Biological Analyses - Biomaterialsengineering.com
advertisement

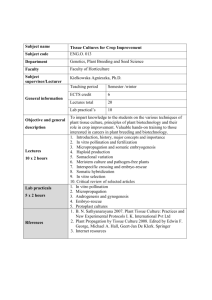
Biomaterials Eng. BIOMEDICAL ENGINEERING BIOMATERIALS Biological Analyses & Sterilization of Biomaterials SECTION 3 1 Biomaterials Eng. Biological analyses For Bachelor Science(B.Sc.) Students Esmaeil Biazar Ph.D in Biomedical Engineering Material attributes for biomedical applications Property Desirables Biocompatibility Noncarcinogenic, nonpyrogenic, nontoxic, nonallergenic, blood compatible, non-inflammatory Sterilizability Not destroyed by typical sterilizing techniques such as autoclaving, dry heat, radiation, ethylene oxide Physical characteristics Strength, elasticity, durability Manufacturability Machinable, moldable, extrudable 2 Adverse Effects Of Biomaterial/Bio-device • B = f (X1,X2......Xn) • Where X: Material, Design, Application etc. 3 Adverse Effects Of Biomaterial/Bio-device Reliability r = 1-f rt = r1 × r2 …… rn Example r ? For Knee replacement after 1 years Fi = 5% , Fw = 3% , Fl= 2% , Fsur= 1% and Ffr=4% r = (1-0.05).(1-0.03).(1-0.02).(1-0.04) = 0.89 4 Human Biomedical Devices Based on the duration of the device use, invasiveness and risk to the user. Class I: crutches, bedpans, tongue depressors, adhesive bandages etc. minimal invasiveness, does not contact the user internally. Class II: hearing aids, blood pumps, catheters, contact lens, electrodes etc. higher degree of invasiveness and risk, but relatively short duration. Class III: cardiac pacemakers, intrauterine devices, intraocular lenses, heart valves, orthopedic implants, etc. considerably more invasive and can pose immense risk to the user-implantables. 5 Human Biomaterials Devices Materials FIRST GENERATION IMPLANTS • “ad hoc” implants. • Specified by physicians using common and borrowed materials. • Most successes were accidental rather than by design. Examples • • • • Gold fillings, wooden teeth, dental prosthesis. Steel, gold, ivory, etc., bone plates. Glass eyes and other body parts. Dacron and parachute cloth vascular implants. 6 SECOND GENERATION IMPLANTS • • • • Engineered implants using common and borrowed materials. Developed through collaborations of physicians and engineers. Built on first generation experiences. Used advances in materials science (from other fields). Examples • Titanium alloy dental and orthopaedic implants. • Cobalt-chromium-molybdinum orthopaedic implants. • UHMW polyethylene bearing surfaces for total joint replacements. • Heart valves and pacemakers. 7 Third generation implants • • • • Bioengineered implants using bioengineered materials. Few examples on the market. Some modified and new polymeric devices. Many under development. Example • Tissue engineered implants designed to regrow rather than replace tissues. • Integra LifeSciences artificial skin. • Genzyme cartilage cell procedure. • Some resorbable bone repair cements. • Genetically engineered “biological” components (Genetics Institute and Creative Biomolecules BMPs). Biological Analyses Objective is to minimize inflammatory responses and toxic effects. • Biocompatibility has been defined as the ability of a medical device to perform with an appropriate host response in a specific application, and biocompatibility assessment is considered to be a measurement of the magnitude and duration of the adverse alterations in homeostatic mechanisms that determine the host response. • Bioactivity – The characteristic that allows the material to form a bond with living tissue (Hench, 1971) – The ability of a material to stimulate healing and trick the tissue system into responding as if it were a natural tissue (Hench 2002). – Advantages: Bone tissue – implant interface, enhanced healing response, extends implant life • Biodegradability – Breakdown of implant due to chemical or cellular actions – If timed to rate of tissue healing transforms implant to scaffold for tissue regeneration – Negates issues of stress shielding, implant loosening, long term stability Biological Analyses • Biology is a science of surfaces and interfaces • Understanding and controlling performance Physical Chemical Biological • Relevant material performance is under biological conditions – 37 ºC, aqueous, saline, Extra Cellular Matrix (ECM) – Material properties as a function of time • Initial negative biological response - toxicity • Long term biological response – rejection – Seldom (never) at equilibrium Host can affect the implant Physically Abrasive, adhesive, delamination wear Fatigue and Fracture Stress Corrosion cracking General corrosion. Biologically Absorption of substances from the tissues Enzymatic degradation Calcification 11 Host can affect the implant Host Factors: Age and health status Immunological/metabolic status Choice of surgeon: minimize tissue damage and contamination, proper implantation. 12 Biological Analyses Material Contact time syringe needle 1-2 s tongue depressor 10 s contact lens 12 hr - 30 days bone screw / plate 3-12 months total hip replacement 10-15 yrs intraocular lens 30 + yrs 13 Biological Analyses Biocompatibility factors Components and natural properties of materials. Tissue type Implantation time Limited X ≤ 24 hrs. Prolonged 24 hrs. < X < 30 days. Permanent X > 30 days. 14 Biological Analyses Screening tests Cytotoxicity Sensitization Irritation or intracutaneous reactivity Acute systemic toxicity Subacute toxicity Genotoxicity Implantation effect Hemocompatibility Chronic toxicity Carcinogenocity Reproductive and developmental toxicity Biodegradation 15 Standards • Assistance in the design of many biomaterials tests is available through national and international standards-organizations. • Thus, the American Society for Testing Materials (ASTM) and the International Standards Organization (IS0) can often provide detailed protocols for widely accepted, carefully thought out testing procedures. • Other testing protocols are available through government agencies (e. g., the FDA) and through commercial testing laboratories. 16 Standards USP (U.S. Pharmacopeia). ISO (International Standard Organization), ISO 10993. FDA ( Food and Drug Administration), Blue Book. AAMI (The Association for the Advancement of Medical Instrumentation). ANSI (American National Standards Institute). BSI (British Standard Institute). NHLBI (National Heart , Lung and Blood Institute). UIPAC (Union for Pure and Applied Chemistry). IACUC (Institutional Animal Care and Use Committee). 17 Standards List of the standards in the 10993 series • ISO 10993-1:2003 Biological evaluation of medical devices Part 1: Evaluation and testing. • ISO 10993-2:2006 Part 2: Animal welfare requirements. • ISO 10993-3:2003 Part 3: Tests for genotoxicity, carcinogenicity and reproductive toxicity. • ISO 10993-4:2002/Amd 1:2006 Part 4: Selection of tests for interactions with blood. • ISO 10993-5:1999 Part 5: Tests for in vitro cytotoxicity. 18 Standards • ISO 10993-6:1994 Part 6: Tests for local effects after implantation. • ISO 10993-7:1995 Part 7: Ethylene oxide sterilization residuals. • ISO 10993-8:2001 Part 8: Selection and qualification of reference materials for biological tests. • ISO 10993-9:1999 Part 9: Framework for identification and quantification of potential degradation products. • ISO 10993-10:2002/Amd 1:2006 Part 10: Tests for irritation and delayed-type hypersensitivity. 19 Standards • ISO 10993-11:2006 Part 11: Tests for systemic toxicity. • ISO 10993-12:2002 Part 12: Sample preparation and reference materials. • ISO 10993-13:1998 Part 13: Identification and quantification of degradation products from polymeric medical devices. • ISO 10993-14:2001 Part 14: Identification and quantification of degradation products from ceramics. • ISO 10993-15:2000 Part 15: Identification and quantification of degradation products from metals and alloys. 20 Standards • ISO 10993-16:1997 Part 16: Toxicokinetic study for degradation products and leachable. • ISO 10993-17:2002 Part 17: Establishment of allowable limits for leachable substances. • ISO 10993-18:2005 Part 18: Chemical characterization of materials. • ISO 10993-19:2006 Part 19: Physico-chemical, morphological and topographical characterization of materials. • ISO 10993-20:2006 21 Part 20: Principles and methods for immunotoxicology testing of medical devices. Standards 22 Biological Analyses BACKGROUND CONCEPTS Toxicity A toxic material is defined as a material that releases a chemical in sufficient quantities to kill cells either directly or indirectly through inhibition of key metabolic pathways. The number of cells that are affected is an indication of the dose and potency of the chemical. Although a variety of factors affect the toxicity of a chemical (e.g., compound, 23 temperature, test system), the most important is the dose or amount of chemical delivered to the individual cell. Biological Analyses BACKGROUND CONCEPTS Delivered and Exposure Doses Delivered dose: the dose that is actually absorbed by the cell. Exposure dose: the amount applied to a test system. • For example, if an animal is exposed to an atmosphere containing a noxious substance (exposure dose), only a small portion of the inhaled substance will be absorbed and delivered to the internal organs and cells (delivered dose). 24 Biological Analyses BACKGROUND CONCEPTS DELIVERED AND EXPOSURE DOSES o The cells that are most sensitive are referred to as the target cells. o Cell culture methods: evaluate target cell toxicity by using delivered doses of the test substance. This distinguishes cell culture methods from whole animal studies, which evaluate the exposure dose and do not determine the target cell dose of the test substance. 25 Biological Analyses BACKGROUND CONCEPTS SAFETY FACTORS • This practice requires being able to exaggerate the anticipated human clinical dosage in the nonhuman test system. • Local toxicity model in animals: there is ample opportunity for reducing the target cell dose by distribution, diffusion, metabolism, and changes in the number of exposed cells (because of the inflammatory response). • Cell culture models: the variables of metabolism, distribution, and absorption are minimized, the dosage per cell is maximized to produce a highly sensitive 26 test system. Biological Analyses BACKGROUND CONCEPTS How can biomaterials be evaluated to determine if they are biocompatible and will function in a biologically appropriate manner in the in vivo environment? This introduction: common to all biomaterials biological testing. 27 Biological Analyses BACKGROUND CONCEPTS Tests IN VITRO EX VIVO IN VIVO 28 Biological Analyses BACKGROUND CONCEPTS IN VITRO • Evaluation under in vitro (literally "in glass") conditions: rapid and inexpensive data on biological interaction . No one material will be appropriate for all medical device application. The material, its composition and degradation products may affect host cells and tissues. The host environment may also affect material properties and device performance. • The question: will the in vitro test measure parameters relevant to what will 29 occur in vivo environment? Biological Analyses BACKGROUND CONCEPTS IN VITRO TESTING Types of in - Vitro tests for estimating biocompatibility : Cytotoxicity – Elution or extract test (MEM Elution) Direct contact test Agar or agarose overlay test Hemocompatibility - Hemolysis assay Clotting and complement activation Mutagenecity – Ames test Hypersensitivity – Lymphocyte transformation test Leukocyte migration & inhibition test 30 Biological Analyses IN VITRO Cytotoxicity • Three primary cell culture assays are used for evaluating biocompatibility (Cytotoxicity): o Direct contact o Agar diffusion o Elution (also known as extract dilution). • These are morphological assays, meaning that the outcome is measured by observations of changes in the morphology of the cells. 31 Biological Analyses IN VITRO DIRECT CONTACT METHOD In this method, a piece of test material is placed directly onto cells growing on culture medium. Cell cultures are grown to a standard monolayer. During incubation, leachable chemicals in the test material can diffuse into the culture medium and contact the cell layer. Subsequently, the monolayers are examined microscopically for the presence of morphological changes, reduction in cell density or lysis of cells around the test material. 32 Biological Analyses IN VITRO DIRECT CONTACT METHOD • A near-confluent monolayer of L-929 mammalian fibroblast cells is prepared in a 35 mm diameter cell culture plate. • Old cell culture media (agar generally) is removed . • Fresh media is added . • Material being tested is placed onto the cultures, which are incubated for 24 hours at 37 degrees Celsius (Incubator in 37 degrees Celsius, 5% CO2 , Humidity 9095%). (Specimen of negative or positive controls and the test article are carefully placed in prepare culture and incubated for 24 hour). • The material is removed . • The culture media is removed . • The remaining cells are fixed and stained by the cytochemical stain. • Dead cells are lost during fixation and only the live cells are stained . • The toxicity of the material is indicated by the absence of stained cells around 33 the material . Biological Analyses IN VITRO AGAR DIFFUSION METHOD In this method, a thin layer of nutrient-supplemented agar is placed over the cultured cells (L-929 mouse fibroblast cells ). The test material (or an extract of the test material dried on filter paper/sample) is placed on top of the agar layer, and the cells are incubated for 24 hours. Cytotoxic leachates diffuse into the cell layer via the agar, and a zone of malformed, degenerative or lysed cells under and around the test material indicates cytotoxicity. 34 Biological Analyses IN VITRO AGAR DIFFUSION METHOD • • • • • • • • A near confluent layer of L-929 mammalian fibroblast cells are prepared in a culture plate . Old cell culture media is removed . The cells are covered with a solution of 2% agar, which often contains red vital stain. After the agar has solidified, specimen of negative and positive controls and the test article are placed on the surface of the same prepared plate and the culture incubated for at least 24 hours (Incubator in 37 degrees Celsius, 5% CO2 , Humidity 90-95%). This assay also contain red stain in the agar mixture, which allows ready visualization of live cells. Healthy cells retain red stain. Dead or injured cells do not retain neutral red and remain colorless. Toxicity is evaluated by the loss of the stain under and around the periphery of the 35 specimens. Biological Analyses IN VITRO ELUTION METHOD • A near confluent layer of L-929 mammalian fibroblast cells are prepared in a culture plate . • An extract of the material which is being tested is prepared using physiological saline (0.9% sodium chloride) or serum-free culture medium (the latter is generally preferred) . • The extract is placed on the cells and incubated for 48 hours at 37 degrees Celsius (Incubator in 37 degrees Celsius, 5% CO2 , Humidity 90-95%). • After 48 hours the toxicity is evaluated using either a histochemical or vital stain. 36 Biological Analyses IN VITRO 37 Biological Analyses IN VITRO ASSAY METHODS • To standardize the methods and compare the results of these assays, the variables: – – – – – – Number of cells. Growth phase of the cells. Cell type. Duration of exposure. Test sample size (e.g., geometry, density, shape, thickness). Surface area of test sample. – Cell morphology Trypan blue (enters dead cells), neutral red (actively taken up by living cells) 38 Biological Analyses IN VITRO 39 Biological Analyses IN VITRO ASSAY METHODS • In general, cell lines that have been developed for growth in vitro are preferred to primary cells that are freshly harvested from live organisms because the cell lines improve the reproducibility of the assays and reduce the variability among laboratories. • That is, a cell line is the in vitro counterpart of inbred animal strains used for in vivo studies. • Cell lines maintain their genetic and morphological characteristics throughout a long (sometimes called infinite) life span. 40 Biological Analyses IN VITRO ASSAY METHODS • Cell lines from other tissues or species may also be used. • Selection of a cell line is based upon the type of assay, the investigator’s experience, measurement endpoints (viability, enzymatic activity, species specific receptors, etc.), and various other factors. • It is not necessary to use human cell lines for this testing because, by definition, these cells have undergone some dedifferentiation and lost receptors and metabolic pathways in the process of becoming cell lines. 41 Biological Analyses IN VITRO Organ of origin Primary cultures or isolated cells Cell lines Nervous system Chick embryo ganglia; chick embryo brain cells; mouse and rat cerebellum cells C 1300 (mouse); C 6 (rat) Lung Human, rabbit and rat alveolar macrophages P 388Dl (mouse); A 549 (human) Reticuloendothelial system Human, mouse lymphocytes and erythrocytes; rat and mouse peritoneal macrophages ------ Liver Rat and chick embryo hepatocytes Chang (human); CC1144 (rat); ARL (rat); RLC-GA (rat) 42 Biological Analyses IN VITRO SPECIAL CELLS Chondrocyte (Cartilage) Epithelial (Skin) Hepatocyte (Liver) Endothelial (Vascular) Osteoblast (Bone) Fibroblast (Connective tissue) Schwann cell (Nerve) 43 Biological Analyses IN VITRO CELL TOXICITY MTT Neutral red assay Calcein assay Alamar Blue Radioisotope 3-H-Leucine assessment Bromodeoxyuridine (BrdU) assessment Lactate dehydrogenase (LDH) assessment MTT (Quantitative cytotoxic assays) Dehydrogenase enzyme: conversion of the water-soluble yellow dye MTT [3-(4,5dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide] to an insoluble purple formazan by the action of mitochondrial reductase (ELISA). Dead cells do not have active mitochondrial reductases (as the cellular reduction is only 44 catalyzed by living cells), MTT is not reduced and the purple formazan is not formed. Biological Analyses IN VITRO Neutral Red (NR) assay Lysosomal activity Membrane permeability The neutral red (NR (3-amino-7-dimethyl-2-methylphenazine hydrochloride)) assay is a cell survival chemo sensitivity assay. This assay is based on the incorporation of NR into the lysosomes of viable cells after being incubation with test agents. Therefore, it is possible to distinguish between viable, damaged or dead cells as viable cells take up the NR dye, damaged or dead cells do not. 45 Biological Analyses IN VITRO • Positive and negative controls are often included in the assays to ensure the operation and suitability of the test system. • The negative control of choice: high-density polyethylene material or TCPS (Tissue Culture Poly Styrene). • The positive controls: low-molecular-weight organo tin-stabilized poly (vinyl chloride), gum rubber, and dilute solutions of toxic chemicals, such as phenol and benzalkonium chloride. 46 Biological Analyses IN VITRO The in vitro cytotoxicity assays are the primary biocompatibility screening tests for a wide variety of elastomeric, polymeric, and other materials used in medical devices. After the cytotoxicity profile of a material has been determined, then more application specific tests are performed to assess the biocompatibility of the material. 47 Biological Analyses IN VITRO HEMOCOMPATIBILITY TESTS Are used to evaluate the effect of a material on blood coagulation processes, thrombus formation and hemolysis (destruction of red blood cells). Materials or theirs extracts are incubated with red blood cells, isolated from rabbits, mice, or rats for three hours with intermittent shaking to keep samples mixed and in contact with blood. The amount of hemoglobin released into the supernatant from the cells is determined spectrophotometrically and reported as percent hemolysis with respect to negative controls. To evaluate the effect of materials and their surfaces on blood clotting, materials are exposed to whole blood serum. Turbulent flow of blood may increase hemolysis and or clotting – the number of adherent platelets may be determined per unit area after exposure 48 to whole blood. Biological Analyses IN VITRO MUTAGENECITY AND GENOTOXICITY Mutagenes – modify the genome of a host, so materials may be classified as genotoxic. It is widely accepted that carcinogenic behavior proceeds via a mutation in the genome. Ames test – uses a mutant bacterial cell line (Salmonella typhimurium or Escherichia coli) that must be supplied with histidine to growth. The cells are cultured in histidine-free environment and only those material that mutate the cells back to state of histidine indipendence will allow the cells back to grow. Styles test (Fibroblast cell deformation , Agar gel) Hypersensitivity Tests – the leukocyte migration inhibition and lyphocyte transformation tests have been used as in-vitro models to estimate delayed hypersensitivity reaction to implant materials and their released components. 49 Biological Analyses IN VITRO CONSIDERATIONS Choice of cells Conformity of Biomaterials to tissue Repetition (Number of replicates) Statically evaluations (P-value) CAS (Cell Analysis System) or Image Pro Plus 50 Biological Analyses IN VITRO • In vitro tests minimize the use of animals in research, a desirable goal. • Also, in vitro testing is required by most regulatory agencies in the device approval process for clinical application. • When appropriately used, in vitro testing provides useful insights that can dictate whether a device need be further evaluated in expensive in vivo experimental models. 51 Biological Analyses IN VITRO • • • • • • In vitro tests minimize the use of animals in research, a desirable goal. Also, in vitro testing is required by most regulatory agencies in the device approval process for clinical application. When appropriately used, in vitro testing provides useful insights that can dictate whether a device need be further evaluated in expensive in vivo experimental models. Current experience indicates that a material that is judged to be nontoxic in vitro will be nontoxic in in vivo assays. This does not necessarily mean that materials that are toxic in vitro could not be used in a given clinical application. The clinical acceptability of a material depends on many different factors, of which target cell toxicity is but one. For example, glutaraldehyde-fixed porcine valves produce adverse effects in vitro owing to low residues of glutaraldehyde; however, this material has the greatest clinical efficacy for its unique application. 52 Biological Analyses IN VITRO Advantages Low expense Low work High speed High reproducibility Cell and tissue (biopsy) access High Performability 53 Biological Analyses IN VIVO The goal of in vivo assessment of tissue compatibility of a biomaterial, prosthesis, or medical device is to determine the biocompatibility or safety of the biomaterial, prosthesis, or medical device in a biological environment. • From a practical perspective, the in vivo assessment of tissue compatibility of medical devices is carried out to determine that the device performs as intended and presents no significant harm to the patient or user. • Thus, the goal of the in vivo assessment of tissue compatibility is to predict whether a medical device presents potential harm to the patient or user by evaluations under conditions simulating clinical use. 54 Biological Analyses IN VIVO 55 Biological Analyses IN VIVO SENSITIZATION, IRRITATION, AND INTRACUTANEOUS (INTRADERMAL) REACTIVITY • Exposure to or contact with even minute amounts of potential leachables from medical devices or biomaterials can result in allergic or sensitization reactions. • Sensitization tests estimate the potential for contact sensitization to medical devices, materials, and/or their extracts. • Symptoms of sensitization are often seen in skin and tests are often carried out topically in guinea pigs. 56 Biological Analyses IN VIVO SENSITIZATION, IRRITATION, AND INTRACUTANEOUS (INTRADERMAL) REACTIVITY • The most severely irritating chemical leachable may be discovered prior to in vivo studies by careful material characterization and in vitro cytotoxicity tests. • Irritant tests emphasize utilization of extracts of the biomaterials to determine the irritant effects of potential leachable. • Intracutaneous (intradermal) reactivity tests determine the localized reaction of tissue to intracutaneous injection of extracts of medical devices, biomaterials, or prostheses in the final product form. • Intracutaneous tests may be applicable where determination of irritation by dermal or mucosal tests are not appropriate. • Albino rabbits are most commonly used. 57 Biological Analyses IN VIVO Systemic Toxicity Acute, Subacute, and Subchronic Toxicity Mice, rats, or rabbits are the usual animals of choice for the conduct of these tests and oral, dermal, inhalation, intravenous, intraperitoneal, or subcutaneous application of the test substance may be used, depending on the intended application of the biomaterial. 58 Biological Analyses IN VIVO SYSTEMIC TOXICITY ACUTE, SUBACUTE, AND SUBCHRONIC TOXICITY • Acute toxicity is considered to be the adverse effects that occur after administration of a single dose or multiple doses of a test sample given within 24 hours. • Subacute toxicity (repeat-dose toxicity) focuses on adverse effects occurring after administration of a single dose or multiple doses of a test sample per day during a period of from 14 to 28 days. 59 Biological Analyses IN VIVO SYSTEMIC TOXICITY ACUTE, SUBACUTE, AND SUBCHRONIC TOXICITY • Pyrogenicity tests are also included in the systemic toxicity category to detect material-mediated fever-causing reactions to extracts of medical devices or materials. • It is noteworthy that no single test can differentiate pyrogenic reactions that are material-mediated from those due to endotoxin contamination. 60 Biological Analyses IN VIVO GENOTOXICITY • In vivo genotoxicity tests are carried out if indicated by the chemistry and/or composition of the biomaterial or if in vitro test results indicate potential genotoxicity [changes in deoxyribonucleic acid (DNA)]. • Initially, at least three in vitro assays should be used and two of these assays should utilize mammalian cells. • The initial in vitro assays should cover the three levels of genotoxic effects: – DNA destruction. – Gene mutations. – Chromosomal aberrations. 61 Biological Analyses IN VIVO IMPLANTATION 62 Biological Analyses IN VIVO IMPLANTATION • For short-term implantation evaluation out to 12 weeks, mice, rats, guinea pigs, or rabbits are the usual animals utilized in these studies. • For longer-term testing in subcutaneous tissue, muscle, or bone, animals such as rats, guinea pigs, rabbits, dogs, sheep, goats, pigs, and other animals with relatively long life expectancy are suitable. 63 Biological Analyses IN VIVO IMPLANTATION • If a complete medical device is to be evaluated, larger species may be utilized so that human-sized devices may be used in the site of intended application. For example – substitute heart valves are usually tested as heart valve replacements in sheep, – whereas calves are usually the animal of choice for ventricular assist devices and total artificial hearts. 64 Biological Analyses IN VIVO IMPLANTATION Haematoxylin and eosin (H&E) staining Ziehl-Neelsen stain Papanicolaou staining Masson's trichrome …. Haematoxylin and eosin (H&E) staining 65 Biological Analyses IN VIVO HEMOCOMPATIBILITY OR BLOOD COMPATIBILITY • Hemocompatibility tests evaluate effects on blood and/or blood components by blood-contacting medical devices or materials. • In vivo hemocompatibility tests are usually designed to simulate the geometry, contact conditions, and flow dynamics of the device or material in its clinical application. • From the IS0 standards perspective, five test categories are indicated for hemocompatibility evaluation : Thrombosis, coagulation, platelets, hematology, and immunology (complement and leukocytes). 66 Biological Analyses IN VIVO HEMOCOMPATIBILITY In vivo testing in animals may be convenient, but species' differences in blood reactivity must be considered and these may limit the predictability of any given test in the human clinical situation. 67 Biological Analyses IN VIVO CHRONIC TOXICITY Chronic toxicity tests determine the effects of either single or multiple exposures to medical devices, materials, and/or their extracts during a period of at least 10 % of the lifespan of the test animal, e.g. over 90 days in rats. Chronic toxicity tests may be considered an extension of subchronic (subacute) toxicity testing and both may be evaluated in an appropriate experimental protocol or study. 68 Biological Analyses IN VIVO CARCINOGENICITY • Carcinogenicity tests determine the tumorigenic potential of medical devices, materials, and/or their extracts from either single or multiple exposures or contacts over a period of the major portion of the lifespan of the test animal. • Since tumors associated with medical devices have been rare carcinogenicity tests should be conducted only if data from other sources suggest a tendency for tumor induction. • In addition, both carcinogenicity (tumorigenicity) and chronic toxicity may be studied in a single experimental study. 69 Biological Analyses IN VIVO REPRODUCTIVE AND DEVELOPMENTAL TOXICITY • These tests evaluate the potential effects of medical devices, materials, and/or their extracts on reproductive function, embryonic development (teratogenicity), and prenatal and early postnatal development. • The application site of the device must be considered and tests and/or bioassays should only be conducted when the device has a potential impact on the reproductive potential of the subject. 70 Biological Analyses IN VIVO BIODEGRADATION Biodegradation tests determine the effects of a biodegradable material and its biodegradation products on the tissue response. • They focus on: – The amount of degradation during a given period of time (the kinetics of biodegradation). – The nature of the degradation products. – The origin of the degradation products (e. g., impurities, additives, corrosion products, bulk polymer). – The qualitative and quantitative assessment of degradation products and leachable in adjacent tissues and in distant organs. 71 Biological Analyses IN VIVO IMMUNE RESPONSE • Immune response evaluation is not a component of the standards currently available for in vivo tissue compatibility assessment. • However, ASTM, IS0, and the FDA currently have working groups developing guidance documents for immune response evaluation where pertinent. • Synthetic materials are not generally immunotoxic. • However, immune response evaluation is necessary with modified natural tissue implants such as collagen, which has been utilized in a number of different types of implants and may elicit immunological responses. 72 Biological Analyses IN VIVO SELECTION OF ANIMAL MODELS FOR IN VIVO TESTS • Animal models are used to predict the clinical behavior, safety, and biocompatibility of medical devices in humans. • The selection of animal models for the in vivo assessment of tissue compatibility must consider the advantages and disadvantages of the animal model for human clinical application. • Several examples follow, which exemplify the advantages and disadvantages of animal models in predicting clinical behavior in humans. 73 Biological Analyses IN VIVO 74 Biological Analyses IN VIVO SELECTION OF ANIMAL MODELS FOR IN VIVO TESTS Thus, the choice of this animal model for bio prosthetic heart valve evaluation is made on the basis of accelerated calcification in rapidly growing animals, which has its clinical correlation in young and adolescent humans. Nevertheless, normal sheep may not provide a sensitive assessment of the propensity of a valve to thrombosis. 75