An Introduction to Co-Occurring Disorders
advertisement

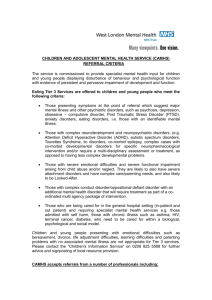
An Introduction to Co-Occurring Disorders Hon. Peggy Fulton Hora Judge of the Superior Court of California (Ret.) LADCP April 12, 2012 “Frequent flyers” in the justice system Questions 1.. Have you had a professional experience where you needed information about an AOD and mental health issues? 2. What is the percentage of persons whom you see who have co-occurring mental health and substance abuse disorders? 3. What is the biggest problem you have in a court setting handling this type of person? Mental Illness Defined Mental illnesses are medical conditions that disrupt a person's o thinking, feeling, mood, o ability to relate to others o and daily functioning. Just as diabetes is a disorder of the pancreas, mental illnesses are medical conditions that often result in a diminished capacity for coping with the ordinary demands of life. NAMI Addiction is a brain disease… …with biological, sociological and psychological components expressed as compulsive behavior. Why is this topic important to criminal justice? • Approximately 5-7% of the U.S. population has a serious mental illness • But 14.5 % of men and 31% of women in custody have a SMI • 33% of drug court participants have a co-occurring disorder • “Task Force for Criminal Justice Collaboration on Mental Health Issues,” AOC CA 2010 DSM 301.7 Antisocial Personality Disorder • Pervasive pattern of disregard for and violation of the rights of others • Begins in childhood or early adolescence and continues into adulthood • Deceit and manipulation are central features • Impulsivity and disregard of consequences • 3% males, 1% females general population • 20-25% for SA tx; 30% criminal offenders Psychopathy • Mental disorder marked by affective, interpersonal, and behavioral abnormalities • A demonstrated incapacity for empathy and guilt, impulsivity, egocentricity, and chronic violations of social, moral, and legal norms • 3.5% in SA Tx • 8% in criminal justice system Largest mental hospital in the U.S.? Los Angeles County Jail with 3,000 MI inmates every day Earley, Pete, Crazy: A Father's Search Through America's Mental Health Madness (Putnam, 2006) Recidivism rates higher • Recidivism rates for probationers with mental illness are nearly double (54% vs. 30%) • Those with MI are more likely to have their probation revoked than those without • Parolees have higher violation rates • Lorena L. Dauphonot, “The efficacy of community correctional supervision for offenders with severe mental illness 57 (9-B) Dissertation Abstracts International: Section B: The Sciences and Engineering 5912 (March 1997) Crime rates • Persons with mental conditions report being under the influence at the time of the offense in greater numbers than those who do not have such conditions Louisiana Numbers • 183,000 adults live with SMI and about 49,000 children live with serious mental health conditions • In 2008, approximately 9,100 adults with mental illnesses were incarcerated in prisons in Louisiana • Public mental health system provides services to only 17 percent of adults who live with • serious mental illnesses in the state NAMI State Advocacy 2010 Grading the State “D” “D” “D” “Grading the States 2009,” NAMI • Health Promotion and Measurement: D • Financing & Core Treatment/Recovery Services: D • Consumer & Family Empowerment: D • Community Integration and Social Inclusion: D Who do we see in court? • People with significant multiple drug problems • People with psychiatric disorders that can benefit from medication, including psychotic disorders • People whose accommodation and general life functioning is brittle • High risk, high need on Risk/Need Assessment instruments Lethality • According to U.S. Justice Department statistics, 15.8 percent of the defendants in cases of children killed by a parent had a history of untreated mental illness. • People with SMI commit 5,000 suicides and 5% of all homicides in the U.S. Shortage of hospital beds for MI • For every 20 public psychiatric beds in the US in 1955, there is only one today • “Untreated persons with severe mental illness have become major problems in homeless shelters, jails, public parks, public libraries and emergency rooms.” “TAC Study Reveals Severe Shortage of Psychiatric Beds,” Catalyst, Treatment Advocacy Center (Summer 08) If punishment won’t work, • …then what’s a judge to do? • ASSIGNMENT: Write down alternatives to “punishment” for people with cooccurring disorders Incarceration When you use jail as a sanction, what happens? Issues • Sanctions, Incentives and Treatment Responses • Incarceration • Victim input • Mental Health Court/docket • Courtroom Control • Others? What is a co-occurring disorder? • More than one diagnosable illness in the same individual • Types of co-occurring: medical, psychiatric, developmental, etc. What is a co-occurring substance abuse and mental health disorder? • Substance use, abuse, addiction • Plus one (or more) diagnosable mental health disorders, e.g., Bi-Polar Schizophrenia Depression PTSD 1. 2. 3. 4. “Co-occurring mental health disorders should be the expectation, not the exception.” Dr. Ken Mincoff Prevalence of Co-Occurring Epstein, Joan, et al., “ Serious Mental Illness and Its Co-Occurrence with Substance Use Disorders,” 2002. Office of Applied Sciences, SAMHSA Prevalence of Co-occurring Disorders • 4.2 million adults (18+ y.o.) have a serious mental illness (SMI) and a substance use disorder • Illicit drug use is more than twice as high among persons with a SMI than without (27% to 12.5%) • 2003 NSDUH data 4 million people with co-occurring • More than half (52%) receive neither MH or SA Tx • Of those receiving tx, 34% receive only MH • 2% for SA tx • 12% received tx for both “4 Million Have Co-Occurring Serious Mental Illness, Substance Abuse,” SAMHSA News (Sept./Oct. 2004) Co-Occurring Disorders by Severity Substance Abuse Low Severity Mental Illness High Severity High Severity Low to Moderate Psychiatric Disorders Low to Moderate Severity Substance Use Disorder High Severity Psychiatric Disorders Low to Moderate Severity Substance Use Disorder Low to Moderate Psychiatric Disorders High Severity Substance Use Disorder High Severity Psychiatric Disorders High Severity Substance Use Disorder Co-occurring disorders are expensive • In central TX in the last 6 years just 9 residents accounted for 2,678 visits. • One treated in Er > 100 times • Most have hx of substance abuse and mental illness • Cost = $2.7 million “What an Outrage,” AARP Bulletin (June 2009) Mental Health + Substance Use • Each can effect the onset of the other • E.g., patients with psychotic disorders who smoked marijuana at an early age developed symptoms almost three years sooner than those who did not Matthew Large, et al., “Cannabis Use and Earlier Onset of Psychosis A Systematic Metaanalysis” , Arch Gen Psychiatry. Published online (February 7, 2011) • Its severity • E.g., marijuana may contribute to the severity of schizophrenia’s symptoms (Smesny, et al, ”Cannabinoids influence lipid-arachidonic acid pathways in schizophrenia,” Neuropsychopharmacology 32:2067-2073, 2007) “Cannabis Could Increase Risks Of Psychotic Illness By 40 Percent,” Cardiff University (2007, August 1). Each can mask the other Which comes first? • Recent study showed alcohol abuse may lead to an increased risk of depression, not the opposite • May be genetic link • Fergusson et al., “Tests of Causal Links Between Alcohol Abuse or Dependence and Major Depression,” Archives of General Psychiatry 66 (3) (2009) Treat Both Disorders “Ample evidence in the literature supports the notion that inadequately treated psychiatric symptoms interfere with addiction treatment.” Co-Occurring Disorder Center Mentally ill offenders’ re-entry • Major program components that improve chance of MI offenders reentering society: 1. Coordinated pre-release planning up to 3 months prior to release 2. Intensive post-release case management Theurer, Gregory and David Lovell 47(4) Journal of Offender Rehabilitation (2008) 385-406 Re-entry, cont. • Residential support services • Community supervision • Co-occurring tx delivered by mental health staff with SA training Some Strategies to Consider • Use jail sparingly so medication regimes are not compromised • Look for creative alternative to incarceration like ordering the defendant to set up chairs for peer support group • Link volunteer work with something defendant likes to do (work outdoors, work with animals, etc.) Strategies, cont. • Make sure defendant receives integrated substance abuse and mental health treatment • Monitor cases closely – community corrections or the court for high risk/high need offenders To reduce recidivism • Ask, “Are they managing their illness”? 1. 2. 3. Going to tx and support groups Taking meds Accepting their illness • Find an “honest broker” to services. 1. 2. 3. Reporting deviations from the tx plan Providing gender and culturally competent tx Using evidence-based practices Dave Kelly, Deputy District Attorney, Brooklyn Mental Health Court WOMEN Mental health issues • Co-morbidity complicates and exacerbates the problems • Almost 12% of mothers in the U.S. has serious mental illness; 3.2% had SMI + SA • Up to 95% of parents in tx programs have co-occurring disorders Post Traumatic Stress Disorder 30-57% women in treatment meet criteria for PTSD 45-85% of battered women meet criteria Co-morbidity for PTSD and substance use disorders is 2-3xs higher for females Trauma-informed Care • Community corrections, prosecution, defense and the court must become “trauma-informed” • Substance abuse and other mental health issues are closely associated with trauma • SA/MH drives the justice system—both criminal and child abuse and neglect cases “Understanding women in court,” SAMHSA, Center on Women, Violence and Trauma (2006) Women with Co-Occurring Primary Drugs of Choice 50% 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% OAS, 2002 Alcohol Opiates Cocaine Marijuana Stimulant Other Cocaine / Alcohol Abusers with Comorbid Psychiatric Disorder MEN Anxiety Depression Bipolar Panic disorder Social phobia PTSD 48% 36% 6% 10% 14% 24% WOMEN 70% 40% 4% 18% 10% 46% Men vs. Women in Custody • Women inmates have >symptomology • diagnosed with mental health problems 3xs rate of men Symptoms Diagnosed SP M SP F Jail M Jail F 48% 8% 62% 23% 59% 9% 70% 23% Women with Co-Occurring More Likely Than Men to be: • • • • • • • Poor Uneducated Poor job skills Receive public assistance Report more relatives with AOD problems Care for more dependents Depressed, anxious, have eating disorders and lower self-esteem “Women with Co-Occurring Mental Illness and Substance Abuse,” AIA Center (May 2005) Jennifer • Repeated phone calls to ex • AOD issues? • MH issues? • How do you get the information you need? CHILDREN AND ADOLESCENTS Teens with co-occurring disorders Addressing Teens’ Issues • Consider arrest histories of adolescent and young adult clients • Coordinate services between MH, juvenile and criminal justice • Provide those at high risk with best services targeted at reducing antisocial behavior • Provide for continuity of services during ages 16-25 Davis, Maryann, PhD, et al., “Adolescent Mental Health Gender Differences in Arrest Onset & Risk,’ Center for Mental Health Services Research, U Mass Med. School Issue Brief 5:1 (Jan. 2008) 25 years to grow a mature one • 18-25 “apprentice adults” • Exposure to traumatic stress can affect developmental processes • Increases risk of SA, criminal activity, homelessness and revictimization Early onset of use • Every year before 21 increases likelihood of problem drinking by 12% • Early drinkers need more alcohol to get high Adolescent girls • 1:3 sexually abused by age 16 in U.S. • Youth aged 12-17 have 2xs rate of violent victimization than adults • 2:3 experience direct violence as victims or witnesses to violence Another recent survey showed: • 1:5 girls have been sexually or physically abused • The abuse occurred at home (53%) • It happened more than once (65%) • The abuser was a family member (57%) • Or a family friend (13%) • 29% told no one • Have increased likelihood of SA or eating disorders Infant and Toddler Mental Health • 79.8% of children who die of abuse and neglect were younger than 4 • First year of life the most dangerous • Mental health risks to infants are magnified; they suffer disproportionately yet few referrals are made for children under 5 • 1:5 children in poverty has a diagnosable mental health disorder • “Babies and Toddlers Can Suffer Mental Illness, Seldom Get Treatment,” ScienceDaily (Feb. 23, 2011 Traumatic stress during childhood • • • • Can affect physical/mental health Relationships School performance Risk taking in childhood and as an adult Resources • SAMHSA Report to Congress on The Prevention and Treatment of Co-Occurring Substance Abuse Disorders and Mental Disorders http://www.samhsa.gov/reports/co_occur_ho me.htm Recommendations to Congress • “Any door is the right door” to receive treatment for co-occurring disorders. • Develop client-centered, individualized treatment plans based on accurate assessments. • Ensure the maximum feasible degree of integration for individuals with the most serious substance abuse disorders and mental disorders • Provide prevention and treatment services that are culturally competent, age, sexuality and gender appropriate and that reflect the diversity in the community. • Promote the expansion and enhancement of service providers’ capabilities to treat individuals of all ages who have co-occurring substance abuse disorders and mental disorders. REPORT TO CONGRESS ON THE PREVENTION AND TREATMENT OF CO-OCCURRING SUBSTANCE ABUSE DISORDERS AND MENTAL DISORDERS http://www.samhsa.gov/reports/congress2002/CoOccurringRpt.pdf Co-Occurring Center for Excellence COCE http:coce.samhsa.gov • “Providing integrated services is fundamental to providing quality care. Failure to address co-occurring disorders in either substance abuse or mental health programs is tantamount to ignoring the needs of the majority of participants.” COCE • National co-occurring disorders prevention and treatment cross training and technical assistance • Bring together state-of-the-art information on prevention and treatment services, best practices, and other knowledge-based treatment and evaluation activities TIP 42 Substance Abuse Tx for Persons with Co-Occurring Disorders (SAMHSA) • Key elements for co-occurring disorders in SA Tx agencies and MH agencies • Seeks to coordinate MH & SA services for clients who need both • Good background and statistics https://ncadistore.samhsa.gov/catalog/product Details.aspx?ProductID=16979 Principles of Drug Abuse Treatment for Criminal Justice Populations • Comprehensive assessments should include mental health evaluations with treatment planning for these problems. “17 Step” Programs Dual Diagnosis Anonymous Dual Recovery Anonymous Double Trouble in Recovery Five Steps of Dual Diagnosis 1. We admitted we had a mental illness in addition to our substance abuse and we accepted our dual diagnosis 2. We became willing to accept help for both of our diseases 3. We understood the importance of medical management, clinical interventions and therapies and accepted the need for the total abstinence an sobriety from all nonprescribed drugs and alcohol in our program 4. We came to believe that when our own efforts are combined with the help of others and GOD as we understand Him we will develop healthy drug and alcohol free lifestyles and learn to live at peace with unresolved problems, which is the basic principle of serenity 5. In following the Twelve plus Five Steps of Dual Diagnosis Anonymous, and with the guidance of our Higher Power, a loving GOD of our own understanding combined with the help and direction of our fellow D.D.A., we will maintain healthy drug and alcohol free lifestyles and help others to achieve abstinence. U.S. Conference of Chief Justices Resolution • Urged state supreme court chief justices to "take a leadership role to address the impact of mental illness on the court system through a collaborative effort involving stakeholders from all three branches of government.” • JLI is coordinated by the Council of State Governments (CSG) Criminal Justice/Mental Health Consensus Project and the GAINS/TAPA Center for Jail Diversion. Judges' Criminal Justice/Mental Health Leadership Initiative • JLI is coordinated by the Council of State Governments (CSG) Criminal Justice/Mental Health Consensus Project and the GAINS/TAPA Center for Jail Diversion • CCJ committed to join Jan. 18, 2006. 50:0 COSIGs Co-occurring State Incentive Grants Administered by CSAT and CMHS • Screen individuals for co-occurring disorders • Assess the level of severity • Treat in comprehensive and coordinated manner • Train providers to screen, assess and develop preventive interventions and treatment plans • Evaluate impact of prevention and treatment COSIGs, cont. • $6.5 million in incentive grants available to states to develop and enhance infrastructure to improve treatment for co-occurring disorders • Average award from $500,000 to $1.1 million per year up to 5 years Resources • • • • GAINS Center Consensus Project Judicial Leadership Initiative Evidence-Based Practices, Drake, et al., “Implementing Evidence-Based Practices in Routine Mental Health Service Settings,” Psychiatric Services 52 (2001) Resources, cont. • Bazelon Center for Mental Health Law • NJC Co-Occurring Substance and Mental Health Disorders and Managing Cases with Mental Disabilities courses (www.judges.org) • Second Generation of Mental Health Courts • Redlich, et al., The Second Generation of Mental Health Courts, Psych.Pub.Pol.Law 11(4) 527-538 (2005) Resources, cont. • The Courage to Change: A Guide for Communities to Create Integrated Services for People with Co-Occurring Disorders in the Justice System (National GAINS Center, Dec. 1999) • MH webliography/AOD listserv • judgehora@judgehora.com Resources Resources