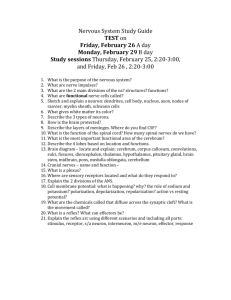
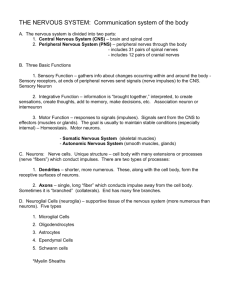
Nervous System

FUNCTION OF THE NERVOUS SYSTEM
Directs internal processes
Link to the external environment
TWO DIVISIONS OF THE NERVOUS SYSTEM
CENTRAL NERVOUS
SYSTEM (CNS)
Composed of brain and spinal cord
Controls entire organism
Integrates incoming info and responses
Dependent upon the
PNS
PERIPHERAL NERVOUS
SYSTEM (PNS)
Link between CNS, body and environment
Spinal and cranial nerves
Composed of sensory and motor divisions
Sensory:
Somatic afferents
Visceral afferents
Motor:
somatic nervous system
autonomic nervous system
TWO DIVISIONS OF THE NERVOUS SYSTEM
DIVISIONS OF THE NERVOUS SYSTEM
DIVISIONS OF THE PNS
SOMATIC NERVOUS SYSTEM (Voluntary)
Conducts impulses from the CNS to skeletal muscles
AUTONOMIC NERVOUS SYSTEM
Innervates smooth muscle (internal organs), glands and cardiac muscle
Maintains homeostasis
DIVISIONS OF THE AUTONOMIC N.S.
AUTONOMIC NERVOUS
SYSTEM
Sympathetic N.S.
“ Flight or fright system”
Inhibits digestion
Dilates pupils
Accelerates heart and respiration rate
Parasympathetic N.S.
Brings functions back to normal
Contracts pupils
Promotes digestion
Returns heart and respiration rate to normal
NERVOUS SYSTEM CELL TYPES
NEURONS
Excitable
Conduct nerve impulses
Amitotic
NERVOUS SYSTEM CELL TYPES
NEUROGLIA (Glial cells)
Supporting cells
Surround neurons
Nonconducting
6 types
2 in PNS
4 in CNS
Astrocyte
Oligodendrocyte
Ependymal Cells Microglia Schwann Cells
SUPPORTING CELLS OF THE CNS
1) Astrocytes
In CNS only
Anchor neurons to capillaries
Pick up excess K +
Recapture released neurotransmitters capillary
SUPPORTING CELLS OF THE CNS
2) Oligodendrocytes
CNS only
Wrap extensions around neuron fibers (axons)
Form myelin sheath axon
SUPPORTING CELLS OF THE CNS
3) Ependymal Cells
CNS only
Line the cavities of the brain and spinal cord
Ciliated
Circulate the cerebrospinal fluid
(CSF)
SUPPORTING CELLS OF THE CNS
4) Microglia
CNS only
Migrate toward injured neurons
Phagocytic cells
Devour microorganisms or debris from damaged neurons neuron
SUPPORTING CELLS OF THE PNS
1) Schwann Cells
PNS only
Wrap around axons of neurons in the PNS
Form myelin sheath
Needed for axon regeneration myelin sheath axon
SUPPORTING CELLS OF THE PNS
2) Satellite Cells
PNS only
Surround neuron cell bodies
Help control the chemical environment neuron cell body
NEURON STRUCTURE
Cell Body (soma or perikaryon )
Contains typical cell organelles (no centrioles)
Abundant clusters of rER called nissl bodies
Nerve Processes (Neurites)
Dendrites
Short, branched extensions
Receive input (receptive)
Axon (nerve fiber)
Conducting extension
NEURON STRUCTURE
Axon (Nerve Fiber)
Abundant organelles
No nissl bodies
Axon hillock
Enlarged part of cell body
Axoplasm
Cytoplasm
Axolemma
Plasma membrane
NEURON STRUCTURE
Axon terminal = synaptic knobs or terminal boutons
Bulb-like ends of the telodendria
Telodendria (terminal branches)
Profuse branches at the end of the axon
Axon collaterals
Large branches of the axon
NEURON STRUCTURE
Myelin sheath
Node of Ranvier
Neurilemma
Schwann cell
NEURON STRUCTURE
Presynaptic neuron
Synapse
Postsynaptic neuron
CLASSIFICATION OF NEURONS
Neurons can be classified by structure:
Multipolar
Most common in CNS and
PNS
Single axon, numerous dendrites (motor neurons and interneurons of CNS)
Bipolar
One dendrite, one axon
(sensory neurons found in the retina, olfactory receptors)
Unipolar
Single fiber functions as both dendrite and axon (sensory neurons , dorsal root ganglia)
CLASSIFICATION OF NEURONS
Neurons can be classified by function:
Afferent (sensory)
Carry info from receptors towards CNS
Efferent (motor)
Carry info from CNS to muscles or glands
Association or Interneurons
Link sensory and motor neurons
Make up 99% of neurons in body
OTHER NERVOUS SYSTEM STRUCTURES
Ganglion
Clusters of neuron cell bodies in the PNS
Nuclei
Clusters of neuron cell bodies in the CNS (gray matter)
Tract
Bundles of nerve fibers together in the CNS
Nerve
Bundles of nerve fibers (axons) traveling together in the PNS
NERVE STRUCTURE endoneurium
Epineurium
Connective tissue surrounding the entire nerve
Perineurium perineurium
C.T. surrounding a bundle of axons
(fascicle)
Endoneurium epineurium
C.T. surrounding each individual axon
NEURON FUNCTION: The Synapse
Synapse
Junction between one neuron and another
Most are axodendritic or axosomatic
Two types:
Electrical
Chemical
TYPES OF SYNAPSES
Electrical Synapses
Not common
Protein channels connect pre-synaptic neuron directly to postsynaptic neuron
Ions flow from one neuron to the next
Rapid transmission
In some brain areas, cardiac and smooth muscle
Chemical Synapses
Most are this type
Neurotransmitter released from synaptic knob of pre-synaptic neuron
Neurotransmitter binds to receptors on membrane of post-synaptic neuron
Binding of the neurotransmitter to receptor permeability change in postsynaptic neuron cell membrane
NEUROTRANSMITTERS
Action Potential
Ca 2+ ions axon axon terminal synaptic cleft
Released at chemical synapses
Chemicals produced in the cell body or synaptic knob of the neuron
Stored in synaptic vesicles in the synaptic knob
Nerve impulse causes release of neurotransmitter into synaptic cleft
NEUROTRANSMITTERS
When bound to receptors on the postsynaptic neuron, the neurotransmitter can either excite or inhibit the postsynaptic neuron
THE RESTING MEMBRANE POTENTIAL
Na + k +
Na + k +
Na +
Na +
Na +
+
+
+
+
+
+
+
+
+
+
+
+
–
–
–
–
–
–
–
–
–
–
–
–
Na + k +
Na + k +
Na +
Inside of cell membrane is more negative than outside
Due to the presence of more positive ions (Na + ) outside the cell
Difference between charge inside and outside cell membrane = RESTING
MEMBRANE POTENTIAL
(RMP)
RMPs vary from -40 to -90mV in different neuron types
EXCITATORY NEUROTRANSMITTERS
When bound to receptors on the postsynpatic neuron membrane:
Causes the opening of positive ion channels
Sodium ions enter rapidly
RMP becomes more positive
This positive change in the
RMP is called depolarization
This brings the neuron closer to firing neurotransmitter sodium receptor ion channel potassium
k +
Na +
Na +
– +
– +
– +
Na +
Na + k +
Na +
Na +
Na +
Na +
Na + k + k +
Na +
DEPOLARIZATION
Na +
Na +
A positive change in the
RMP
Caused by influx of positive ions
Causes the inside of the cell membrane to become less negative
This sudden positive change in the membrane potential is called
DEPOLARIZATION
Depolarization spreads to adjacent areas
INHIBITORY NEUROTRANSMITTERS
When bound to receptors on the postsynaptic membrane:
Make membrane more permeable to negative ions (usually Cl )
As negative ions rush into neuron, the
RMP becomes more negative
The negative change in the RMP is called hyperpolarization
This brings the neuron farther away from firing
HYPERPOLARIZATION
Na +
Na +
Cl k +
Cl -
Cl k +
Na +
Na +
Cl -
+
+
+
+
+
+
+
+
+
+
+
+
–
–
–
–
–
–
–
–
–
–
–
–
Cl -
Na +
Cl -
Cl k +
Na + k +
Na +
A negative change in
RMP
Usually caused by influx of chloride ions
Decreases the likelihood of the neuron firing
GRADED POTENTIALS
Short changes in the RMP in small regions of the membrane
Can be positive changes or negative changes (they can depolarize or hyperpolarize the membrane)
Alone, not strong enough to cause a nerve impulse to fire
Together, can trigger a nerve impulse (action potential) stimulus depolarized region depolarization wave
POSTSYNAPTIC POTENTIALS
EPSP (Excitatory Postsynaptic Potential)
A local graded potential
Binding of a neurotransmitter on the postsynaptic membrane results in a more positive RMP (depolarization occurs)
The neuron is brought closer to firing
POSTSYNAPTIC POTENTIALS
IPSP (Inhibitory Postsynaptic Potential)
A local graded potential
Binding of the neurotransmitter on the postsynaptic membrane results in a more negative RMP (hyperpolarization)
Inhibits the neuron from firing an impulse
TYPES OF NEUROTRANSMITTERS
40 to 50 Known Neurotransmitters
Acetylcholine (Ach)
Released from cholinergic neurons
Norepinephrine (NE)
Released by adrenergic neurons
GABA
Dopamine
Serotonin
ACTION POTENTIALS
Action Potential = Nerve Impulse
Consists of:
Depolarization
Propagation
Repolarization
ACTION POTENTIALS
If depolarization of the membrane reaches threshold (usually a positive change of 15 to 20 mV or more), an action potential is triggered
The positive RMP change causes electrical gates in the axon hillock to open
A sudden large influx of sodium ions causes a reversal in the membrane potential (becomes approx. 100mV more positive)
Begins at the axon hillock and travels down the axon
TYPES OF ION CHANNELS
Chemically Gated
Voltage Gated
PROPAGATION
Movement of the action potential down the membrane of the axon
Caused by electrically gated sodium channels opening in response to the positive RMP change
Axon hillock
REPOLARIZATION
Restoration of the RMP back to it’s negative state
A repolarization wave follows directly behind the depolarization wave
3 factors contribute to restoring the negative membrane potential:
Sodium (Na + ) gates close (it no longer enters)
Potassium (K + ) gates open, potassium rushes out
Sodium/potassium pump kicks in
THE SODIUM/POTASSIUM PUMP
An active process that requires cellular energy
Actively pumps 3 sodium (Na +) ions out of the cell and 2 potassium
(K +) ions in
Potassium freely leaks back out of the cell
ABSOLUTE REFRACTORY PERIOD
Period of time when electrical sodium gates are open
The neuron is incapable responding to a stimulus no matter how strong
SUMMATION BY POSTSYNAPTIC NEURON
A single EPSP cannot induce an action potential
EPSP’s can add together or SUMMATE to influence a postsynaptic neuron in initiation of an action potential
Spatial Summation
Large numbers of axon terminals stimulate the postsynaptic neuron at the same time
Temporal Summation
One or more presynaptic neurons transmit impulses in rapid fire succession
ALL-OR-NONE RESPONSE
An action potential is an “ all or none ” phenomenon
When threshold is reached, the action potential will happen completely
If threshold is not reached, the action potential will not occur at all
SALTATORY CONDUCTION
Occurs only in myelinated axons
Depolarization wave jumps from one node of
Ranvier to the next
Results in faster nerve impulse transmission
SUMMARY OF EVENTS
A nerve impulse in the presynaptic neruon causes release of neurotransmitter into synaptic cleft
Neurotransmitter binding to receptors on postsynaptic neuron dendrite or soma cause certain chemically gated ions to open
If Na + channels open:
Rapid influx of Na + ions ( depolarization )
A small positive graded potential occurs ( EPSP )
If RMP changes in a positive direction by 20mV ( or reaches the threshold ), voltage gated sodium channels in the axon hillock open
Sodium rushes in at the axon hillock resulting in an action potential
As the positive ions get pushed down the axon, more voltage gated sodium channels open and the depolarization continues down the axon ( propagation )
The process of restoring the negative RMP begins immediately following the depolarization wave
( repolarization )
NERVE FIBER TYPES
The larger the axon diameter, the faster the impulse travels
Myelinated axons conduct impulses more rapidly
Fiber Types:
Type A fibers
Large diameter axon with thick myelin sheath
Impulse travels at 15 to 150 m/sec.
Sensory and motor fibers serving skin, muscles, joints
Type B fibers
Intermediate diameter axon, lightly myelinated
Impulse travels at 3 to 15 m/sec.
Type C fibers
Small axon diameter, unmyelinated
Slow impulse conduction (1 m/sec. or less)
NERVE FIBER TYPES
Type C Fiber
Type B Fiber
Type A Fiber
NEURONAL CIRCUITS
Diverging Circuits
One incoming fiber triggers responses in increasing numbers of neurons farther down the circuit
NEURONAL CIRCIUTS
Converging Circuits
Many incoming fibers send impulses to the same neuron
REFLEX ARCS
Neural pathways with 5 components:
Receptor
Sensory neuron
CNS integration center
Motor neuron
Effector
A rapid, automatic response to a stimulus
Divisions of the Brain
Brainstem
Medulla oblongata (1)
Pons (2)
Midbrain (3)
Diencephalon (4)
Thalamus
Hypothalamus
Epithalamus
Cerebellum (5)
Cerebrum (6)
6
4
3
2
1
5
The Cerebrum: Regions
In anterior and middle cranial fossa
Six lobes
1
Frontal (1)
Parietal (2)
Occipital (3)
Temporal (4)
Limbic (5)
Insula (6)
5
4
Many functions in various regions
6
2
3
Protection of the CNS
Structures that help to protect the brain and spinal cord:
Skull bones
Vertebrae
Cerebrospinal Fluid (CSF)
Bathes and cushions
Meninges
Three connective tissue membranes surrounding the brain and spinal cord
Cerebrospinal Fluid
Flows around and in the brain and spinal cord
99% water
Also sugar ( glucose ), chlorides, proteins, ions, vitamin C
Total volume of 150 ml
( replaced every 3 to 4 hrs .)
900 to 1200 ml formed daily
Formed by choroid plexuses in the brain ventricles wastes ependymal cells capillary glucose,
O
2 ions choroid plexus
Three Layers of Meninges
Dura Mater
Most superficial
Tough, double-layered membrane
Outer layer is fused to skull
In some areas the layers separate to enclose dural sinuses
Extends inward in some areas forming septa to anchor the brain to the skull dura mater dural sinus
Dural Septa
Dural Septa
Falx cerebri
Falx cerebelli
Tentorium cerebelli falx cerebri tentorium cerebelli falx cerebelli
Dural Spaces
Subdural space
Space below dura and above arachnoid layer below
Epidural space
Space between bone and the dura
( above the dura )
Not present in the skull
Three Layers of Meninges
Arachnoid (Mater) Layer
Deep to dura
Web-like extensions down to pia mater below
Subarachnoid space
Space below arachnoid membrane
Filled with CSF
Numerous blood vessels
Arachnoid villi (granulations)
Drain CSF into dural sinuses arachnoid
Three Layers of Meninges
Pia Mater
Innermost layer
Adheres to brain and spinal cord
Follows folds of brain
Very vascular
Small extension of pia called the filum terminale fastens the spinal cord down to the coccyx bone pia mater
Blood-Brain Barrier
Barrier formed by astrocytes and endothelial lining of brain capillaries
Prevents cellular wastes from entering brain tissue capillary astrocyte
Disorders of the Meninges
Hydrocephalus
Build up of CSF due to blockage or obstruction
Exerts pressure on the brain
Can cause permanent brain damage
Meningitis
Inflammation of the meninges caused by a viral or bacterial infection
May spread to nervous tissue of CNS
Encephalitis
Brain tissue inflammation
Fatal 50% of the time
Brain Ventricles
Interconnected chambers within the brain
Filled with CSF
Four ventricles:
1 st and 2 nd (Lateral) Ventricles
Anterior, inferior and posterior horns
3 rd Ventricle
Within diencephalon
Connected to 4 th ventricle by the cerebral aqueduct
4 th Ventricle
Dorsal to pons and medulla
Opens into central canal of spinal cord and subarachnoid space around brain
1
4
3
2
Spinal Cord
Function
Controls reflex activities
Transmits info. from peripheral nerves to brain and back
Structure
Runs from the foramen magnum to L
1 or L
2
Cervical and lumbar enlargements
31 pair of spinal nerves emerge from the cord
Spinal Cord Structure
Filum Terminale
Extension of pia mater attaching the cord to the coccyx
Conus Medullaris
Caudal end of spinal cord
Cauda Equina
Nerves from the lower cord running inferior before exiting the vertebrae conus medullaris filum terminale cauda equina
Spinal Cord Structure
Gray Matter
In the interior of the cord
Forms an ‘H’ shape
Ventral Horns
To anterior projections of gray matter
Contain cell bodies of large alpha motor neurons gray matter ventral horns
Spinal Cord: Gray Matter
Dorsal Horns
Incoming unipolar sensory neurons enter and synapse with association neurons
Cell bodies of these sensory neurons are in the dorsal root ganglia lateral horn
Lateral Horns
Only visible from T
1 to L
2
Contain autonomic neuron cell bodies dorsal horns
Spinal Cord: Structure
Gray commissure
Connects right and left halves of gray matter
External fissures
Anterior median fissure
Posterior median sulcus anterior median fissure posterior median sulcus gray commissure
Spinal Cord: Structure
White matter
Divided into columns called columns or funiculi
Anterior, lateral and dorsal white columns or funiculi lateral funiculus anterior funiculus posterior funiculus
Spinal Cord Tracts
Ascending Tracts
Spinothalamic
Ascending afferent sensory fiber tract
Info regarding pain, temperature and crude touch
Spinocerebellar
Afferent sensory tract
Carries info regarding movement and limb position spinocerebellar spinothalamic
Spinal Cord Tracts
Ascending Tracts
Fasciculus cuneatus & Fasciculus gracilis
Afferent sensory tract
Carries info from skin, joints and muscles concerning discriminative touch, pressure, vibration and body position fasciculus cuneatus fasciculus gracilis
Spinal Cord Tracts
Descending Tracts
Corticospinal
Descending efferent fiber tract
Carry info for voluntary movement of skeletal muscle corticospinal corticospinal
Reflex Actions
An automatic response to a specific stimulus
Reflex Arcs
Most don’t involve conscious thought
Some involve lower brain
Some are carried out by the spinal cord without any brain involvement
Types of Reflexes
Monosynaptic Reflexes
Chain of only 2 neurons involved
Example: Patellar reflex (stretch reflex)
– Quadriceps tendon stretched muscle spindles send impulse (muscle stretching)
spinal cord
motor neuron
quadriceps muscle contracts
Stretch Reflex
Types of Reflex
Polysynaptic Reflexes
Require 3 or more sets of neurons
Example: Withdrawal reflex ( crossed extensor reflex )
–
Pain receptors
spinal cord
association neuron
integration
motor neurons (to muscles for contraction)
flexors contract
extensors extend for balance
Crossed Extensor Reflex
Referred Pain
Perceived by the brain as pain from an extremity or body region rather than visceral pain
Blood Supply To The Brain
Circle of Willis
Circular network of blood vessels supplying the brain
2 vertebral, 2 internal carotid arteries contribute
Many anastamoses help curtail inadequate blood supply to the brain
The Cerebrum: Gray Matter
Cerebral Cortex
Gray matter
Neuron cell bodies
Outer layer of cerebrum
Gray matter also in basal nuclei gray matter
The Cerebrum: Basal Nuclei
Also called basal ganglia
Areas of gray matter deep within the cerebrum
Putamen, globus pallidus, caudate nucleus caudate nucleus lentiform nucleus
( putamen + globus pallidus )
The Cerebrum: Basal Nuclei
Receive input from cerebral cortex caudate nucleus
Project messages through thalamus to premotor and prefrontal areas
monitor and regulate movements from motor cortex
Regulate intensity of movements, inhibit unnecessary movements lentiform nucleus putamen globus pallidus
The Cerebrum: Gyri and Sulci
Gyri (gyrus)
Folds or hills in the cerebral tissue longitudinal fissure
Sulci (sulcus)
Shallow grooves or valleys
Fissures central sulcus
Deeper grooves and valleys precentral gyrus
The Cerebrum: Gyri
Gyri
Precentral gyrus (1)
Postcentral gyrus (2)
Superior temporal gyrus (3)
Cingulate gyrus (4)
3
1
2
4
The Cerebrum: Sulci
Sulci
Central sulcus (1)
Lateral (Sylvian) sulcus or fissure (2)
Parieto-occipital sulcus (3)
Calcarine sulcus (4)
2
1
3
4
The Cerebrum: Fissures
Fissures
Longitudinal fissure (1)
Transverse fissure (2)
1
2
The Cerebrum: White matter
association fibers White matter = myelinated axons
Three types of fibers in cerebral white matter:
Association fibers
Travel to other areas in the same hemisphere
The Cerebrum: White Matter commissural fibers
Commissural fibers
Connect areas from one hemisphere to the other hemisphere
Projection fibers
Descend from cortex towards lower brain or spinal cord projection fibers
The Cerebrum: White Matter
corpus callosum
Commissures
Regions with commissural fibers
Corpus callosum
Anterior commissure fornix anterior commissure
Cerebrum: Functions
Three Functional Types of Areas Within the
Cerebrum:
À Sensory Areas
Conscious awareness of sensations
Motor Areas
Control voluntary functions
Association Areas
Integrate information for a purposeful action
Frontal Lobe
Cerebral Lobes: Function
Primary Motor Cortex (1)
Precentral gyrus
Allows conscious control of skeletal muscle
Contralateral innervation
2 1
Premotor Area (2)
Controls learned, repetitious motor skills
3
Broca’s Area (3)
Directs the movement of muscles involved in speech
(lips, tongue, throat)
Cerebral Lobes: Function
Parietal Lobe
Primary Somatosensory
Cortex (4)
Postcentral gyrus
Receives input from sensory receptors in skin, muscles
I.D. body region input is from
Sensory Association Area (5)
Integrates and analyzes sensory input
Evaluates size, texture, relationships etc.
4
5
Cerebral Lobes: Function
Occipital Lobe
Primary Visual Cortex (6)
Posterior occipital lobe
( calcarine sulcus )
Receives input from retina
Info relayed through lateral geniculate body of thalamus
Visual Association Area (7)
Surrounds visual cortex
Interprets visual inputs, uses past experiences
Allows for visual recognition
7
6
Cerebral Lobes: Function
Temporal Lobe
Primary Auditory
Cortex (8)
Superior temporal gyrus
Receives info. from receptors in inner ear for sound
8
Auditory Association
Area (9)
Uses memories of sounds for sound recognition
9
Cerebral Lobes: Function
Posterior Temporal Lobe
Wernicke’s Area (11)
Understanding written and spoken language
Sounding out unfamiliar words
10
Cerebrum: functions
Limbic Lobe
Cingulate gyrus, parahippocampal gyrus, hypothalamus and part of the thalamus
“Emotional brain”
Extensive link to lower and higher brain areas
Allows emotional and visceral responses to things we are consciously aware of cingulate gyrus hypothalamus parahippocampal gyrus
Cerebral Lobes: Function
Insula
Deep within the cerebrum in area deep to lateral sulcus
May be involved with autonomic and somatic activities lateral sulcus insula
The cerebrum
Aphasias
Inability to speak in grammatical sentences due to lesions in Broca’s area
Electroencephalograph (EEG)
Used to trace patterns of brain activity
Can be used to detect regions where seizures are occurring
Diencephalon
Consists of the
Thalamus, Hypothalamus and Epithalamus
Thalamus
Makes up 80% of the diencephalon
Two large gray masses connected by the intermediate mass
Contains many nuclei
Projects fibers to and from the cortex
Sorts and edits info. headed for the cortex
Directs info. to proper cortical region thalamus intermediate mass of thalamus
The Diencephalon
Hypothalamus
Initiates physical expression of emotions (linked to the limbic system)
Regulates thirst, food intake, body temp., sexual behavior, pleasant and painful feelings, pleasure, fear, rage
Regulates autonomic centers in the brain stem controlling B.P., digestive rate, respiration rate hypothalamus
The Diencephalon
Hypothalamus
Infundibulum
Stalk connecting the hypothalamus to the pituitary gland
Mammillary bodies
Relay station for olfactory pathways infundibulum mammillary body
The Diencephalon
Hypothalamus
Supraoptic Nucleus
Contains neurons that produce ADH (antidiuretic hormone)
Paraventricular Nucleus
Contains neurons that produce oxytocin
– Stimulates uterine contractions in labor and milk ejection for nursing paraventricular nucleus
Supra-optic nucleus
The Diencephalon
Other structures in the region
Optic chiasma
Pituitary gland (hypophysis)
Diaphragma sella optic chiasma hypophysis
The Diencephalon
Epithalamus
Pineal gland
Secretes melatonin
Helps regulate sleep/wake cycles
May be influenced by light (intensity and day length) pineal gland
The Midbrain
Cerebral Aqueduct
Runs through midbrain from 3 rd to 4 th ventricle
Cerebral Peduncles
Stalks
Contain motor fibers coming from the motor cortex (corticospinal tract) cerebral aqueduct
Posterolateral View cerebral peduncle
The Midbrain
Cranial Nerves III and IV
Corpora Quadrigemina
Four dome-shaped nuclei on the dorsal midbrain
Superior colliculi
Visual reflex centers
Coordinate head and eye movements
Inferior colliculi
Act in reflexive responses to sound
Posterior View
Trochlear (IV)
Nerve
The Pons
Mostly contains tracts
Cranial nerves V, VI, and VII
Trigeminal (V)
Nerve
Abducens
(VI) Nerve middle cerebellar peduncles
Facial (VII) Nerve
View
Medulla Oblongata
Pyramids
Anterior bulges containing white matter
Carry corticospinal tracts running from motor cortex
(voluntary muscle movement)
These fibers decussate
(cross over) in the lower medulla = decussation of pyramids medulla oblongata
Anterior View pyramid
decussation of pyramid
Medulla: Decussation
Medulla Oblongata
Plays a role as an autonomic relay center
Contains several visceral motor nuclei:
Cardiovascular Center
Cardiac center- force and rate of heart contraction
Vasomotor center regulates B.P.
-changes diameter of blood vessel walls
Respiratory Centers
Control rate and depth of breathing (works with pons )
Other Centers
Regulate activities such as hiccuping, vomiting, swallowing, coughing, sneezing
Medulla Oblongata
Ascending Sensory Tract Nuclei
Nucleus cuneatus
Relay nuclei for ascending sensory information
Nucleus gracilis
Relay sensory info. from the spinal cord up to the somatosensory cortex
Olivary Nuclei
Neuron cell bodies that relay info. regarding stretch of muscles and joints to the cerebellum
Medulla Oblongata
C.N. VIII, IX, X, XI and XII
Reticular Formation
Clusters of neuron cell bodies scattered throughout the white matter of the midbrain, pons and medulla
Project to the hypothalamus, thalamus, cerebellum and spinal cord
Govern arousal of the brain by sending continuous impulses to the cerebral cortex to keep it alert (RAS)
Filters out repetitive or weak signals to dampen unnecessary input
The Cerebellum
Two hemispheres
Separated by the falx cerebelli
Vermis
Worm-like structure between the 2 hemishperes
Folia and fissures
Similar to gyri and sulci
Arbor vitae
White matter with a tree- like appearance arbor vitae folia vermis
Cerebellum
Function
Processes info. from the cerebral motor cortex, brainstem nuclei and sensory receptors
Sends output regarding timing and coordination of skeletal muscle contraction
Makes movements smooth and coordinated cerebellum
The Cerebellum
3 Cerebellar Peduncles
Connect the cerebellum to the brainstem
Superior Cerebellar Peduncle (1)
Carries axons between midbrain and cerebellum
Middle Cerebellar Peduncle (2)
Carries axons between the pons and cerebellum
2
3
1
Inferior Cerebellar Peduncle (3)
Carries axons between the medulla and cerebellum cerebellum
Diseases and Disorders
Ataxia
Staggering gait, slurred speech, overshooting of target when touching things
May result from damage to cerebellum
Cerebrovascular Accidents (Strokes)
Caused by lack of blood to the brain
Possible blockage of a cerebral artery or rupture of an aneurysm
Diseases and disorders
Transient Ischemic Attacks (TIA’s)
Temporary blood deprivation lasting from 5 to
50 min.
Temporary numbness, paralysis, or impaired speech
Usually warning of an impending, more serious stroke
Alzheimer’s Disease
Progressive degeneration of brain function
Deficit of Ach
Memory loss, shortened attention span, disorientation, possible language loss
Diseases and disorders
Parkinson’s Disease
Degeneration of dopamine releasing neurons
Basal ganglia become deprived of dopamine
Persistent tremors, forward bent posture when walking and shuffling gait
Diseases and Disorders
Huntington’s Disease
Hereditary
Massive degeneration of the basal ganglia and eventually the cerebral cortex
Causes spastic, abrupt, jerky movements
Mental deterioration and death result
The Peripheral Nervous System
CNS
PNS
Sensory Division Motor Division
Sympathetic
Division
Parasympathetic
Division
Autonomic
Nervous
System
Somatic
Nervous
System
Links the external environment and the body to the CNS
Peripheral N.S.: Components
Sensory Division
Sensory fibers carry impulses from receptors in the skin, muscles and joints ( somatic afferents )
Sensory fibers carry impulses from the visceral organs ( visceral afferents )
Motor Division
Efferent motor fibers carry impulses from the
CNS to effectors (muscles, glands and viscera)
31Pair of spinal nerves
12 Pair of cranial nerves
PNS: The Motor Division
Consists of Two Subdivisions
Somatic Nervous System
Somatic motor fibers
Conduct impulses to skeletal muscles
Allows conscious control of skeletal muscles
Autonomic Nervous System
Visceral motor fibers
Regulate smooth muscles, cardiac muscle and glands
Regulates involuntary activities
Divided into two subdivisions:
Sympathetic N.S.
Parasympathetic N.S.
Autonomic Nervous System
Nerves and receptors involved with homeostasis
Sympathetic System
Fight or flight
Parasympathetic System
Return to resting state
Sensory Receptors of the PNS
Classified by location or type of stimuli detected
Location
Exteroceptors
Interoceptors
Proprioceptors
Stimuli Detected
Mechanoreceptors
Chemoreceptors
Photoreceptors
Thermoreceptors
Nociceptors
Exteroreceptors
Near the body surface
Pick up messages from the external environment
Pick up touch, pressure, pain, temperature, special senses
Exteroreceptors
Examples:
Free Nerve Endings
In all body tissues (esp. epithelium) - pain, temp., and pressure
Merkel’s Discs
Free nerve with disc shaped endings
Found in deep epidermis
Light touch
Exteroreceptors
Examples:
Meissner’s Corpuscles
In dermal papillae of hairless skin (lips, nipples, fingertips)
Light pressure and discriminative touch
Krause’s End Bulbs
In mucosa
(mouth,conjunctiva, hairless skin near body openings)
Detect the same stimuli as
Meissner’s
Exteroreceptors
Examples
Pacinian Corpuscles
In hypodermis of skin, periostea, ligaments, joint capsules, fingers, soles of feet, external genitalia and nipples
Deep pressure and stretching
Respond only when pressure first applied
Ruffini’s Corpuscles
Found in deep dermis, hypodermis and joint capsules
Detect the same as
Pacinian’s
Interoreceptors (Visceroreceptors)
Detect stimuli originating from within the body
Pain, discomfort, stretching tissue, temperature
Examples:
Free nerve endings
Pacinian corpuscles
Propioceptors
Respond to internal stimuli
In muscles, tendons, ligaments and joints
Monitor degree of stretch
Examples: muscle spindle
Free nerve endings
Pacinian’s corpuscles
Ruffini’s corpuscles
Golgi tendon organs
Muscle spindles
Golgi tendon organ
Mechanoreceptors
Send impulses when tissues deformed by mechanical forces
Touch, pressure, vibrations, itching
Examples:
Merkel’s discs
Meissner’s corpuscles
Pacinian corpuscles
Muscle spindles and Golgi tendon organs
Chemoreceptors & Photoreceptors
Chemoreceptors
Detect dissolved chemicals
Examples:
Olfactory receptors
Taste receptors
Photoreceptors
Detect changes in light energy
Examples:
Retina of the eye
Thermoreceptors & Nociceptors
Thermoreceptors
Detect changes in temperature
Examples:
Free nerve endings
Nociceptors
Detect pain or potentially damaging stimuli
Examples:
Free nerve endings
All receptor types may function in this respect at one time or another
Pain
Pain Receptors
Pain receptors (free nerve endings) are stimulated by noxious stimuli
Damaged body tissues release chemicals bind to pain receptors
ATP released from injured cells may stimulate some pain receptors
Pain Receptor
Classification
Somatic Pain
From skin, muscles or joints
Visceral Pain
From receptors in organs in the body cavities
Results from stretching tissue, muscle spasms, or chemicals
Because visceral pain and somatic pain follow the same neural pathway, visceral pain may be perceived as somatic pain ( referred pain )
gallbladder liver liver gallbladder appendix kidneys urinary bladder
Referred Pain Areas heart lungs & diaphragm heart stomach pancreas small intestine ovaries colon ureters
optic chiasma
Trochlear nerve (IV)
Trigeminal nerve (V)
Facial nerve (VII)
Vagus nerve (X)
Hypoglossal nerve (XII)
Cranial Nerves
Olfactory nerve (I)
Optic nerve (II)
Occulomotor nerve (III)
Abducens nerve (VI)
Vestibulocochlear nerve (VIII)
Glossopharyngeal nerve (IX)
Accessory nerve (XI)
Cranial Nerves
12 pair numbered by their location (from rostral to caudal)
C.N. (I) and (II) originate from the cerebrum
C.N. (III) through (XII) originate from the brainstem
Almost all of the cranial nerves serve the head and neck
C.N. (X), Vagus, extends down into the abdominal cavity
Cranial nerves can have sensory, motor or parasympathetic neuron fibers (or all of these)
C.N. (III), (VII), (IX), and (X) contain parasympathetic fibers
Old Opie Occasionally Tries Trigonometry And Feels
Very Gloomy, Vague, And Hypoactive
C.N. I: Olfactory Nerves
Sensory only
Carry sensations of smell from nasal cavity
Originate in the mucosa of the nasal cavity
Pass through the cribiform plate of the ethmoid bone to the olfactory bulb
Olfactory nerves olfactory bulb olfactory tract inferior frontal and medial temporal lobes
C.N. II: Optic Nerves
Sensory only
Originate from the retina
Optic nerves optic chiasma optic tracts lateral geniculate bodies of thalamus optic radiations visual cortex in occipital lobe
C.N. III: Occulomotor Nerves
Motor, sensory and parasympathetic fibers
Motor to 4 of the 6 extrinsic eye muscles ( inferior oblique, superior rectus, inferior rectus, medial rectus )
Parasympathetic fibers to the constrictor pupillary muscles and the ciliary muscles (constrict the pupils and thicken the lens)
Proprioceptive afferents from 4 eye muscles it innervates
C.N. IV: Trochlear Nerves
Motor and sensory
Motor to the superior oblique muscle
Proprioceptive afferents from the superior oblique
C.N. V: Trigeminal Nerves
Motor, sensory
Three branches:
Ophthalmic Branch V
1
Sensory from upper eyelid, eye surface, tear glands, nose, scalp and forehead
C.N. V: Trigeminal Nerves
Maxillary Branch V
2
Sensory from upper teeth, gum and lip, palate and skin of cheek and lower eyelid
C.N. V: Trigeminal Nerves
Mandibular Branch V
3
Motor to muscles of mastication
Sensory from lower teeth, gum, lip, skin of jaw and part of scalp
C.N. VI: Abducens Nerves
Motor and sensory
Motor to lateral rectus muscles
Proprioceptive afferents from the lateral rectus
C.N. VII: Facial Nerves
Motor, sensory and parasympathetic fibers
Motor to muscles of facial expression
Taste from anterior 2 /
3 of tongue
Parasympathetic innervation of salivary glands
(submandibular and sublingual)
C.N. VIII: Vestibulocochlear Nerves
Sensory only
Two branches
Cochlear Branch
Afferent fibers from cochlea in inner ear carrying auditory messages
Vestibular Branch
Afferents from vestibule and semicircular canals carrying info. on equilibrium
C.N. IX: Glossopharyngeal Nerves
Motor, sensory and parasympathetic fibers
Motor to muscles of the pharynx for swallowing
Taste from posterior 1 /
3 of tongue
Sensory from tongue, tonsils, eustachian tubes
Sensory from carotid arteries regarding blood pressure and chemistry
Parasympathetic innervation of the Parotid salivary glands
C.N. X: Vagus Nerve
Motor, sensory and parasympathetic fibers
Motor to muscles of pharynx and larynx
Sensory from posterior tongue and pharynx, thoracic and abdominal viscera
Parasympathetic innervation of heart, lungs, smooth muscles of pharynx, larynx, thoracic and abdominal viscera
C.N. XI: Spinal Accessory Nerves
Motor and sensory
Motor to the muscles of the shoulder, neck
(sternocleidomastoid, trapezius) pharynx, larynx
Proprioceptive afferents from the same muscles
C.N. XII: Hypoglossal nerves
Mostly motor, some sensory
Motor to intrinsic and extrinsic tongue muscles
(move the tongue)
Proprioceptive afferents back from the same muscles
Spinal Nerves
31 pair of mixed nerves arising from the spinal cord
Transmit sensory info. to the cord ( afferents )
Transmit motor info. from the
CNS to the body ( efferents )
Numbered according to where they leave the spinal cord
C
1 exits between the occipital bone and the atlas
C
2 through C
7 exit through intervertebral foramina above which they are named (C
8 above T
1
) is
All of the rest exit below the vertebrae they are named after
There is only one small pair of coccygeal nerves (Co)
Spinal Nerve Composition
Dorsal Root
Dorsal root ganglion
Ventral Root dorsal root dorsal root ganglion ventral root
Spinal Nerve Divisions
Dorsal Ramus
Ventral Ramus
Meningeal Branches
Rami Communicantes dorsal ramus rami communicantes ventral ramus
The Cervical Plexus
The Brachial Plexus
Branches of the Brachial Plexus
Brachial Plexus Nerves
Musculocutaneous
From lateral cord
Median
From lateral and medial cords
Ulnar
From medial cord
Radial
From posterior cord
Axillary
From posterior cord
LATERAL
CORD
The Lumbar Plexus
The Sacral Plexus
Lumbosacral Nerves
Femoral
Obturator
Sciatic
Tibial
Common peroneal
Superficial branch
Deep branch
Nerve Damage
Sciatica
Pain radiating down the posterior and lower leg along the branches of the sciatic nerve
Usually the result of compression of the nerve root from a herniated disc
Brachial Plexus Injuries
Brachial Plexus Injuries
Cause weakness or paralysis to the upper limb
Median nerve damage
Loss of pincer grasp and flexion of wrist and fingers (lateral 3 1 /
2
)
Ulnar nerve damage
Results in clawhand (medial two fingers become hyperextended)
Radial nerve damage
Results in wrist drop (inability to extend the hand at the wrist and extend fingers)
THE AUTONOMIC NERVOUS SYSTEM
Innervates smooth muscle, cardiac muscle and glands
Helps to maintain homeostasis
Also called the involuntary or visceral motor system
THE AUTONOMIC NERVOUS SYSTEM
Regulation
By brainstem, spinal cord, hypothalamus and parts of the cerebrum
AUTONOMIC GANGLIA AND CIRCUITS
The motor units of the ANS consist of two neurons:
Preganglionic Neuron
Cell body is in the CNS
Synapses with another neuron before reaching the effector
The synapse occurs in an autonomic ganglion outside the CNS
(The somatic motor unit consists of one neuron with its cell body in the CNS and its axon extending to the effector)
Postganglionic Neuron
Extends from the autonomic ganglion in the PNS to the effector
AUTONOMIC GANGLIA AND CIRCIUTS
CNS PNS Effector
THE AUTONOMIC NERVOUS SYSTEM
DIVISIONS OF THE ANS:
The Sympathetic System (see table 14.4)
Fight or flight system activated in emergency situations
Effects:
Increases heart rate
Dilates bronchial tubes and pupils
Constricts blood vessels
Stimulates secretion of epinephrine and norepinephrine from the adrenal gland
Stimulates sweat glands
Inhibits digestion
Aids in ejaculation in males
THE SYMPATHETIC SYSTEM
Neurons
Emerge through the ventral roots of spinal nerves T
1 through L
(thoracolumabar outflow)
2
THE SYMPATHETIC SYSTEM
Preganglionic
Sympathetic Neurons
Preganglionic bodies are in the lateral horns of the spinal cord at the T
1 through L
2 levels
Preganglionic sympathetic axons are short
Preganglionic fibers pass through the ventral root into the white rami communicantes
THE SYMPATHETIC SYSTEM
Preganglionic
Sympathetic Neurons
Preganglionic sympathetic neurons synapse with a postganglionic neuron in the paravertebral chain ganglia
Paravertebral chain ganglia run lateral to the spinal cord on both sides
There are 22 to 23 pair of paravertebral ganglia on both sides of the vertebral column
THE SYMPATHETIC SYSTEM
Preganglionic
Sympathetic Neurons
Preganglionic fibers may ascend or descend within the chain to synapse within a ganglion at a different level
Some sympathetic preganglionic fibers pass through the chain ganglion without synapsing
These are called sympathetic splanchnic nerves
THE SYMPATHETIC SYSTEM
Preganglionic
Sympathetic Neurons
Sympathetic splanchnic nerves synapse in ganglia anterior to the vertebral column (near the aorta)
These ganglia are called prevertebral or collateral ganglia
Sympathetic splanchnics innervate smooth muscles of the abdominal and pelvic viscera and their blood vessels
THE SYMPATHETIC SYSTEM
Postganglionic
Sympathetic Neurons
Post ganglionic sympathetic axons are long
Post ganglionic sympathetic neurons exit the paravertebral ganglia via the gray rami communicantes
(unmyelinated) and reenter the spinal nerve
From here they continue on to the effector (viscera, blood vessels, sweat glands)
THE SYMPATHETIC SYSTEM
All sympathetic preganglionic neurons release acetylcholine as a neurotransmitter ( cholinergic )
Sympathetic postganglionic neurons release norepinephrine ( adrenergic ) with the exception of neurons to blood vessels and sweat glands
( cholinergic )
THE SYMPATHETIC SYSTEM
Adrenal Medulla
Preganglionic sympathetic neurons innervate the adrenal medulla
Cause release of epinephrine and norepinephrine into the bloodstream
Has the same effect as the sympathetic system only lasts 5 to 10 times longer
THE SYMPATHETIC SYSTEM
Norepinephrine & Epinephrine
Norepinephrine and epinephrine both have similar effects on the body
Epinephrine has a greater effect on cardiac stimulation, raising B.P. and increasing metabolic rate
Both are secreted by the adrenal medulla in response to sympathetic stimulation
Same effect as stimulating organs via sympathetic nerves only lasts 5 to 10 times longer
THE PARASYMPATHETIC SYSTEM
Effects:
Constricts the pupils and bronchi
Restores gland and digestive system activity
Slows heartrate
THE PARASYMPATHETIC SYSTEM
Neurons:
Emerge with the cranial nerves (III, VII,
IX and X)
Some emerge with the sacral spinal nerves
Craniosacral outflow
Neuron cell bodies for the fibers traveling with cranial nerves are in the brainstem
Cell bodies for the fibers traveling with the sacral spinal nerves are in the lateral gray horns of spinal levels S
2
-S
4
C.N. III
C.N. VII
C.N. IX
C.N. X
THE PARASYMPATHETIC SYSTEM
Preganglionic
Parasympathetic Neurons
Preganglionic neurons are long
Preganglionic neurons travel from the CNS almost all the way to the effector before synapsing with a postganglionic neuron
THE PARASYMPATHETIC SYSTEM
Postganglionic
Parasympathetic Neurons
Postganglionic parasympathetic neurons are short
Postganglionic neurons synapse with preganglionics on or near the effector organ in terminal ganglia
(collectively called intramural ganglia )
Postganglionic neurons travel from the terminal ganglia to the effector cells
THE PARASYMPATHETIC SYSTEM
Cranial Outflow
With C.N. III, VII, IX and X
Preganglionic fibers travel with each cranial nerve
Postganglionic fibers for
C.N. III, VII and IX travel with C.N. X for distribution to the face
Vagus nerve accounts for 90% of all preganglionic parasympathetic fibers in the body
Parasympathetic fibers from the Vagus nerve supply almost every thoracic and abdominal organ
C.N. III
C.N. VII
C.N. IX
C.N. X
THE PARASYMPATHETIC SYSTEM
Sacral Outflow
Axons run from the spinal cord with the ventral rami of
S
2
-S
4
Fibers branch into pelvic splanchnic nerves
Most fibers go on to synapse in intramural ganglia near the effector organ
Pelvic splanchnics innervate the distal large intestine, urinary bladder, ureters and reproductive organs
ANS RECEPTORS
Cholinergic Receptors
Activated by acetylcholine (Ach)
Two types:
Muscarinic
– Found on all effector cells stimulated by postganglionic cholinergic fibers (all parasympathetic target organs and some sympathetic)
Nicotinic
– Found on motor end plates of skeletal muscle
– Found on all postganglionic neurons (sympathetic and parasympathetic)
– Found on the hormone producing cells of the adrenal medulla
ANS RECEPTORS
ANS RECEPTORS
Adrenergic Receptors
Activated by epinephrine and norepinephrine
Two types:
Alpha (
)
– Epinephrine has a greater effect on these than norepinephrine
– Found on all sympathetic target organs except the heart
– Usually stimulatory when NE or Epinephrine binds to them
Beta (
)
– Found in the heart, adipose tissue and most sympathetic organs
– Usually inhibitory when either hormone binds to them
(except in the heart)
– Cause dilation of blood vessels
ANS RECEPTORS
VISCERAL REFLEXES
Visceral Reflex Arcs