Evidence-based Medicine - Computing in the Humanities and Social

Ethics and
Evidence-based Medicine (EBM)
PHL281Y Bioethics
Summer 2005
University of Toronto www.chass.utoronto.ca/~kirstin
Overview
1.
(Olivieri case)
2.
Decision-making in Medicine
3.
What is EBM?
4.
Evaluating the Evidence
Hierarchy
5.
Ethics and EBM
6.
Ethics and Corporate Influences on Decision-making in Medicine
Interim findings of RCTs
Case: Dr. Nancy Olivieri
Mid 1990’s
Hospital for Sick Children (Toronto)
Apotex
Thalassemia
Hydroxypyridin-4-1 (deferiprone)
Physician/scientist roles (Hellman &
Hellman)
Individual equipoise vs. clinical equipoise
Academic freedom in clinical research
Decision-making in Medicine
How do physicians make decisions about treatments for particular patients?
• Intuition? Experience? Authority? Case studies?
RCT evidence?
Is it ethical of a physician to make decisions on other grounds? Why/Why not?
• Decision based on ‘gut feeling’?
It matters quite a lot whether these decisions are right or wrong (life/death)
EBM Version 1.0
Evidence-based Medicine (EBM)
Motivation
• History: textbook information + authority of superiors + personal experience as sources of evidence
• Surveys in the 70’s and 80’s - lack of standardization
• Increase in biomedical research - overload of information (read 19 articles/day, 365 days/year vs. 1 hour a day to read)
Goal: Make the practice of medicine more objective
(and hopefully therefore more standardized)
The (In)famous Declaration (1.0)
EBM “de-emphasizes intuition, unsystematic clinical experience and pathophysiologic rationale as sufficient grounds for clinical decision-making and stresses the examination of evidence from clinical research”
EBM Working Group 1992 JAMA
The Process (1.0)
1.
Formulate a question
2.
Do a literature search (MEDLINE)
3.
Use the evidence hierarchy to ‘critically evaluate’ the quality of evidence
4.
Apply the recommendations of the ‘best evidence’ directly to patients
*Don’t let intuition or clinical experience interfere
The Reaction to EBM 1.0
Medical journals flooded with articles, editorials
Concern about a ‘cook-book’ approach to medicine (no deviation)
The art vs. science of medicine
EBM Version 2.0
“Evidence-based Medicine is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients”
- Sackett, JAMA 1996
Integration model – best evidence + individual clinical expertise (‘neither alone is enough’)
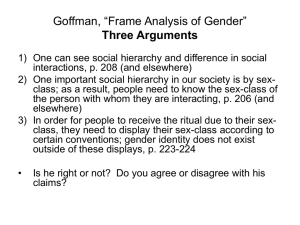
Comparing Versions 1 & 2
EBM 1 “de-emphasizes intuition, unsystematic clinical experience and pathophysiologic rationale as sufficient grounds for clinical decision-making and stresses the examination of evidence from clinical research”
(1992)
EBM 2 “is the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients” (1996)
The Process (2.0)
1.
Formulate a question
2.
Do a literature search (MEDLINE)
3.
Use the evidence hierarchy to ‘critically evaluate’ the quality of evidence
4.
Integrate ‘best evidence’ with clinical experience to produce a decision regarding treatment
Simplified Evidence Hierarchy
Meta-analyses
Randomized Controlled Trials
Non-randomized / Observational Research
Case-series, Case Studies, Qualitative Research, Anecdotal Evidence
Assumptions Underlying the Hierarchy
Why is the hierarchy ordered the way it is?
Best evidence is identified by 3 characteristics:
1. Simple
• The simplest explanation is often the best (Ockham’s razor)
2. Generalizable
• The results of research need to be generalizable to as many patients as possible
3. Objective (free from bias)
Success
EBM now widely accepted in medical schools and hospitals across North America and much of Europe
Extended to physiotherapy, nursing, public policy, dentistry… “Evidence-based practice”
Practice Guidelines
“One of the most influential ideas of the year” New York
Times Magazine 2001
Funding bodies, journal editors and policy makers continue to rely on strict application of the evidence hierarchy (RCTs and meta-analyses of RCTs)
7 Alternatives to EBM (BMJ)
1. Eminence-based medicine - the more senior the colleague, the less importance he or she placed on the need for anything as mundane as evidence. These colleagues have a touching faith in clinical experience, which has been defined as “making the same mistakes with increasing confidence over an impressive number of years.”
2. Vehemence-based medicine - the substitution of volume for evidence.
3. Eloquence-based medicine - the year-round suntan, carnation in the buttonhole, silk tie, Armani suit, and tongue should be equally smooth. Sartorial elegance and verbal eloquence are powerful substitutes for evidence.
7 Alternatives (continued)
4. Providence-based medicine – decision left in the hands of the
Almighty
5. Diffidence-based medicine do nothing from a sense of despair. (This may still be better than doing something merely because it hurts the doctor’s pride to do nothing)
6. Nervousness-based medicine fear of litigation is a powerful stimulus. In an atmosphere of litigation phobia, the only bad test is a test you didn’t think of ordering
7. Confidence-based medicine this is restricted to surgeons
Evaluating the Hierarchy
What is actually being done (almost exclusive focus on RCTs and meta-analyses) vs. charitable reading of what is proposed
• Example: 13 observational studies found same effect, all trumped by 1 RCT that disagreed
Evaluating the Hierarchy
“Because the randomized trial, and especially the systematic review of several randomized trials, is so much more likely to inform us and so much less likely to mislead us, it has become the ‘gold standard’ for judging whether a treatment does more harm than good”
• Note: the claim that observational research ‘overestimates’ effects is circular
Do we have reason to doubt the RCT as the ‘gold standard’?
Do we have reason to value the lowest levels of evidence more highly?
Evaluating the Hierarchy
A weak claim: “An RCT is not always the best choice of study design”
A stronger claim: “An RCT, even when possible, often gives markedly worse evidence than an observational study”
(Grossman & Mackenzie, 2005)
Evaluating the Hierarchy
1. Treating the ‘Average’ Patient (vs. individualized care)
• The RCT evaluates efficacy rather than effectiveness
• Restricted population in trials (inclusion and exclusion criteria)
• “Only 10% of patients in primary care have the sort of isolated, uncomplicated form of hypertension that lends itself to management by a standard evidence-based guideline.”
(Greenhalgh, 1999)
• “Clinical research, as currently envisioned, must inevitably ignore what may be important, yet non-quantifiable, differences between individuals. Defining medical knowledge solely on the basis of such studies, then, would necessarily eliminate the importance of individual variation from the practice of medicine” (Tonelli, 1998)
Evaluating the Hierarchy
• “The empirical observation of populations in randomized trials and cohort studies cannot be mechanistically applied to individual patients (whose behavior is irremediably contextual and idiosyncratic) or episodes of illness.” (Greenhalgh, 1999)
• “When transferred to clinical medicine from an origin in agricultural research, randomized trials were not intended to answer questions about the treatment of individual patients”
(Feinstein and Horwitz, 1997)
• Complexity of human beings
Adverse Drug Reactions (rate 4-6 th leading cause of death
in USA)
Support from pharmacogenetics
• RCT results may be most helpful at policy level
• Need subgroup analysis (at the very least)
Evaluating the Hierarchy
2. False Sense of Objectivity
Some possible sources of bias in research:
Broad social forces
Funding agencies
Publication bias
• Suppressing negative results, confidentiality clauses, presenting only part of the data (ex/ Celebrex – first 6 months of year-long trial, AIDS vaccine – only presented positive subgroup)
Loopholes in methodology
• Study design bias - testing against placebo rather than current drug, testing only young people (less side effects), suboptimal dosing, trials too brief to be meaningful
Backgrounds and goals of researchers (research what you fear)
Researcher’s values (ex/ interpreting data favourably)
Patient’s values
…
Evaluating the Hierarchy
3. “Lower” Evidence is Often Ignored
• Many research questions cannot be answered with RCTs - think especially of social, psychological and environmental diseases and treatments
• If you treat patients on the EBM model, what happens to information from these sources?
• How does this influence treatment?
Overmedication (nutrition and exercise vs. drug)?
Evaluating the Hierarchy
4. The Problem of Moving Away from First Causes
• RCTs and symptom alleviation
• “Identify and treat the causes”
• You will need research in basic sciences (biochemistry, etc.) to get at these first causes
• Pathophysiology
Antibiotics for infection, pacemakers, blood transfusions, fluids for dehydration…
Insulin and penicillin!
5. Lack of Significant Commitment to Shared Decision-making
• Even EBM version 2.0 downplays the patient’s role in evidence-based decision-making with strict adherence to the evidence hierarchy
• If patient’s role is significant, ‘best evidence’ may vary
Evaluating the Hierarchy
6. Social, Political and Economic Forces Shifting Direction of Research
• RCTs are expensive and require much infrastructural support
(gold)
• Lack of interest in investing/researching un-patentable treatments (market demands)
• Orphan drugs vs. ‘me-too’ drugs
• Some treatments may not be researched because they cannot be patented and the payoff isn’t high enough – yet they could be effective treatments
• This skews the direction/content of ‘good evidence’
Evaluating the Hierarchy
7.
New Forms of Authority
8.
• The Cochrane Collaboration (based in Oxford) – international consortium of workers who construct, rank, and maintain an ever-enlarging data base of clinical trials (based on the evidence hierarchy of EBM)
• Industrial-scale production of meta-analyses?
Potential Abuses
• Cookbook (as much as it is denied)
• Management by policy-makers and hospitals:
“These so-called ‘best practices’ are poised to become coercive mandates imposed by government agencies and third-party payers with political and financial incentives to ration health care
– and the power to do it…The public should be alarmed.” (Brase
2005)
Managed care and EBM
• Malpractice suits?
EBM Assessment
If physicians uncritically accept the EBM hierarchy, they may make decisions about patient-care on inappropriate evidence. Is this acceptable? Is this any different from what existed before EBM?
Does the presence of EBM create new moral obligations for physicians?
How do physicians maintain commitment to the ‘central aim of medicine’ in light of these developments?
Persistent uncertainty in medicine
Ethics and Uncertainty
Uncertainty is unavoidable (though it may be reduced through research)
1.
How should one make a decision under uncertainty when an error might harm someone?
• Moral demand for reasons (vs. hunches, intuitions)
2.
How should clinicians communicate this uncertainty and risk to patients?
• Disclosure of relevant uncertainty
• Share this management of uncertainty with patients in shared decision-making
Ethics and Uncertainty
3.
How ought society respond to the problem of scientific or clinical uncertainty, as well as to the tensions raised as money and malpractice challenge efforts to incorporate more evidence into daily practice?
• Reward quality, not compliance (many cases rather than individual cases)
• Fix malpractice liability problem (‘catastrophe’ in USA) – don’t assume certainty of practice guidelines in law
• Do more, better science (no hidden research) and improve education (medical students should be taught the probabilistic and uncertain nature of medicine and the ethical challenges this raises)
-Goodman (2005)
Influences on Decision-making
Corporate Influence (Global
Industry - $400 billion/year):
• Marketing as research
(examples earlier)
“I became increasingly troubled by the possibility that much published research is seriously flawed, leading doctors to believe new drugs are generally more effective and safe than they actually are.” (Angell,
2004)
Influences on Decision-making
• Marketing as education: retreats, conferences, seminars, lunches, information packages
‘Thought leaders’ and ‘consultants’
‘Detailing’ 88,000 sales representatives of pharmaceutical companies employed to promote products in hospitals and doctors offices (USA)
‘Preceptorship’ – shadowing doctors as they see patients
Marketing off-label use of drugs
Educating patients – DTC advertising
• Should we try to draw a line between education and marketing (education grants vs. kickbacks) and use restrictions?
• Angell – it really is all marketing.
Pharmaceutical companies are not in the education business
Influences on Decision-making
• ‘Free’ samples ($11 billion/year in
USA)
• Gifts – books, golf balls, tickets to sporting events, Christmas trees, champagne, family vacations to
Hawaii
Some new regulations on this recently
• Financial incentives for recruiting patients into studies
Moral assessment?
Central aim of medicine?
Summary
4.
5.
6.
1.
2.
3.
(Olivieri case)
Decision-making in Medicine
What is EBM?
Evaluating the Evidence Hierarchy
Ethics and EBM
Ethics and Corporate Influences on Decision-making in Medicine
Looking Ahead
Next class – last full lecture
Justice and Health Care
Contact
Prof. Kirstin Borgerson
Room 359S Munk Centre
Office Hours: Tuesday 3-5pm and by appointment
Course Website: www.chass.utoronto.ca/~kirstin
Email: kirstin@chass.utoronto.ca