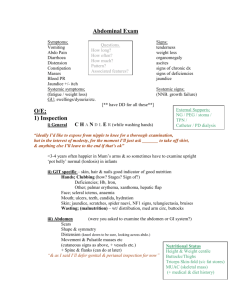
Gastro Click to
advertisement
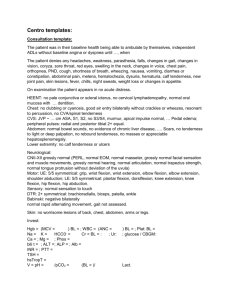
Becky Ollerenshaw - Paediatrics Society 18.04.15 Introduction To Mum/Dad and to child If parents are on your side things are easier! Explain what you're going to do General Inspection Observe Observe! Observe!!! General inspection Well or ill? Appearance Nutritional status Behaviour Cannulae, creon, inhalers, wiggly bags (cartoon bags for central lines),walking aids etc. Rapport Depends on age of child Get mum/dad involved Explain with detail appropriate to age of child Positioning On parent’s lap for wiggly/scared toddlers and small children Hands Leukonychia, Koilonychia, Clubbing – Crohn’s, UC, coeliac’s Beau’s lines – horizontal white lines – caused by any acute severe illness – grow out in 12 weeks Asterixis – realistically only in older children Hands Pulse, perfusion (cap refill on sternum) Colour, skin Single palmar crease - thyroid problems, small bowel obstruction Bruising – liver failure / vitamin K deficiency (in neonates) Face Sunken fontanelle - dehydration Yellow sclera - jaundice Pale conjunctiva - anaemia Keyser-Fleischer rings – Wilson’s disease (mean age of presentation 6-20) Face Ulceration – Crohn’s, Angular stomatitis, Glossitis Gum hypertrophy – leukaemia, anti-epileptics (phenytoin) Candida – immunodeficiency (AIDs, leukaemia) Freckling around the mouth – Putz-Jehger’s syndrome – associated with polyps in the bowel. High risk of cancer / obstruction Warm hands! And stethoscopes!!! Tummy! Can be tickley Get down to their level Get them to move before you touch- Puff out tummy = rebound tenderness Pain less localised than in adults (abdo pain can be pneumonia!) Normal to be rounded Normal to be rounded and feel up to 2 finger widths of liver and spleen in babies and toddlers. Abdomen Inspection - peristalsis, 4 Fs (not 5!), bruises, scars, etc. Pyloric stenosis – visible peristalsis Palpate as for adult in older child Check for pain and distension in babies (& toddlers if unco-operative) Hydration status (skin pinch) Percussion and auscultation technique as for adult Abdomen Listen for cornflakes!!! Don't forget!! Dipstick the urine Plot a growth chart PR not routinely done Case 1 Creon by bed, small for age, patient comfortable at rest. Old laporotomy scar No tenderness, no organomegaly Cystic Fibrosis Creon by bed – exocrine pancreatic insufficiency Small for age - malabsorption Old laporotomy scar – may be due to neonatal complicated meconium ileus No tenderness, no organomegaly Case 2 Young child of afro-caribbean ethnicity, patient comfortable at rest. No jaundice, some conjunctival pallor No scars No tenderness, splenomegaly Early Sickle cell/ Thalassaemia Young child of afro-carribean ethnicity – not likely spherocytosis/eliptocytosis No jaundice, some conjunctival pallor Anaemia No tenderness, splenomegaly – Late SC anaemia spleen would be infarcted (not palpable) Congenital Abnormalities requiring surgery Congenital abnormalities which require abdominal surgery but leave the child well: Omphalacele, Gastroschisis, Meconium ileus, NEC (necrotising enterocolitis – usually premies), Malformations of gut (eg duodenal atresia, biliary atresialivertransplant etc.) It’s worth making a short list of what you would expect to find – don’t spend too much time doing this though (they don’t expect you to be paediatrician just yet!!)