File
advertisement

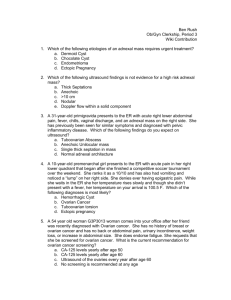
Adnexal Mass Joshua A. Craig State University of New York Polytechnic Institute Subjective History Patient Information • • • • • Patient: SP Age: 57 Clinical Site: Alice Hyde Women’s Health Student: Josh Craig, FNP- Student Date of Encounter: November 10, 2014 Chief Complaint & History of Present Illness • Chief Complaint: I am here today to follow up with Dr. O'Garro after my primary care provider found a mass in late August. • HPI: Presents today to follow up on a mass found by her PCP during a routine physical exam in late August. Onset is new since pelvic exam last year. Located on the right side during pelvic exam. Has had no associated abdominal pain or cramping. Has experienced no limitations in ADLs. Has experienced no associated vaginal bleeding or spotting. Has had no previous history of ovarian cysts or masses upon past physical or gynecological examinations. Recently positive for goiter found upon examination of thyroid during routine physical examination which is being managed by her PCP. Has no further medical complaints or medical problems at this time. Review of Systems • General: Denies change in appetite, body aches, chills, fainting, fatigue, fever, insomnia, pain, feeling weak and weight change. General health stated as good. • Skin: Denies any rashes, lesions, masses, dryness or changes in nail texture. • CV: Denies arrhythmia, CAD, CHF, chest pain, dizziness, dyspnea, irregular heartbeat, palpitations and swelling. • Resp: Denies difficulty breathing, chest heaviness, chest tightness, cough, congestion, dyspnea, hemoptysis, poor sleep quality, shortness of breath and wheezing. • Neck: Positive for goiter. Denies having any swollen glands, pain, stiffness, decreased ROM, difficulty breathing or swallowing. ROS • GI: Denies abdominal pain, abdominal cramping, abdominal swelling, change in appetite, constipation, diarrhea, flank pain, heartburn, nausea, difficulty swallowing and vomiting. • GU: Menarche at age 12. Menopause at age 50. Last pap test on performed on August 28, 2014- results normal. Reports postmenopausal, but denies bloating, postcoital bleeding, sexual dysfunction, uterine fibroids, vaginal problems, bleeding, discharge, foul smell, itching, lesion, mass, soreness and vulvar lesions. LMP was 7 years ago. Reports having genital warts in 1976 which cleared after treatment. Positive for an additional STI , unable to specify what the STI was, lesions cleared after receiving an antibiotic several years ago. Remains sexually active with her husband, neither use STI protection. Husband has had a vasectomy. Positive for urinary incontinence with sneezing and heavy lifting. Denies having urgency or dribbling. Denies having difficulty voiding, hematuria, sexual difficulites and frequent UTIs. ROS • Obstetrical: G 3 T 2 P 0 A 1 L 2 • Breast: Denies cancer, discharge, hot flashes, lumps, masses, pain, rash and tenderness. Performs self breast examinations monthly. • Psych: Denies anxiety, mood changes and sleep pattern disturbance. • Endocrine: Reports goiter but denies diabetes, high cholesterol, hot flashes, polyphagia, excessive thirst or excessive urination. Past Medical History • General Health: Last comprehensive examination September 2014 • Medical Illnesses: Hyperthyroidism, chronic rhinitis • Health Maintenance: Mammogram on October 7, 2014, Bone Density Scan in 2006, Depression Screening in October 1, 2014, Gynecologic Exam in 2014, Pap test on August 28, 2014. • Surgical Hx: Tonsillectomy as a child, year unspecified. • Hospitalizations: Childbirth in 1983 and 1986. Allergies: Positive for allergy to Penicillin, causes hives. Positive for seasonal allergies. Denies any allergies to food or latex. Medications: Allegra 180mg PO daily PMH • • • • Family Hx Father: Positive for dementia and heart disease. Mother: Negative for medical problems. Children: 1 son and 1 daughter. Son positive for HTN. Daughter has no medical history. • No personal or family history of uterine, ovarian, endometrial, breast or colorectal cancers. • Social Hx: Patient has never smoked. Drinks twice weekly, would not specify amount. Uses no illegal drugs. Drinks 2-4 cups of coffee daily. Objective History Physical Examination • Vital Signs: BP 118/84, HR 81, R 18, T 98.4 F, Spo2 98% RA, Pain Level 0/10. • General: A well-developed, well-nourished 57 year-old female who is alert, oriented and in no apparent distress. • Skin: Skin is uniformly pink in color with brisk skin turgor. No lesions or masses present. Skin remains moist. • Neck: Palpation reveals no lymphadenopathy. Thyroid exhibits goiter, but no nodules or tenderness on palpation. Trachea remains midline. • Resp: Vesicular lung sounds present bilateral lungs anteriorly and posteriorly. AP diameter 1:2. No wheezing, rhonchi, rales or crackles present. • CV: Rate is regular. Rhythm is regular. S1 & S2 intact. No S3, S4, murmurs, rubs, heaves or thrills present. Physical Examination • Abdomen: Exam was done with a chaperone present. Positive bowel sounds in all 4 quadrants. Tympany present with percussion throughout abdomen. No tenderness with light palpation. No organomegaly, splenomegaly or hepatomegaly present with deep palpation. • GU: Did not examine. • Lymph: No visible or palpable anterior or posterior cervical lymphadenopathy. No visible or palpable supraclavicular lymphadenopathy. No visible or palpable axillary lymphadenopathy. Inguinal nodes unremarkable. No adenopathy of the submandibular nodes bilaterally. • Psych: Mood/Affect: Patient's attitude is appropriate. No anxiety or depression present. Affect is bright. Assessment Diagnostics Reviewed CBC • • • • • • • Glucose 80 BUN 17 Cr 0.88 Na 140 K 4.5 Cl 105 Ca 9.1 BMP • WBC 5.0 • RBC 4.72 • Hgb 13.9 • Hct 43.0 • PLT 318 Diagnostics Reviewed • • • • TSH 0.877 (0.34-5.60) LDL Cholesterol 101 HDL Cholesterol 72 Triglycerides 78 • All lab work drawn on August 28, 2014 Diagnostics Reviewed • Transvaginal Pelvic US (October 7, 2014) • • • • Small calcification in the anterior aspect of the body of the uterus suggesting of small calcified fibroid. Left ovary is not seen Well defined hyperechoic mass could represent adnexal tumor on the right. A follow-up MRI with and without contrast is recommended. • MRI Pelvis With and Without Contrast (October 7, 2014) • • • • • No definite fibroid seen 2.7cm x 2.4cm lesion with enhancement seen. 2cm simple cyst visualized in right ovary. Uterus shows no abnormality. No free fluid seen. Diagnostics Reviewed • MRI Abdomen (October 7, 2014) • No abnormality seen. • Mammography (October 7, 2014) • Benign calcification in the upper out quadrant of the right breast. No mammographic evidence for malignancy. Differential Diagnoses • • • • • Ovarian cancer Uterine fibroid Uterine cancer Peritoneal cyst Ovarian cyst Diagnosis • 620.2 Ovarian cyst Etiology and Pathophysiology • An ovarian cyst is a fluid filled sac or pouch that forms on the ovary. They most commonly occur during the childbearing years, can develop one or more cysts, and can vary in size. They can also be harmless and benign or problematic and malignant. (American Congress of Obstetricians and Gynecologists [ACOG], 2014). • Neoplastic cysts: Arise via the inappropriate overgrowth of cells within the ovary and may be malignant or benign. The most frequent neoplastic cysts arise from the ovarian surface epithelium (mesothelium). (Helm, 2014). • Serous Cystadenomas: A form of neoplastic cysts. Arise from the ovarian epithelium. Serous cystadenomas can become very large and are prone to torsion because of their size (Schuiling & Likis, 2013, p. 693). • Endometriomas (Chocolate cysts): Blood-filled cysts which are associated with endometriosis (Helm, 2014). Causes a classic triad of painful, heavy periods and dyspareunia (Helm, 2014). More commonly occurs on the left ovary (Schuiling & Likis, 2013, p. 694). Etiology and Pathophysiology • Teratomas (Dermoid cysts): A form of germ cell tumor containing element from all 3 embryonic germ layers- the ectoderm, endoderm and mesoderm (Helm, 2014). They are filled with sebaceous material and often contain hair, bone, teeth, or other tissues from the germ layers (Schuiling & Likis, 2013, p. 693). Ovarian torsion occurs in as many as 10% of teratomas (Schuiling & Likis, 2013, p. 693). • Functional cysts: Functional cysts are the most common forms of ovarian cysts and include follicular cysts and corpus luteal cysts. Follicular cysts occur from a lack of physiologic release of the ovum due to excessive FSH stimulation or lack of the normal LH surge at midcycle just before ovulation. Hormonal stimulation causes these cysts to grow. Corpus luteal cysts occur when there is failure of dissolution of the corpus luteum after 14 weeks’ time. (Helm, 2014). Incidence • Ovarian cysts are found on transvaginal sonograms in nearly all premenopausal women and in up to 18% of post-menopausal women. • Mature cystic teratomas, or dermoids, represent more than 10% of all ovarian neoplasms. • Malignant epithelial ovarian cystadenocarcinomas are the only ovarian cysts associated with a race predilection. Women from northern and western Europe and North America are affected most frequently. • For women aged 55-69 years, the highest rates occur in white women followed by Hispanic and Japanese women. • The incidence of epithelial ovarian cystadenocarcinomas, sex cord stromal tumors, and mesenchymal tumors rises exponentially with age until the sixth decade of life at which point the incidence plateaus. • Tumors of low malignant potential occur at a mean age of 44 years. (Helm, 2014) Diagnostic Screening Recommendations • Medical Imaging • CT Scan • Best for imaging hemorrhagic cysts. More sensitive but less specific than US. • MRI • Reserved for cases in which US and CT scan results are indeterminate in identifying a mass as an ovarian cyst. • Ultrasound • Primary tool for a patient suspected to have an ovarian cyst (Helm, 2014) Diagnostic Screening Recommendations • Blood Work • Cancer antigen 125 • Indicated for women past menopause • CBC • Evaluate H&H for anemia and WBC for potential infectious causes • Urinalysis • Indicated if experiencing abdominal or pelvic pain (Helm, 2014) Treatment Recommendations • For postmenopausal women • Repeat US and Ca-125 in 4-6 weeks • Referral for surgery if simple ovarian cysts remain persistent, symptomatic and size increases to 5-10cm (Helm, 2014) Plan Plan • Diagnostics: CA 125, Abdominal US • Therapeutic: No medications or surgical interventions are required at this time. We will continue to monitor the growth of the ovarian cyst via Abdominal US follow-up in 3 months. We will also draw labs to check for cancerous markers. • Special Instructions: Call if you experience sudden onset of unilateral pelvic pain or if you notice any spotting or vaginal bleeding. • Patient Education: Discussed ovarian cancer, STI monitoring and safe sex practices, hyperthyroid management. • Follow-Up: Follow up in 4-6 weeks to review your Abdominal US results. Follow-up at the women's health clinic for any further gynecologic issues. References • American Congress of Obstetricians and Gynecologists. (2014). FAQ: Frequently asked questions gynecologic problems. Retrieved from http://www.acog.org/Patients/FAQs/Ovarian-Cysts • Helm, C. W. (2014). Ovarian cysts. Medscape. Retrieved from http://emedicine.medscape.com/article/255865-overview • Schuiling, K. D., & Likis, F. E. (2013). Women’s gynecologic health (2nd ed.). Burlington, MA: Jones & Bartlett Learning.