam.
The following are examples of OSCEs used to evaluate students’ clinical performance in the clinical
clerkships (See also ED-28):
ED-150
Albert Einstein College of Medicine
Academic Year 2014-2015
Internal Medicine Clerkship – GOSCE: assesses communication skills using a 4-station group
OSCE: 1) Tobacco dependence 2) Difficult doctor/patient encounter 3) Shared decision making
4) Delivering bad news.
Pediatrics Clerkship OSCE-Adolescent case: assesses communication, professionalism, historytaking, counseling and note-writing skills in an outpatient encounter with an adolescent,
through an OSCE using standardized patients.
Radiology Clerkship – Reading of radiologic studies on either iPads or through simulation with
monitors and dictation equipment to assess problem solving and communication skills.
Internal Medicine Sub-internship – OSCE: assesses advanced communication skills through
two cases on 1) Refusal of care and 2) Delivering bad news.
Geriatrics Clerkship - Goals of Care Discussion Mini-CEX: Students are observed having a
discussion with a patient or surrogate decision maker about advanced care planning.
Obstetrics/Gynecology Clerkship- Two-part summative OSCE: 1) Breast and pelvic exams on
silicone models 2) Oral exam: students are given two case scenarios (1 Ob, 1 Gyn) and ask
questions to get the history, results of a physical, labs and imaging, then make an assessment
and plan.
For all of the above except the summative Ob/Gyn OSCE, formative feedback is generally provided
to the students by the standardized patients and/or supervising faculty at the time of the exercise.
Feedback may include review of checklists or direct verbal feedback. Site leaders and clerkship
directors also will review collective data to identify students’ areas of relative weakness that need to
be addressed more thoroughly in the clerkship.
Student responses on AAMC GQ:
Each year, responses to this questionnaire are solicited using email messages to graduating medical
students, in addition to the periodic reminders sent electronically by the GQ staff at the AAMC.
Our response rates have increased markedly over the past few years, from 73% in 2011 to 82% in
2012, and 89.5% in 2013; the response rate for the Class of 2014 was slightly lower, 74.9%, perhaps
the result of the competing student survey for the self-study.
Results of the GQ are reported by the assistant dean for educational information resources to the
dean, the senior associate dean for medical education, the senior associate dean for students and are
discussed in detail at the Executive Committee of the MEC. The data report and a complete set of
comments are distributed to all Executive Committee members, and a PowerPoint presentation of
the salient findings is presented to this committee; discussion of the findings has resulted in
increased attention to the areas within the curriculum and the academic environment that need
attention.
In addition, the data report is distributed to all course directors and clerkship directors, and the
GQ results become part of the information that is reviewed for the Phase 2 of course and clerkship
reviews initiated by the Evaluation Sub-committee and reported to the Executive Committee.
Student evaluation of courses and clerkship rotations:
ED-151
Albert Einstein College of Medicine
Academic Year 2014-2015
Evaluation instruments for courses are posted electronically by the Office of Educational Resources
for student response at the time of the final examination or predetermined major examination in
each course. Students are required to complete the evaluations as part of their course obligations
within two weeks after the end of the course. Once course obligations are completed, their exam
scores and/or course grades are released to the student; student response rate is almost always
100% for every course.
Evaluations for clerkships are posted for student response on the final day of the clerkship, which
usually coincides with the scheduling of the shelf exam. Students are required to complete the
evaluations as part of their clerkship obligations. Once clerkship obligations are completed, their
shelf exam score and/or clerkship grade are released to the student; student response rate is at or
near 100% for every clerkship.
Upon the close of evaluations, the Office of Educational Resources provides the raw data
(frequencies and means of numerical items, and a complete listing of student comments) to each
course/clerkship director for review. The raw data, some basic analyses, copies of the Evaluation
Sub-committee reports for that course or clerkship of the past three years, the course/clerkship
objectives, the mapping of course/clerkship objectives to the Einstein Educational Competencies,
and any additional data required for the review are provided to the members of the Evaluation
Subcommittee. The sub-committee reviews the course/clerkship and generates a report that is
provided to the course/clerkship director and to the Course or Clerkship Directors’ Sub-committee,
as appropriate. The course/clerkship director responds to the report in his/her respective
subcommittee and documents any proposed changes in the curriculum for review.
In the Phase 2 review of courses and clerkships (described in detail in ED 35-a), the review
committee analyzes the data and delivers a report to the Executive Committee of the MEC focused
on the trends in student performance in the course/clerkship, the comparison with national norms,
identified strengths and weaknesses, identified gaps and redundancies, and student outcomes for
the Einstein competencies in that course. The Executive Committee of the MEC will discuss and
review the report and take appropriate actions as necessary.
Student advancement and graduation rates:
Data on student advancement and graduation rates are maintained in the Office of Student Affairs.
Specifically, the Registrar (part of the Office of Student Affairs) keeps records of the numbers of
students in each class who have been given customized schedules, taken leaves of absence, taken
time for research or independent study, or withdrawn. Additionally, members of each entering
class who are in the MD/PhD program are removed from the class roster for the period of their
laboratory research, and are returned to the medical student roster when they complete the PhD
phase of their education.
The data on student advancement and graduation rates are reviewed by the deans in the Office of
Student Affairs and by the Committee on Student Promotions and Professional Standards. These
data are useful in monitoring a number of factors, including the preparedness of our students to
undertake the medical school curriculum, and the degree of interest in pursuing research,
independent study, and global health fellowships among our students.
NRMP match results:
ED-152
Albert Einstein College of Medicine
Academic Year 2014-2015
Over the years, Einstein students have matched very successfully; the years 2013 and 2014 were no
exception. The 2014 Match List Summary (ED Appendix Y) shows the number of graduates
matching in various specialty areas from 2006-2014.
Information on the match results is prepared by the Office of Student Affairs and distributed to the
dean, the relevant deans, and is discussed at length at the MEC Executive Committee and the
Clinical Directors Sub-committee and the meeting of Department Chairs. Results are posted on
student bulletin boards, and a summary of results (without student names) is posted on the Einstein
website. Circulating the match results widely helps to reinforce the message that a rigorous clinical
education of the kind provided to students at Einstein prepares them well for residency training
and has a significant positive impact on their careers.
Specialty choices of graduates:
In 2014, for example, 44 students (25% of matched students) matched to residency programs in
Medicine; 26 students (15%) chose Pediatrics. Taken together with the 5 students matching in
Family Medicine, these add up to 43% the graduating class entering primary care fields. The next
most popular specialties were Emergency Medicine (12 students; 7%) and Psychiatry (12 students;
7%).
As mentioned above, the specialties to which our senior students have matched are distributed by
the Office of Student Affairs and discussed in detail by the deans and members of the Executive
Committee and Clinical Directors Sub-committee of the MEC.
Assessment of residency performance of graduates:
Since 2008, the Office of Educational Resources has surveyed program directors about the
performance of Einstein graduates completing their PGY-1 year using a survey instrument
designed with the help of the Executive Committee of the MEC. The competency-based survey
asked program directors to assess Einstein graduates in the following domains:
Patient care
Medical knowledge
Practice-based learning and improvement
Interpersonal and communication skills
Professionalism
Systems-based practice
Additional questions ask about the accuracy of the MSPE, the performance of the graduate relative
to other residents at the same level of training, and about the overall preparation of the graduate
for residency. Response rates to this survey have varied between 55-60% of program directors who
have evaluated on average 55-65% of our recent graduates each year.
Results of the survey (containing student names and comments about their performance) are made
available to the deans in the Office of Student Affairs. De-identified data in the form of graphs of
results, as well as comments with student names removed, are presented to the dean, the senior
associate dean for medical education and the Executive Committee of the MEC, as well as to the
Clinical Directors Sub-committee.
ED-153
Albert Einstein College of Medicine
Academic Year 2014-2015
b. Describe the means by which the results of the reviews are used for curriculum evaluation and
revision.
As described in detail in ED-35 a, Phase 2 of the curriculum evaluation incorporates a number of
these outcome measures in its periodic review of all courses and clerkships at Einstein. Specifically,
Phase 2 review committees examine course and clerkship evaluation data, USMLE performance
data, data related to the course/clerkship from the AAMC Graduation Questionnaire and the
Program Directors Surveys, student performance on standardized patient assessments, clinical
shelf examination results, and any other pertinent information. The Phase 2 reports are reviewed
and discussed by the Executive Committee of the MEC as part of its regular review of the
curriculum. Other outcome measures (e.g., NRMP match results, specialty choice, and graduation
rates) are discussed regularly by Executive Committee and other MEC committees.
c. Provide evidence that educational program objectives in the domains of knowledge, skills, behaviors,
and attitudes are being achieved.
Knowledge:
Students have demonstrated the achievement of knowledge by their strong performance in the
USMLE Step 1 examination (97% pass rate for first-time takers in 2013) and the Step 2 CK
examination (99% pass rate in 2013-2014 – interim data); 98% of our students passed the Step 2CS exam in 2013-2014. Student performance on knowledge-based pathophysiology exams in years 1
and 2 has always been strong. In 2013-2014, performance of Einstein students on the NBME
subject exams in the clinical clerkships exceeded national comparison means for all clerkships.
Skills:
Einstein students have performed well on a number of skills-based outcome measures. These
include:
In 2013-2014, 91% of first-year students passed the videotaped graded interview
competence exercise at the conclusion of the ICM-Introduction to the Patient course. In this
exercise, students are graded by a standardized patient on their communication and
history-taking skills.
In 2013-2014, 93% of second-year students passed the videotaped exercise in the ICM
Clinical Examination course; the exercise is graded by standardized patients examined by
the students.
In 2013-2014, the great majority of the third-year class passed each component of the
Clinical Skills Examination (CSA): History Taking (97% passed); Physical Examination
(97% passed); Communication Skills (96% passed).
99% pass rate on Step 2 CS examination in 2012-2013.
Behaviors/Attitudes:
Einstein students have performed well in the Communications domain of the year 3 Clinical
Skills Assessment (96% pass rate in 2013-2014), as evaluated by the standardized patients.
On the AAMC Graduation Questionnaire, students routinely praise Einstein for allowing
them the opportunity to treat many indigent patients served by the hospitals in our Bronx
community. Similarly, most students engage in volunteer activities at local homeless
shelters, food banks, and wellness programs for the benefit of the local community.
ED-154
Albert Einstein College of Medicine
Academic Year 2014-2015
Einstein has one of the largest Global Health programs of any medical school in the U.S.
Over the past decade, approximately 50% of our students have taken advantage of the
opportunity to spend a month or more in at least a dozen less developed/emerging nations in
Africa, Asia, Central and South America to experience caring for its people. These
programs expose students to health care needs in the developing world and sensitize them to
the needs of indigent populations here. A number of our graduates have gone on to include
global health as a major focus of their medical careers.
Einstein students formed a student-run free clinic, the Einstein Health Care Outreach
(ECHO Clinic) to respond to the needs of uninsured patients living in the Bronx. A large
majority of our students volunteer their time at this facility and deliver care under the
supervision of volunteer faculty.
Einstein students originated and continue to run the Social Medicine lecture series,
addressing many of the thorniest public health issues, such as access to care, response to
gun violence and domestic abuse, health care reform health care disparities, LGBT and
women’s healthcare issues, etc.
The results of the annual Program Directors Survey, originated in 2008, show that Einstein
students are consistently rated highly for their performance in the following domains
related to professionalism evaluated in the survey (See graph below in ED-46 d):
o
o
o
o
Putting patients’ needs above self-interest
Commitment to ethical principles
Sensitivity to cultural differences
Advocacy for patients
d. If available, provide summary data on the performance of the medical school’s graduates in the
following areas:
i.
USMLE Step 3 or MCCQE Part II
Year or Academic Year
Number
Examined
Percent
Passing on
First
Attempt
Number
Repeating
Exam
Repeat
Performance
2008 Graduates
2009 Graduates
2010 Graduates
2011 Graduates
168
175
156
168
99%
99%
96%
97%
No data
No data
6
2
No data
No data
67%
No data
ii. Graduate medical education (e.g., from surveys of graduates or residency program directors)
Since 2008 the OER has administered an annual web-based Program Directors Survey evaluating
the progress of Einstein graduates completing their internship year (See ED-46c above.). This
survey provides valuable data on the performance of our graduates and the strength of our medical
education program. Figure 1 summarizes the performance of Einstein graduates who are PGY-1s
in the specific competencies evaluated by their respective program directors over the past three
ED-155
Albert Einstein College of Medicine
Academic Year 2014-2015
years (See ED Appendix Y contains results of the recently completed Program Directors Survey for
the Class of 2013).
Scale: 5=Outstanding; 1=Inadequate
Figure 1: Evaluation of Overall Competency of Einstein Graduates, Classes of 2010-2012:
Results of the Program Directors Survey
4.6
Class of
2010
(n=88)
4.5
4.4
4.3
Class of
2011
(n=110
)
Class of
2012
(n=88)
4.2
4.1
4
3.9
3.8
Figure 2 depicts the program directors’ assessment of Einstein graduates’ clinical preparedness
compared with other residents at the same level of training:
ED-156
Albert Einstein College of Medicine
Academic Year 2014-2015
Figure 2: Performance of 2010, 2011, and 2012 Gradutes in Relation to Residents at
the Same Level of Training: Results of the Program Directors Survey
60.0%
55.7%
50.0%
49.4%
47.7%
40.2%
40.0%
41.4%
30.7%
Performanc
e Stronger
30.0%
20.0%
Performanc
e Weaker
Performanc
e About the
Same
13.6%
12.1%
10.0%
9.20%
0.0%
Class of 2010 (n=88)
Class of 2011 (n=110)
Class of 2012 (n=88)
Figure 3 summarizes the program directors’ view of the overall preparedness of Einstein graduates
to undertake the responsibilities of residency training:
Scale: 5-Outstanding; 1-Inadequate
Figure 3: Overall Preparedness of Einstein Graduates for Residency Training,
Classes of 2010-2012: Results of the Program Directors Survey
4.2
4.17
4.13
4.15
4.1
4.03
4.05
4
3.95
Class of 2010 (n=88)
Class of 2011 (n=110)
Class of 2012 (n=88)
ED-157
Albert Einstein College of Medicine
Academic Year 2014-2015
FOR U.S. MEDICAL SCHOOLS ONLY:
e. Indicate if students at the medical school are required to take or required to pass USMLE Step 1, Step
2 CK, and Step 2 CS. (check)
Step 1
Step 2 CK
Step 2 CS
Take
X
X
X
Pass
X
X
X
f. In the Appendix, include electronic copies of print outs and graphs provided by the National Board of
Medical Examiners that compare the performance of national and medical school first-time takers for
USMLE Steps 1 and 2 for the past three academic years.
See ED Appendix Z.
g. For each of the past three academic years, provide results for REPEAT (not first-time) takers of
USMLE Steps 1 and 2.
STEP 1
Year
Number Examined
Percent Passing
2011
2012
2013
4
5
3
100%
100%
100%
Mean Total Score
and S.D.
Score
211
204
198
S.D.
11
6
10
National Mean
Total Score
and S.D.
Score
S.D.
198
15
196
15
197
13
STEP 2 CK
Year
2011-2012
2012-2013
2013-2014*
*Interim Report
Number Examined
Percent Passing
2
1
0
50%
100%
-
Year
Number Examined
Percent Passing
2010-2011
2011-2012
2012-2013
0
2
1
100%
100%
Mean Total Score
and S.D.
Score
S.D.
Score
S.D.
196
No data
-
13
No data
-
203
209
213
14
12
13
STEP 2 CS
ED-158
National Mean
Total Score
and S.D.
National Percent
Passing
No data
No data
No data
Albert Einstein College of Medicine
Academic Year 2014-2015
FOR CANADIAN MEDICAL SCHOOLS ONLY:
h. In the Appendix, include an electronic copy of the summary table (Dean’s Report: Section II) of
student performance on the MCCQE Part I for each of the past three academic years; include the
percentage of students passing.
Also see Part A, item (b.) in this section, information for standard ED-47, and Required Course and
Clerkship Rotation Forms.
ED-159
Albert Einstein College of Medicine
Academic Year 2014-2015
ED-47. In assessing program quality, a medical education program must consider medical
student evaluations of their courses, clerkship rotations, and teachers, as well as a variety
of other measures.
It is expected that the medical education program will have a formal process to collect and use information from
medical students on the quality of courses and clerkship rotations. The process could include such measures as
questionnaires (written or online), other structured data collection tools, focus groups, peer review, and external
evaluation.
____________________________________________________________________________________
a. Summarize the means by which information is collected from students on course and clerkship
rotation quality. Describe the methods that are used (e.g., questionnaires, focus groups) and average
response rates. In the Appendix, include an electronic copy of any standardized forms used by students
for the evaluation of courses and/or clerkship rotations.
The Office of Educational Resources (OER) is the unit within the Office of Medical Education
responsible for developing and managing the evaluation of the medical school curriculum and its
teachers. The OER's electronic evaluation systems allow students to complete their course and
clerkship evaluations more thoughtfully and away from the stress of the exam room and provides a
timely and comprehensive picture of student opinions about the curriculum. All evaluation
instruments contain a combination of fixed-response and open-ended questions.
Einstein considers it part of each student’s professional responsibility to provide constructive
feedback on the curriculum. All end-of-course or end-of-clerkship evaluations are considered an
essential component of the course or clerkship, and completion of these evaluations is therefore
mandatory for all students. Response rates nearly always reach 100% for all courses and
clerkships.
Student feedback generated by these evaluations is shared routinely with course and clerkship
directors, education deans, the Evaluation Sub-committee, the Course and Clerkship Directors
Sub-committees, and the Executive Committee of the MEC, and with individual faculty members,
as appropriate, in the belief that meaningful improvement in the curriculum and teaching will
result (See ED-35).
All data are gathered and reported as aggregate data. To safeguard student confidentiality, the
OER’s policy has always been to release all course and clerkship evaluation data after grades have
been released. This assures that the grading of students and the evaluation of the curriculum are
completely separate processes.
Pre-Clerkship Course Evaluations:
In consultation with members of the Evaluation Sub-committee and with the Course Directors
Subcommittee of the MEC, the OER prepares evaluations using eMED, our learning management
system, for all first- and second-year courses. The evaluation uses a standard format across courses,
with slight variations depending on specific course components. (See ED Appendix U.)
On the day of the course examination, the evaluation is uploaded in eMED, and students receive an
email message indicating that the evaluation is posted. Students will have one week plus an
additional one-week grace period in which to complete the evaluation. Grades are released to each
student one business day after the evaluation has been completed.
ED-160
Albert Einstein College of Medicine
Academic Year 2014-2015
Clerkship Evaluations:
The OER uses a standard web-based evaluation form for all third-year clerkships, and separate
web-based forms for sub-internships, ambulatory rotations, and short clerkships. Separate forms
also allow students to easily evaluate the clinical teaching of their attendings and residents. These
evaluations are made available electronically to the students on the day of the shelf exam. Any
student who has not completed a clerkship evaluation within six weeks after the shelf exam will
receive a grade of Incomplete. (See ED Appendix U.)
The OER reports clerkship evaluation results in the form of semi-annual summaries sent to the
respective department chairs, clerkship directors, and education deans, and to the Evaluation Subcommittee. These summaries are released only after all grades for the respective clerkship have
been submitted to the Registrar. The students’ evaluations of individual residents are sent to their
residency program directors and to the respective clerkship directors and site leaders in May of
each year. In August or September, annual clinical teaching summaries for all faculty teaching in
the required clerkships are sent to the respective clerkship directors for distribution to faculty, with
summary tables sent to the respective department chair. Faculty wishing to obtain cumulative
teaching data from the electronic systems maintained by the OER staff may contact the OER at any
time throughout the year.
Focus Groups:
The OER professional staff are experienced in conducting focus groups for a variety of users: basic
science course directors, student groups, and faculty conducting educational research
projects. Their services also include the analysis and reporting of focus group data.
Describe any other individuals or groups providing feedback about course and clerkship rotation quality
(e.g., through peer assessment of teaching or course content).
Although the Office of Educational Resources is the main source of evaluation data on courses and
clerkships at Einstein, at least one clerkship, e.g., the Family Medicine clerkship, conducts
evaluations of specific components of their curriculum (e.g., team-based learning sessions and the
community project) that are not evaluated in the end-of clerkship evaluation. The data provided
help the clerkship directors to evaluate and enhance particular aspects of their curriculum.
b. Describe who reviews student and other feedback on courses and clerkships and how the data are
used to improve the medical education program.
Following the completion of a course or clerkship evaluation, the Office of Educational Resources
provides the raw data (frequencies and means of numerical items, and a complete listing of student
comments) to each course/clerkship director for review. The raw data, some basic analyses, copies
of the Evaluation Sub-committee reports for that course or clerkship of the past three years, the
mapping of course/clerkship objectives to the Einstein Competencies, and any additional data
required for the review are provided to the members of the Evaluation Sub-committee. One faculty
member of the sub-committee is selected as the primary reviewer. The Sub-committee will review
the course/clerkship and generate a report that is provided to the course/clerkship director and to
the Course or Clerkship Directors Sub-committee, as appropriate. The course/clerkship director
responds to the report in his/her respective subcommittee and documents any proposed changes in
the curriculum for review.
ED-161
Albert Einstein College of Medicine
Academic Year 2014-2015
Phase 2 Reviews:
Annually, the Executive Committee of the MEC determines which courses and clerkships are to be
reviewed. The goal is to review every course and clerkship every three to four years. The assistant
dean for educational information resources, working with the chair of the Executive Committee of
the MEC, selects the members of the review committee.
The Office of Educational Resources provides the review committee with the raw data for the
course/clerkship since its last review, the Evaluation Sub-committee reports and course/clerkship
director’s responses, data related to the course/clerkship from USMLE Step 1, Step 2, Step 3, as
appropriate, data related to the course/clerkship from the AAMC Graduation Questionnaire and
the Program Directors Surveys, student performance on standardized patient assessments, clinical
shelf examination results, and any other pertinent information.
The review committee analyzes the data and delivers a report to the Executive Committee of the
MEC focused on the trends in student performance in the course/clerkship, the comparison with
national norms, identified strengths and weaknesses, identified gaps and overlaps, and student
outcomes for the Einstein competencies in that course or clerkship. The Executive Committee of the
MEC will discuss and review the report and take appropriate actions as necessary.
Examples of the Use of Evaluation Data to Improve the Medical Education Program:
Changes to the Patients, Doctors & Communities curriculum: Over the years, evaluation data
from students have shown that discussing the challenges they face during their third-year
clerkships was the most valuable aspect of this course and helped them to share experiences and
develop strategies to deal with those challenges. In response to repeated requests from students
in their evaluations of the PDC course, the amount of time devoted to “debriefing” of students’
experiences in the clerkships was expanded and made a formalized component of each group
session.
Changes to the examination schedule in the Nervous System & Human Behavior course: Citing
the large amount of material covered in each of two examinations in this second-year “megacourse,” students consistently requested on the end-of-course evaluation that a third exam be
added. This change was effected in 2010.
Addition of physical diagnosis sessions in first-year Introduction to Clinical Medicine course: In
their end-of-course evaluations of Introduction to the Patient, the first-year ICM course, large
numbers of students have asked for the opportunity to begin learning some basic physical
examination skills that they might be able to practice at their clinical sites in the ICM Clinical
Experience course. Beginning in the 2011-2012 academic year, two sessions emphasizing the
examination of the chest and the abdomen were added, replacing two more advanced
communication skills sessions that have been moved to the second-year ICM course. Student
response to the addition of these PE sessions has been very positive.
Inclusion of USMLE-style questions on pre-clerkship course examinations: Student evaluations
of both first- and second-year courses have asked repeatedly for the addition of these boardtype questions to assist them in preparing to take the USMLE Step 1 exam. These concerns also
were brought to the MEC Course Directors Sub-committee by its student members, resulting in
a workshop for all course directors taught by the director of the Microbiology and Infectious
Diseases course, who is also active in writing and reviewing questions at the NBME. This course
ED-162
Albert Einstein College of Medicine
Academic Year 2014-2015
director offered to review questions written by other course directors, resulting in the inclusion
of board-type questions in many first- and second-year courses.
At the request of the students, a lecture capture system (Panopto) was purchased and utilized
for the majority of lectures during the 2012-2013 academic year. Students appreciated having
the option to review the recording linked to the PowerPoints after the class, and made a request
to standardize this option for all lectures. Starting in December 2013, a policy was approved to
capture all lectures given during the first two years. The only exception granted will be if a
video of a patient is utilized in lecture and the patient has not signed a waiver authorizing the
use of the video for educational purposes.
c. Describe whether medical students provide evaluation data on individual faculty, residents, and others
who teach or supervise them in required courses and clerkship rotations. How are these data used to
improve the quality of teaching and/or supervision?
Evaluation of Faculty Instructors in Pre-clinical Courses:
All end-of-course evaluations allow students to assess the teaching skills of their faculty instructors,
an integral component of each course. Students are required to complete an evaluation of the
teaching skills of these instructors by the end of the course, and grades are not released until the
student has completed all the components of the evaluation. After evaluations are collected, a
course evaluation summary is sent to the course director containing reports of these teaching
evaluations, and individual reports with each faculty instructor’s score and the range of scores for
all instructors. Each course director is responsible for reviewing these evaluations and distributing
individual copies to all faculty teaching in the course. As part of its regular review of all courses, the
Evaluation Sub-committee also reviews the teaching performance of course faculty.
In January 2014, a new form focused on small-group instruction was developed, including an
assessment of the skills of small-group facilitators. Beginning in September 2014, a new form for
evaluating lecturers and a revised form for evaluating small-group facilitators will be opened at the
start of each course, enabling students to evaluate faculty while the course is ongoing.
Course directors may use these teaching evaluations to plan course-specific faculty development
programs for their faculty or to recommend that individual faculty attend one of the many sessions
offered by the Office of Faculty Development to improve teaching skills.
Evaluation of Clinical Faculty in the Clerkships:
Similarly, students in the clinical clerkships are required to complete all components of the
clerkship evaluation, including the evaluation of the teaching skills of their faculty instructors;
clerkship grades are not released until the student has completed clinical teaching evaluations.
Annual clinical teaching summaries are created by the Office of Educational Resources staff for all
faculty teaching medical students in the third-year and fourth-year clerkships and fourth-year
required sub-internships (Medicine, Pediatrics, and Family Medicine). These summaries are
generated yearly in August/September, and copies are sent to the respective clerkship directors,
with summary tables of overall teaching performance sent to department chairs and to the senior
associate dean for medical education. Tables of overall clinical teaching performance are also
reviewed by the Evaluation Subcommittee as part of their review of each clinical clerkship.
ED-163
Albert Einstein College of Medicine
Academic Year 2014-2015
After reviewing individual and aggregate teaching data, clerkship directors may elect to develop
clerkship-specific teaching modules to address faculty needs, or to encourage individual faculty
members to attend the workshop offerings of the Office of Faculty Development.
Other Uses of Teaching Evaluations:
In a larger sense, the data generated by teaching evaluations of faculty suggest to the Offices of
Medical Education and Faculty Development broad areas where our faculty may need development
or enhancement of their teaching skills in the form of workshops, attendance at conferences, etc.
The Faculty Development Task Force is the venue for discussions about developing programs and
workshops to enhance the teaching skills of our faculty.
Teaching scores generated from student evaluations by the Office of Educational Resources also
form the basis of recommendations for rewarding excellent faculty teaching, through the selection
of faculty for the receipt of education awards and/or for membership in the Leo M. Davidoff
Society, in recognition of their outstanding teaching of medical students. In addition, faculty being
proposed for academic promotion rely heavily on the cumulative clinical teaching data that can be
generated by the OER or individual faculty on demand.
Evaluation of Non-Faculty Instructors:
A non-faculty instructor at Einstein is usually a:
• Resident / Intern
• Graduate student
• MD-PhD student
• Postdoctoral research fellow without faculty appointment
• Postdoctoral clinical fellow without faculty appointments
• Physician without faculty appointment
• Peer medical student
• Nurse
• Midwife
• Nutritionist
• Community worker
• Social worker
• Medical technician
• Physician assistant
Evaluation of Non-Faculty Instructors in the Pre-clinical Courses:
In courses where these non-faculty instructors teach and supervise medical students, all students
are required to complete an evaluation of the teaching skills of these instructors by the end of the
course. Student grades are not released until the student has completed all the components of the
course evaluation including the resident/non-faculty instructor teaching evaluation. These
evaluations must be completed within two weeks after the end of the course. After evaluations are
collected, the course evaluation summary is sent to the course director containing reports of these
teaching evaluations, and individual reports with each instructor’s score and the range of scores for
all instructors. The course director is responsible for reviewing the evaluations and distributing
them to all non-faculty instructors who teach in his/her course.
Evaluation of Resident and Non-faculty Instructors in Clinical Rotations:
ED-164
Albert Einstein College of Medicine
Academic Year 2014-2015
In clerkships where these residents and non-faculty instructors teach and supervise medical
students, all students are required to complete all components of the clerkship evaluation, including
the evaluation of the teaching skills of these instructors. These evaluations must be completed
within two weeks after the rotation has finished. Student grades are not released until the student
has completed the resident/non-faculty instructor teaching evaluation. Cumulative reports are
generated for the residents and non-faculty instructors who teach Einstein medical students in the
third-year and fourth year clerkships and fourth-year required sub-internships (Medicine,
Pediatrics, and Family Medicine).
These semi-annual reports, with numerical evaluation data and comments, are produced twice each
academic year and are sent to the clerkship/sub-internship directors.
Annually, summary reports of these data are sent to:
The Evaluation Sub-committee, which reviews the non-faculty and resident teaching
evaluations for each course and clerkship/sub-internship.
All clerkship/sub-internship directors and clerkship site directors.
All residency program directors at all Einstein-affiliated institutions where our students
receive their clinical training.
The associate dean for graduate medical education receives a copy of the memo, data and
comments for house staff at all sites (downloaded on May 1st, as per instructions from the
Office of Graduate Medical Education).
The assistant deans at the affiliates also receive the data on resident teaching at their
respective sites.
Each residency program director is advised that he/she may request, from the Office of Educational
Resources, individual copies of the resident teaching evaluations to distribute to their residents for
feedback. Each residency program may use the results of the student evaluations to select
candidates for selection for various teaching awards, including the Leo M. Davidoff Society resident
teaching award.
Opportunities provided for remediation of inadequate performance of all non-faculty instructors:
The identification and remediation of a resident or non-faculty instructor with inadequate teaching
and/or assessment skills occurs via a summative process and/or a formative process.
Summative process:
Medical students appraise residents and non-faculty instructors on their teaching/assessment skills
after the end of each course and each clerkship rotation block using an evaluation form (e.g.,
“Student Evaluation of Resident / Non-faculty Instructor Teaching in Courses/Clerkships” forms)
via an on-line system. This evaluation form allows medical students to rate their residents/nonfaculty instructors’ specific teaching abilities (e.g., feedback skills, enthusiasm) and their overall
teaching performance on a 5-point scale (1=poor; 5=outstanding). Medical students are also
provided a section for narrative comments. The Office of Educational Resources generates a report
of this data at the end of each course and every six months for clerkships/sub-internships. This
report identifies any challenged resident/non-faculty instructors if an aggregate report denotes:
A cumulative score of ≤2.9 on any one or more items linked to specific teaching abilities
and/or on the overall performance and/or
ED-165
Albert Einstein College of Medicine
Academic Year 2014-2015
Narrative comments indicating a serious concern about teaching performance or
mistreatment of students.
The Office of Educational Resources notifies the course/clerkship director and assistant dean for
medical education that a challenged resident/non-faculty instructor has been identified by the
summative evaluation process. The Office of Educational Resources provides the course /clerkship
director with the “Resident/Non-faculty Instructor Teaching Improvement Plan” form contained in
the Teaching Star manual. (See ED Appendix N.)
In courses, the course director contacts the resident/non-faculty instructor directly to discuss the
summative evaluation of their teaching/assessment performance and mutually create a remediation
plan. In clerkships, the clerkship director contacts the supervisor (e.g., residency program director,
fellowship director, nursing or midwife director, etc.) of the challenged resident/non-faculty
instructor. The supervisor contacts the resident/non-faculty instructor directly to discuss the
summative evaluation of their performance and create a mutual remediation plan. In some
situations, the supervisor may be the clerkship director.
In the event that mistreatment is reported in either the course or clerkships:
Residents, fellows, nurses, other clinical staff and their supervisors will follow the local
departmental and hospital policies and procedures on mistreatment.
Graduate students, MD-PhD students, peer medical students and their course/clerkship
directors will follow the existing policies and procedures on mistreatment of the College of
Medicine.
The resources for remediation that are provided to all challenged resident/non-faculty instructor
include counseling, mentoring, review of institutional policies, readings, direct observation of
teaching with feedback, reflective exercises, online modules and teaching development sessions (e.g.,
lectures, workshops, and retreats) provided by departments, hospitals and the medical school (e.g.,
Fundamentals of Course Design and Teaching course).
The “Resident/Non-faculty Instructor Teaching Improvement Plan” form must be completed and
signed by the course director – and in clerkships, by both the clerkship director and the
appropriate supervisor – and returned to the Assistant Dean for Medical Education to document
compliance with this remediation policy.
Formative process:
A resident/non-faculty instructor may be identified as a challenged instructor during a
course/clerkship rotation by the course director, clerkship director or clerkship site director. This
may occur by:
Direct observation by faculty
Student report
Observation and report by others (e.g., peers or staff)
A resident/non-faculty instructor identified as a challenged instructor during a course/clerkship
rotation by the course/clerkship director will also follow the same process outlined above, but
documentation will not be required unless the summative process is activated.
ED-166
Albert Einstein College of Medicine
Academic Year 2014-2015
Also see information for ED-35.
END OF SECTION II
ED-167