Antibiotics for Community-Acquired Pneumonia: What is the
advertisement
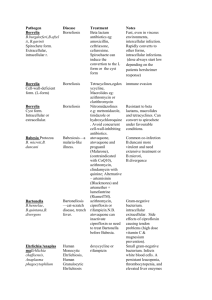
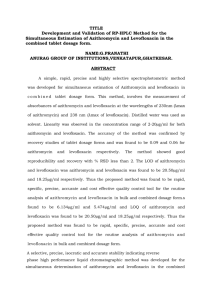
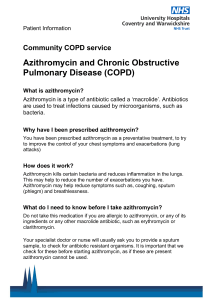
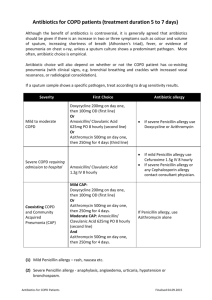
Thank you for viewing this presentation. We would like to remind you that this material is the property of the author. It is provided to you by the ERS for your personal use only, as submitted by the author. 2014 by the author Macrolide Therapy for Pneumonia: Balancing Benefits with Cardiovascular Risks Eric Mortensen, MD, MSc, FACP Faculty Disclosure • I have no relevant conflicts of interest nor will discuss “off label” use of any medications Community-Acquired Pneumonia (CAP) • Leading infectious cause of death • Since 1950 mortality has been stable or increasing • Increased incidence with aging of the population CAP Clinical Practice Guidelines • • • • • • • ATS- 1993 and 2001 IDSA- 1998, 2000, and 2003 BTS- 1993 and 2001 CIDS/CTS- 1993 and 2000 CDC- 2000 ERS- 2005 and 2011 IDSA/ATS- 2007 Mandell et al. ,Clin Infect Dis, 2007. 44 Suppl 2: p. S27 Woodhead et al. Clin Micro Infect 2011. 17 Suppl. 6, 1–24 IDSA/ATS Outpatient Antibiotic Recommendations • No risk factors for drug resistant S. pneumoniae (DRSP) • Macrolide or doxycycline • Has risk factors for DRSP or significant comorbid conditions • Anti-pneumococcal fluoroquinolone • -lactam + macrolide or doxycycline IDSA/ATS Inpatient Antibiotic Recommendations • Wards -lactam + macrolide or doxycycline – Anti-pneumococcal fluoroquinolone alone • ICU -lactam + azithromycin or fluoroquinolone Beneficial Effects of Macrolides on the Inflamed Airway Kanoh S , and Rubin B K Clin. Microbiol. Rev. 2010;23:590-615 Macrolides for Pneumonia • Erythromycin • Clarithromycin • Azithromycin Factors Associated With Mortality And Lengthy Of Stay In Elderly Patients With CAP- Azithromycin vs. Clarithromycin Sánchez F et al. Clin Infect Dis. 2003;36:1239-1245 Macrolide versus non-macrolide therapy and mortality in critically ill patients with community-acquired pneumonia: primary analysis (n=27) Sligl, W, et al. Critical Care Medicine. 42(2):420-432 Ray WA, et al. NEJM. May 17 2012; 366(20):1881-1890 Cumulative Incidence of Cardiovascular Death and Death from Any Cause for Patients Who Took Azithromycin vs Amoxicillin Ray WA et al. N Engl J Med 2012;366:1881-1890. Cardiovascular Death and Death from Any Cause among Patients Who Took Azithromycin vs. no Antibiotics Ray WA et al. N Engl J Med 2012;366:1881-1890. Svanström H et al. N Engl J Med 2013;368:1704-1712 Risk of Death from Cardiovascular Causes with Azithromycin Use as Compared with No Antibiotic Use or Use of Penicillin V Svanström H et al. N Engl J Med 2013;368:1704-1712 Subgroup Analyses of the Risk of Death from Cardiovascular Causes with Current Use of Azithromycin as Compared with Penicillin V Svanström H et al. N Engl J Med 2013;368:1704-1712 EM Mortensen and coauthors Association of Azithromycin With Mortality and Cardiovascular Events Among Older Patients Hospitalized With Pneumonia Available at jama.com and on The JAMA Network Reader at mobile.jamanetwork.com jamanetwork.com Aim: To examine the association of azithromycin use with all-cause mortality and cardiovascular events for older patients hospitalized with pneumonia Mortensen et al. JAMA 2014 Inclusion Criteria • Hospitalized with pneumonia in VA health care system between FY 2002 and 2012 • > 65 years old • >3 outpatient visits in year prior & received outpatient medications • Received guideline-concordant antibiotic therapy and first dose given within 48 hours of admission Guideline-Concordant Antibiotic Regimes • Wards – Beta-lactam + azithromycin – Antipneumococcal fluoroquinolone alone • ICU – Beta-lactam + azithromycin – Beta-lactam + fluoroquinolone Mandell LA, et al. Clin Infect Dis. Mar 1 2007;44 Suppl 2:S27-72 Primary Outcomes • Mortality within 90-days • Cardiovascular events within 90-days – MI – Heart failure – Arrhythmia – Any Statistical Analyses • Propensity matching with score created using 59 variables including: – – – – Demographics (age, race, marital status) Comorbid conditions Severity of illness (ICU, vasopressors) Outpatient medications (statins, anti-diabetic) • Instrumental variable analysis – Chosen IV was proportion of patients receiving azithromycin in each hospital Results • Overall 73,690 patients from 118 hospitals meet inclusion criteria • Propensity-matched group composed of 63,726 patients Variable Age, mean (SD) Men Married ICU admission Mechanical ventilation Tobacco use Alcohol abuse Myocardial infarction Heart failure COPD Prior antibiotic therapy Azithromycin N=31,863 77.8 (7.4) 98.2% 52.5% 15.6% 5.2% 39.7% 4.5% 7.1% 25.7% 51.8% 31.3% No Azithromycin N=31,863 77.8 (7.4) 98.2% 52.4% 15.5% 5.3% 39.7% 4.5% 7.0% 25.6% 51.7% 31.1% After matching no significant differences (all p >0.3) Survival Curves by Azithromycin Use vs Nonuse Time to First Cardiac Event by Azithromycin Use vs Nonuse Outcomes after Propensity Matching Outcome Odds Ratio 95% CI 90-day mortality MI Arrhythmia Heart failure Any CV event 0.73 1.17 0.99 1.01 1.01 0.70-0.76 1.08-1.25 0.95-1.02 0.97-1.04 0.98-1.05 Instrumental Variable Analysis Average Marginal Effect Outcome of Azithromycin Mortality -0.08 Any CV Event -0.004 Heart Failure -0.04 MI 0.03 Arrhythmia 0.01 Azithromycin users had • 8% lower probability of mortality • 4% lower probability of HF • 3% higher probability of MI Bootstrapped 95% CI -0.10 to -0.07 -0.02 to 0.02 -0.06 to -0.02 0.02 to 0.04 -0.01 to 0.03 Secondary Analyses • No prior outpatient antibiotics – 90-day mortality OR 0.74 (0.71-0.78) – Any CV event OR 1.02 (0.97-1.06) • Prior cardiac disease – 90-day mortality OR 0.72 (0.67-0.77) – Any CV event OR 1.04 (0.97-1.11) • Invasive mechanical ventilation – 90- day mortality OR 0.81 (0.70-0.93) – Any CV event OR 1.24 (1.08-1.43) ConclusionsAzithromycin and CAP • Azithromycin use associated with lower mortality but higher rate of MI – NNT to prevent 1 death- 21 – NNH to cause 1 MI- 144 – Net benefit: 7 deaths averted for each non-fatal MI Summary • Macrolides are part of guidelineconcordant pneumonia therapy • Azithromycin is associated with some increased cardiac risks, but… • For pneumonia, benefits of azithromycin outweigh risks Questions? Eric.Mortensen@UTSouthwestern.edu