Schizophrenia Lecture
advertisement
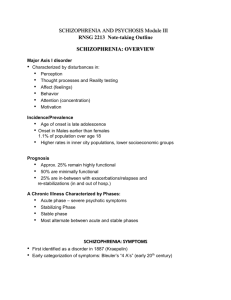
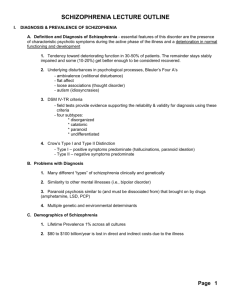
Chapter 12 • Psychosis: a loss of contact with reality • A change in your ability to perceive and respond to the environment • Can be substance-induced – but most due to schizophrenia. 2 • • • • Prevalence: 1% (about 2.5 million Americans) Little variability in prevalence cross-culturally Equal rates across men and women More frequently found among low SES • “downward drift” theory • At greater risk for suicide and to be victims of crime 3 • The DSM-5 calls for a diagnosis of schizophrenia only after symptoms of psychosis continue for six months or more • Individuals must also show a deterioration in their work, social relations, and ability to care for themselves 4 • There are three kinds of symptoms of schizophrenia: • Positive symptoms – “Pathological Excesses” • (e.g., hallucinations) • Negative symptoms • (e.g., flat affect) • Psychomotor symptoms • (e.g., catatonic postures) 5 • Positive symptoms include: • Hallucinations – false perceptions • Most common are auditory • Can involve ANY of the 5 senses – olfactory, tactile, visual • Delusions – faulty interpretations or beliefs • Lots of kinds of delusions https://www.youtube.com/watch?v=G vF4-C1EuJU 6 • Types of delusions • Persecutory • Referential • Somatic • Religious • Grandiose • Thought withdrawal • Thought insertion 7 • Disorganized Thinking and Speech: • Loose associations (derailment): • “Kyra serves drinks at a bar. I love candy bars. I went to Hershey, PA when I was five years old.” • Neologisms (made-up words): • “butterflower” • Perseveration • Patients repeat their words and statements again and again • “Let’s go to supper at the supper club, with the supper, supper” • Clang (rhymes): • How are you? “Well, hell, it’s well to tell” 8 • Other positive symptoms include: • Heightened perceptions • People may feel that their senses are being flooded by sights and sounds, making it impossible to attend to anything important • Inappropriate affect – emotions that are unsuited to the situation https://www.youtube.com/watch?v=n 7BEOxj81fM 9 • Poverty of speech (alogia) • Flat affect or blunted affect poor eye contact monotonous voice face appears to lack emotion • Loss of volition (avolition or apathy) lack of initiation or follow through • Social withdrawal 10 • Catatonic stupor – stop responding to environment, motionless and mute • Catatonic rigidity – rigid posture, resisting movement • Catatonic posturing – awkward positions • Catatonic excitement – “wild waving of arms &legs” 11 • Type I and Type II schizophrenia • Type I schizophrenia is dominated by positive symptoms • Better adjustment prior to the disorder • Later onset of symptoms • Greater likelihood of improvement • Tied more closely to biochemical abnormalities in the brain • Type II schizophrenia is dominated by negative symptoms • Tied largely to structural abnormalities in the brain 12 • Lots of proposed explanations for schizophrenia • Biological explanations have received the most research support • Biological theories: • • • • Genetic Biochemical Abnormalities Abnormal Brain Structure Viral problems • Diathesis-stress relationship • People have a biological risk for schizophrenia (diathesis) • Might only develop symptoms if they experience certain kinds of stress 13 • There is a big genetic risk in schizophrenia • The closer you are related to a person with the disorder, the more likely you are to get it. • 1% risk with no family hx • 17% risk for dizygotic twins • 48% risk for monozygotic twins • (Not 100%! Stress plays a role.) 14 • Genetic factors • Genetic factors may lead to the development of schizophrenia through two kinds of (potentially inherited) biological abnormalities: • Biochemical abnormalities • Abnormal brain structure 15 • The Dopamine Hypothesis • Certain neurons using dopamine fire too often, producing symptoms of schizophrenia • This theory was discovered accidentally • Antipsychotic drugs (which increase dopamine) were tested as allergy pills • They failed in that role – but they were found to increase dopamine 16 • Antipsychotics/neuroleptics are dopamine antagonists: bind to dopamine receptors (D2), thus preventing dopamine from binding, and preventing neurons from firing. • Extrapyramidal side effects: muscular tremors, uncontrollable shaking, similar to symptoms of Parkinson’s 17 • Biochemical abnormalities • Research since the 1960s has supported and clarified this hypothesis • Example: patients with Parkinson’s disease develop schizophrenic symptoms if they take too much L-dopa, a medication that raises dopamine levels • Example: people who take high doses of amphetamines, which increase dopamine activity in the brain, may develop amphetamine psychosis – a syndrome similar to schizophrenia 18 Antipsychotics work . . . . . . but have serious and disabling side effects • Used to be given antipsychotics like thorazine. • Now, new atypical antipsychotics • Clozapine, risperidone, olanzapine… • More effective (85% vs. 65%) • Few extrapyramidal effects • No tardive dyskinesia effects. • But, 1% risk of agranulocytosis (drop in white blood cells) -- need frequent blood tests • Abnormal brain structures have been found: • Enlarged ventricles • Smaller temporal/frontal lobes • Smaller amounts of grey matter 22 • Correlational research: • More people who were born in the winter have schizophrenia • Possible increased exposure to viruses? • More direct research: • Mothers of those with schizophrenia more likely to have had the flu • Antibodies for certain viruses more commonly found in those with schizophrenia. 23 • Research on biology of this disorder is strong, many abandoned psychological views • Two main psychological theories of schizophrenia: • Psychodynamic • Cognitive 24 • The psychodynamic explanation • Freud believed that schizophrenia develops from two processes: • Regression to a pre-ego stage (due to cold, un-nurturing parents) • Efforts to re-establish ego control • Frieda Fromm-Reichmann theorized the schizophrenogenic mothers theory • Proposed that mothers of people with schizophrenia were cold, domineering, and uninterested in their children’s needs • These theories are not supported by research. 25 • The cognitive view • Cognitive theorists agree that biological factors produce symptoms • They argue: some symptoms develop because of faulty interpretation • Example: a man experiences auditory hallucinations and approaches his friends for help; they deny the reality of his sensations; he concludes that they are trying to hide the truth from him; he begins to reject all feedback and starts feeling persecuted • There is little direct research support for this view 26 • 3 main sociocultural influences • Multicultural factors • Prevalence higher in some minority groups – is it because of SES? • Social labeling • Rosenhan’s “pseudo-patient” study • Family dysfunction • Parents higher in “expressed emotion” – more critical, overly involved • Higher “expressed emotion” – 4x greater chance of relapse! 27 • For much of human history, people with schizophrenia were considered beyond help and without hope • Though schizophrenia is still hard to treat, the discovery of antipsychotic drugs has enabled people with the disorder to think clearly and profit from psychotherapies • A historical perspective of treatment allows the best understanding of the nature, problems, and promise of modern approaches • For more than half of the 20th century, people with schizophrenia were considered insane and were institutionalized in public mental hospitals • Because patients failed to respond to traditional therapies, the primary goals of the hospitals were to restrain them and give them food, shelter, and clothing • In the 1950s, clinicians developed two institutional approaches that brought some hope to chronic patients: • Milieu therapy • Based on humanistic principles • Token economies • Based on behavioral principles • These approaches particularly helped improve the personal care and self-image of patients, problem areas that were worsened by institutionalization • Milieu therapy • The guiding principle is that institutions can help patients make clinical progress by creating a social climate (“milieu”) that promotes productive activity, self-respect, and individual responsibility • Milieu programs have been set up in institutions throughout the Western world with moderate success • Research has shown that patients with schizophrenia in milieu programs often leave the hospital at higher rates than patients receiving custodial care • The token economy • Based on operant conditioning principles, token economies are used in institutions to change the behavior of patients with schizophrenia • Patients are rewarded when they behave in socially acceptable ways and are not rewarded when they behave unacceptably • Immediate rewards are tokens that can later be exchanged for food, cigarettes, privileges, and other desirable objects • Acceptable behaviors likely to be targeted include care for oneself and one’s possessions, going to a work program, and showing self-control • The token economy • Researchers have found that token economies help change psychotic and related behavior • However, questions have been raised about such programs: • Are such programs ethical and legal? Aren’t all humans entitled to basic rights, some of which are compromised in a strict token economy system? • Are such programs truly effective? For example, patients may change overt behaviors but not underlying psychotic beliefs • While milieu therapy and token economies helped improve treatment outcomes, it was the discovery of antipsychotic drugs in the 1950s that revolutionized treatment for those with schizophrenia • It was discovered that one group of antihistamines, phenothiazines, could be used to calm patients about to undergo surgery • Psychiatrists tested one of the drugs, chlorpromazine, on six patients with psychosis and observed a sharp reduction in their symptoms • Antipsychotic drugs developed throughout the 1960s, 1970s, and 1980s are now referred to as “conventional” antipsychotic drugs • Drugs developed in recent years are known as “atypical” antipsychotics • Research has repeatedly shown that antipsychotic drugs reduce schizophrenia symptoms in the majority of patients • In direct comparisons, drugs appear to be more effective than any other approach used alone • In most cases, the drugs produce the maximum level of improvement within the first six months of treatment • Symptoms may return if patients stop taking the drugs too soon • Antipsychotic drugs, particularly the conventional ones, reduce the positive symptoms of schizophrenia more completely, or at least more quickly, than the negative symptoms • Although the use of such drugs is now widely accepted, patients often dislike the powerful effects of the drugs, and some refuse to take them • The most common unwanted effects produce Parkinsonian symptoms, reactions that closely resemble the features of the neurological disorder Parkinson’s disease, including: • Muscle tremor and rigidity • Dystonia (bizarre movements of the face, neck, tongue, and back) • Akathisia (great restlessness, agitation, and discomfort in the limbs) • A more difficult side effect of conventional antipsychotic drugs appears up to one year after starting the medication • This reaction, called tardive dyskinesia, involves involuntary movements, usually of the mouth, lips, tongue, legs, or body • It affects more than 10% of those taking the drugs • It can be IRREVERSIBLE! • Since learning of the unwanted side effects of conventional antipsychotic drugs, clinicians have become more careful in their prescription practices: • They try to prescribe the lowest effective dose • They gradually reduce or stop medication weeks or months after the patient begins functioning normally • Recently, new drugs have been developed • Called “atypical” because their biological operation differs from that of conventional antipsychotics • They appear more effective than conventional drugs, especially for negative symptoms • They cause few extrapyramidal side effects (i.e., movement disorders) • Examples: Clozaril, Risperdal, Zyprexa, Seroquel, Geodon, and Abilify • Before the discovery of antipsychotic drugs, psychotherapy was not an option for people with schizophrenia • Most were simply too far removed from reality to profit from psychotherapy • Today, psychotherapy can be very helpful when used in combination with medication • The most helpful forms of psychotherapy include insight therapy and two broader sociocultural therapies: family therapy and social therapy • These approaches are often combined • Insight therapy • A variety of insight therapies have been used to treat schizophrenia • Studies suggest that the orientation of the therapist is less important than their experience with schizophrenia • In addition, the most successful therapists are those who take an active role, set limits, express opinions, and challenge the patients’ statements • Family therapy • About 25% of persons recovering from schizophrenia live with family members • This creates significant family stress • Those who live with relatives who display high levels of expressed emotion are at greater risk for relapse than those who live with more positive or supportive families • Family therapy attempts to address such issues, create more realistic expectations, and provide psychoeducation about the disorder • The community approach is the broadest approach for the treatment of schizophrenia • In 1963, Congress passed the Community Mental Health Act, which said that patients should be able to receive care within their own communities, rather than being transported to institutions far from home • This led to massive deinstitutionalization of patients with schizophrenia • Unfortunately, community care was (and is) inadequate for their care • The result is a “revolving door” syndrome • People recovering from schizophrenia and other severe disorders need medication, psychotherapy, help in handling daily pressures and responsibilities, guidance in making decisions, training in social skills, residential supervision, and vocational counseling • This combination of services sometimes is called assertive community treatment • There is no doubt that effective community programs can help people with schizophrenia recover • However, fewer than half of all people who need them receive appropriate community mental health services • In any given year, 40% to 60% of all people with schizophrenia receive no treatment at all • Two factors are primarily responsible: • Poor coordination of services • Shortage of services • When community treatment fails, many people with schizophrenia receive no treatment at all • Some return to their families and receive medication and perhaps emotional and financial support, but little else in the way of treatment • Finally, a great number of people with schizophrenia become homeless • Approximately one-third of the homeless people in America have a severe mental disorder, commonly schizophrenia • Today community care is a major feature of treatment for people recovering from schizophrenia in countries around the world • Both in the U.S. and abroad, varied and well-coordinated community treatment is seen as an important part of the solution to the problem of schizophrenia