Pneumonia Pneumonia
advertisement

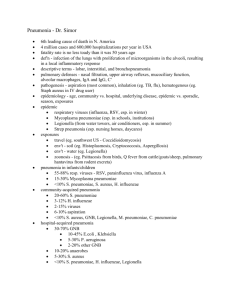
Pneumonia Prof. Dr. Bilun Gemicioğlu Definition Pneumonia is a lung parenchyma infection caused by bacteria, a virus or fungi, with a consolidation on radiological examination. Pneumonitis is an inflammation of the lungs caused by chemical or radiation therapy but not with infectious agents. Spread of lung infections – Inhalation – Aspiration of oropharingeal secretion – Hematogenic spread – Direct spread (thorax wall, mediastinum) Predisposing factors of pneumonia • Airways mechanical barrier damage • Specific and/or nonspecific immune defense mechanisms injury • Bronchial obstruction • Micro aspiration of upper respiratory truck secretion. • Lung edema • Viral infections. Diagnostic Methods • History, physical examination • Chest X-Ray • Sputum examination (gram stained) • Sputum , blood cultures • Serological tests • Peripheral blood analysis Diagnosis Symptoms fever, shaking chills, cough, sputum (expectoration), pleuritic pain. Others: (dispnea, fatigue, sweating, loss of appetite...) Physical signs: increased vibration thoracic impaired percussion (matity), end inspiratory rales (crepitations) and bronchial breathing (tuber soufle) Others (cyanosis, tachipnea, tachicardia...) Diagnosis Radiology: lobar opacities, interstitial images, bronchopneumonic (patchy) opacities, Others (absea, pneumatocele, pleurisy...) Chest X-Ray • Gold standart test for pneumonia • For differencial diagnosis • For grading pneumonia severity • For examining complications Normal Chest X Ray in Pneumonia -First 24 hours -Dehydration -Elderly -Neutropenia -Pneumocystis carinii Classification with anatomical localization • Lobar consolidation • Bronchopneumonia • Interstitial pneumonia Classification with ethiology •Bacterial •Viral •Fungal •Parazites Classification with targeting therapy • Community acquired pneumonia • Hospital acquired pneumonia (Nosocomial) • Immunosuppresed (immunocompromised) patients pneumonia Community acquired pneumonia Pneumonia acquired outside hospital frequently in healthy persons Caracteristics of community acquired pneumonia (CAP) Typical pneumonia acute fever,chills productive cough pleural pain physical signs ( + ) lobar consolidation Agents S. pneumoniae H. Influenzae Gr(-)aerop bacillus Aneorobes Atypical pneumonia subacute, subfebril fever non productive cough nonrespiratory symptoms physical signs ( - ) non-lobar infiltration M.pneumonia C.pneumoniae L. Pneumophila Virus Lobar pneumonia Lobar pneumonia Bronchopneumonia Interstitial pneumonia CAP THERAPY GROUP 1 GROUP 2 GROUP 3 OUTPATIENTCLINIC HOSPITAL INTENSIVE CARE Mild pneumonia, Moderate pneumonia Severe pneumonia CAP Therapy: Group I No antibiotic usage No comorbidity With comorbidities Pneumococci resistant to penicillin Gram (–) agents Usage of antibiotic last three months Usage of corticosteroid Penicillin, Macrolide, Floroquinolone, ß laktame + Macrolide Therapy: Group 2 II CAPCAP Therapy: Group • S.pneumoniae • H.influenzae • M.pneumoniae • C.pneumoniae • Mix infection) • Enteric Gram negatives ! • Virus First choise Alternatif ________________________________________ Penicillin G ± makrolide Levofloksasin Aminopenicillin ± makrolide Moksifloksasin Aminopenicillin / β-laktamase inhibitor ± macrolide Non- antipseudomonal cefalosporin II-III ± macrolide CAP Therapy: Group III No risk of P. aeruginosa • Non pseudomonal cefalosporin III+ macrolide or • Non pseudomonal cefalosporin III + (moksifloksasin or levofloksasin) With risk of P. aeruginosa • Anti-pseudomonal cefalosporin (sefepim-seftazidim) or • Ureidopenicillin/beta-laktamase inhibitor (piperasilin.. or • Karbapenem + siprofloksasin Duration of the therapy After fever drop 1 week - Pneumococcic pneumonia 7-10 days - Legionella pneumonia - Mycoplasma ve C. pneumoniae 14-21 days 10-14 days Severe pneumonia 2-3 weeks