FIBThrombocytes & Coagulation
advertisement

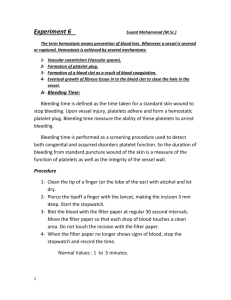
Thrombocytes and Coagulation VTHT 2323 CLINICAL PATHOLOGY KRISTIN CANGA, RVT Reading Assignment A&P: PG. 230 LAB PRO: PP. 30-32 (ANTICOAGULANTS) AND 69-73 Thrombocyte Formation Production of platelets = ___________________________ Produced in bone marrow by __________ _________________________(TPO) = stimuli for PPSCs to differentiate into thrombocyte precursor. Platelet parent cell = _________________________________ Thrombocyte Formation Megakaryocyte undergoes incomplete ___________: (___________________ divides but cytoplasm doesn’t) Small chunks (~1,000 – 5,000 per megakaryocyte) break off while still in bone marrow, and are sent into circulation as platelets Some platelets are stored in ______________ for release as needed Megakaryocytes Megakaryocyte Megakaryocytes Megakaryocytes: Platelet formation Infoldings develop into plasma membrane that divide marginal _______________ into little compartments. These compartments break off and enter bloodstream as ______________. Some platelets are stored in the ___________, while others circulate freely in the blood and live for about ________ days in dogs and just over ___ day in cats. Megakaryocyte Video http://www.youtube.com/watch?v=6R- ESPFiKbo&feature=related&ajax=1&nocache=12710 11451258 Thrombocytes Commonly referred to as ________________. Not complete cells (lack a ____________), but frequently listed as one of the cell types in peripheral blood. RBCs>PLTs>WBCs Have a greater variety of _________________than any of the true blood cells. Are responsible for _________________phase of clot formation AND initiation of ________________phase of clot formation. Thrombocyte Morphology Most are _______________than RBCs Most PLTs in circulation are _____________ and have numerous, small, purple/pink _____________ scattered throughout the cytoplasm. Occasionally _________ platelets are seen in blood smear Giant platelets are considered more _______________ than smaller platelets Giant Platelet in Peripheral Blood L T Platelets… Play a part in both the __________________ and __________________ formation of clots. Secrete ________________________ Form platelet plugs Secrete ____________________ Initiate dissolution of blood clots (“_______________________”) Secrete _______________that attract neutrophils and monocytes to sites of inflammation Secrete ______________ factors to help maintain and repair blood vessels Normal Platelet Values Canine: 200,000 – 500,000 /µL Feline: 300,000 – 700,000 /µL All species: ____________ of ____________/µL Horses = ___________normal concentrations Cattle = ____________normal concentrations Animals will bleed spontaneously if PLT concentration is ≤ ____________ to ____________ /µL Normal Platelet Morphology Normal Platelet Morphology Function of Platelets Platelets are essential for ________________. Role of platelets depends on ______________ numbers being present in the blood. There are 3 main functions of platelets: 1) Maintenance of __________________ integrity 2) _________________________ formation 3) ______________________ of plug by contributing to ______________ formation. Function of Platelets: 1) Vascular Integrity Platelets attach to _______________________ Release endothelial ____________ factor into endothelial cells. (Prevents leakage of blood in to tissues) ________________ or _______________may occur if there are __________________ numbers of platelets in circulation. Platelets: 2) Plug Formation Damaged blood vessel initiates the _________________ process of clot formation. Platelet _________________ The platelets adhere ______________ to the damaged vessel AND each other. __________ often affects this step in the clotting process Change shape and form ______________ Allows platelets to intertwine with each other to create platelet __________________. Platelet ______________________ The intertwining of platelets to help stop bleeding and causes the release of _________________ factors. Initiates the _________________ Function of Platelets Platelets: 2) Plug Formation, cont’d Release of platelet factors (PFs) that are necessary for the clotting process to be complete. The aggregation of platelets _______________ the release of PFs Platelet _______________ occurs after aggregation of platelets. This is the beginning of the _______________ phase of clot formation. Platelet Activation Platelets become activated when there is _____________ to the lining of a blood vessel The platelets are attracted to the damaged area and stick to it. Once the platelet has stuck to the damaged vessel, it becomes activated. Activated platelets have a ______-like appearance and form __________“tails” as they try and catch other platelets. Dendritic “tails” are sometimes referred to as __________________________ Activated Platelets Normal Activated Platelets Platelets that have been slightly activated in the sample or by contact with the glass slide (as is common in feline samples) have a stellate form with dendritic processes ("a" in figure). The inset shows a large platelet with centrally aggregated granules which resemble a nucleus. Platelet Clumping Platelet Clumps Thrombocytosis Platelet Clumps Platelet Function: 3) Stabilization of Platelet Plug Often referred to as the “______ Matrix” or “Clotting __________” Each step must happen in _________ and ________________ in order for the next step to occur. “____________ Reaction” Converts soluble ______________ to insoluble _________ strands among platelets. Acts as “scaffolding” to encourage ____________. Fun Video Introduction to Coagulation http://www.youtube.com/watch?v=9QVTHDM90io Hemostasis Hemostasis is the process by which blood is prevented from leaking out of _____________ blood vessels. Depends on three factors: _____________ of blood vessels Presence of adequate ___________________ factors Adequate number of normal circulating ______________. ___________ is a key player!!! 1. Manufactures most clotting factors 2. Bile = essential for _____________ of vitamin ___ Stages of Coagulation ______________ Hemostasis _________________________ Primary _______________ plug formation Platelet _______________ Platelet ________________ Does adhesion or aggregation CAUSE platelet activation? Stages of Coagulation _________________ Hemostasis _________________ Cascade Ultimate goal = __________ for stabilization of platelet plug Involves three pathways to clotting: __________________ Pathway, __________________ Pathway, and __________________ Pathway Stages of Coagulation Tertiary Hemostasis (________________) _________ retraction – occurs after ~___ minutes Platelet Derived ______________ Factor (PDGF) is secreted during clot retraction. _____________ damage to all tissues involved Tissue ____________________ Activator is secreted Clot initiates its own ____________________. Coagulation Simplified Extrinsic Clotting Mechanism • chemical outside of blood triggers blood coagulation • triggered by thromboplastin (not found in blood) • triggered when blood contacts damaged tissue Intrinsic Clotting Mechanism • chemical inside blood triggers blood coagulation • triggered by Hageman factor (found inside blood) •Triggered when blood contacts foreign surface The Coagulation Cascade Automated Hemostasis Testing Samples should be collected very carefully with minimal ________________ damage. ___________ collect sample through indwelling catheters. Can cause ___________ or blow the vein through manipulation. Anticoagulant of choice = Sodium citrate Blocks calcium (but not as strongly as EDTA) Blue top tube (a.k.a – turquoise) Results of some testing may be affected by stress, illness, recent exercise, heat cycle (females) Clotting Tests Assess one or more of the phases of ________________ (primary, secondary or tertiary) Tests involving ______________ hemostasis assess intrinsic, extrinsic and/or common pathways. All patients should undergo coagulation testing prior to undergoing a __________________ procedure. Platelet estimation Buccal mucosal bleeding time Activated clotting time (ACT) Prothrombin time (PT) Partial thromboplastin time (PTT) Fibrinogen assay Platelet Counting Methods ____________ or _______________ (least accurate) Most inaccuracies attributable to _______________, giant platelets, RBC _____________ Always use ___________ sample to minimize error Manual methods: 1. Platelet estimation during blood film analysis 2. Formula? ALWAYS USE HIGH POWER, _______________________ Unopette system & hemocytometer (NOT COMMONLY USED) Buccal Mucosal Bleeding Time Tests _____________ hemostasis Evaluates platelet __________ & _____________(thrombocytopathy, thrombocytopenia) Evaluates endothelial cell function (__________) Test can be affected by certain ___________________ BMBT Procedure 1. 2. 3. 4. 5. 6. Place _______________ animal in _____________ recumbency. Use a strip of gauze to tie upper lip back and expose mucosal surface. (Also acts as ______________) Using a Surgicutt® or a Simplate® lancet, create a small wound (~1 mm deep) Remove blood with filter paper at 30-second intervals DO NOT TOUCH SKIN Stop timing when there is no more blood. Normal = ________ minutes (canine/feline) Buccal mucosal bleeding time Toenail Bleeding Time An alternative to BMBT Clip toenail just past quick to cause bleeding Keeping animal undisturbed, monitor for bleeding to cease Normal = <5 minutes (canine/feline) Activated Clotting Time (ACT) Evaluates _________________ hemostasis (all factors except Factor VII) Requires Vacutainer containing sterile _____________________ earth to activate coagulation pathways 2 mL of blood is collected directly into tube It is important that tube is pre-warmed and kept at 37º C. Test can be affected by significantly ______ platelet numbers Normal = ___ – ___seconds (canine/feline) Prothrombin Time (PT) Evaluates adequacy of factors associated with _______________ and ___________ pathways Routinely done by ___________ Factor XIII activity not evaluated Platelet substitute added to sample (thrombocytopenia does not interfere) Normal: Canine = 6.4 - 7.4 seconds; Feline = 7 - 11.5 seconds Partial Thromboplastin Time (PTT) Evaluates adequacy of factors associated with the ___________ and ____________ pathways Routinely done by machine Factor XIII activity not evaluated Platelet substitute added Normal: Canine = 9-11 seconds; Feline = 10-15 seconds Fibrinogen Assay Can be done by ___________ or ________________ methods Only evaluates _________________ concentration Can use ____________ anticoagulated sample Concentrations may be increased during __________________ or decreased when consumed during coagulation (_________) Normal: Canine = 100 – 250 mg/dL Feline = 100 – 350 mg/dL Other Coagulation Tests Whole Blood Clotting time Clot Retraction Test One-Stage Prothrombin Time (OSPT) Used to confirm warfarin toxicity (rodenticide) Activated Partial Thromboplastin Time (APTT) PIVKA (proteins induced/invoked by vitamin K absence) d-Dimer and Fibrin Degradation Products Quick Coagulation Testing Coagulopathy Coagulation defects can be categorized as: Coagulation defects of primary hemostasis Coagulation defects of secondary hemostasis Defects of fibronolysis (tertiary hemostasis) Coagulation Defects of Primary Hemostasis Coagulation defects of primary hemostasis _______________________ or ____________________ (Quantity or quality) ________________ bleeding Petechiae, mucosal bleeding, ecchymoses, epistaxis, melena, prolonged bleeding Coagulation Defects of Primary Hemostasis ___________________________ Decreased _______ number Can be _________________ or _________________ #1 cause = infectious disease Ehrlichia, rickettsial diseases, babesiosis, systemic mycoses, toxoplasmosis, mycoplasmosis, Feline retroviruses (FeLV, FIV, FIP), others Other causes = bone marrow depression; unknown ______________________________ (vWd) Decreased or deficient vWF= decreased PLT _____________ , aggregation, and fibrin cross linking Can occur secondary to ______________________ CS: MM hemorrhage, hematuria, GI bleeding, epistaxis Screening test of choice = _____________ Defects of Secondary Hemostasis Coagulation defects of secondary hemostasis _____________(e.g. pleural, peritoneal, retroperitoneal) __________________formation Delayed bleeding/re-bleeding Coagulation Defects of Secondary Hemostasis Congenital clotting factor deficiencies of virtually all known factors have been described. (e.g.: Hemophilia A & B) _____________ coagulation defects can result from: #1 = ________________ toxicity Inhibits vitamin K Vitamin K is required to activate factors II, VII, IX, and X One-step prothrombin time = test to confirm ______________ toxicity. Liver disease, infiltrative bowel disease, and biliary obstruction can also inhibit Vitamin K Disseminated Intravascular Coagulopathy (DIC) Not a disease in itself; it is a complex _________________ that results from a pathologic condition. Involves __________________ activation of platelets, coagulation proteins, and plasmin; evolving into consumption of coagulation proteins, platelets, and inhibitors of fibrinolysis Some of the many pathologic conditions associated with initiation of DIC include: Trauma and burns Metabolic acidosis/severe shock A large number of infectious diseases _________________________ Systemic infection ________________________ disease _________________________ Sometimes considered an “_______________ ” condition DIC Laboratory findings are highly _________________ Classically ACT, PTT, PT, and thrombin time are prolonged; fibrinogen and platelet counts are decreased _________________________ seen on smear Diagnosis is based on clinical suspicion and at least 3 abnormal coagulation test results. Clinical signs depend on the phase in which the patient is experiencing _____________/Subacute phase: may have few to no overt clinical signs ___________ (consumptive) phase: characterized by venipuncture oozing or modest to severe hemorrhage with inability to form a normal clot ______________ phase: charactized by no clinical signs or oozing of blood Death is caused by extensive microthrombosis or circulatory failure, leading to single or multiple organ failure Treatment of DIC Successful treatment depends on early detection in critically ill animals. Involves: CORRECTING UNDERLYING _____________________ Support of target organs where microthrombi may cause hemorrhage Coagulation factor __________________therapy Administration of _______________ as needed (controversial) Fluid therapy – balanced electrolyte solutions to maintain effective circulating volume Should be accompanied by administration of _____________ Close monitoring of antithrombin activity Prognosis is usually _______; depends on underlying cause If an animal survives an acute DIC event, a ___________ form of DIC can exist Other Acquired Coagulation Defects of Secondary Hemostasis _________________ Disease The __________ synthesizes many of the clotting factors including factors I, II, V, VII, VIII, IX, X, XI, and XII Liver manufacturers __________ which is essential in absorption of vitamin ___ from diet Disseminated Intravascular Coagulation (DIC) A complex syndrome with systemically accelerated coagulation It is clinically difficult to differentiate between hepatic disease and DIC because PT and PTT are usually prolonged with both. DIC can occur secondary to hepatic disease. Qualitative Platelet Dysfunction Thrombocytopathia Most common cause is inappropriate use of ________________. Can also be caused by: ________________________________ disorders Rare _____________________ problems Certain _______________ Thrombocytopathy: Drugs Causing Platelet Dysfunction Table 10-3. Drugs Affecting Platelet Function Anesthetics General – Halothane Local - Procain Antibiotics Cephalosporins – Cefazolin Penicillins - Ampicillin Anticoagulants Heparin Antihistamines Chlorpheniramine Cardiovascular drugs Propanolol, Verapamil Foods and food additives Ethanol, onions Non-steroidal anti-inflammatory drugs Aspirin, Phenylbutazone Oncologic drugs Daunorubicin Plasma Expanders HetaStarch, Dextrans Miscellaneous drugs Chlorpromazine Tertiary Hemostatic Dysfunctions (Defective Fibrinolysis) The most common dysfunctional state is excessive _____________________. This is an uncommon disease. Fibrinolysis ______________ can also cause thrombus formation (a condition, not a disease state) Other Bleeding Disorders Bleeding disorders may be caused by _____________ or ______________ defects in coagulation proteins, platelets, or vasculature. Inherited coagulation defects are usually associated with a _________ coagulation protein and often occur at a ____________age. Acquired coagulation defects often affect ________________ coagulation proteins and can occur at _________ age. Anticoagulants and Hemostasis As you already know, anticoagulants _____________ or ____________ the formation of a clot. Anticoagulants are an important part of blood collection. Different anticoagulants are utilized depending on the _____________ that are needed. On the following slides, we are going to talk about each anticoagulant and how it can affect your sample. Heparin Heparin is acceptable for most tests requiring ________________. (Green top) Heparinized tubes should be used for _______________ chemistry analyzers. Heparin acts on the clotting cascade by preventing the conversion of __________________ to ____________ during the clotting process. Heparin also may cause _____________of WBCs Heparin interferes with the _______________ of WBCs and should not be used for blood films. Ethylenediamine Tetraacetic Acid Commonly referred to as ___________ (Purple top) Preferred anticoagulant for blood films because it does not alter cell _______________________. Prevents clotting by binding with _______________ , which is necessary for clot formation. Should not be used for ____________ analysis because it affects the metabolism of certain chemicals in the blood and may ____________________ increase or decrease those chemicals. ______________ EDTA can cause shrinkage of _____ This will invalidate automated chemistry machines. Oxalates Available as: _________oxalate, ______________ oxalate, ______________ oxalate, or ______________oxalate. _____________________ oxalate is most commonly used. (Grey top) Prevents clotting by binding with __________, which is necessary for clot formation. Not frequently used as it interferes with potassium tests, alkaline phosphatase tests, and lactate tests. Citrates Available as: ______________citrate, or __________________citrate. Blue top Commonly used in ________________ medicine Prevents clotting by binding with calcium, which is necessary for clot formation. Interfere with ___________tests and many of the tests performed by ________________ chemistry analyzers. Sodium Flouride Known as __________ preservative but does have anticoagulant properties Prevents clotting by binding with calcium, which is necessary for clot formation. May be added to other samples that already have an ______________________. Also _________top! Interferes with many _______________ tests performed by automated analyzer. Commonly Used Anticoagulants Table 2-2 Name Mode of Action Advantages Disadvantages Uses Heparin Antithrombin Reversible, nontoxic Clumps WBCs, expensive, staining interference Critical RBC measurements EDTA Chelates calcium Best preservative Irreversible, shrinks cells Hematology Oxalates (potassium, Na, lithium) Chelates calcium Temporary Variable effects Coagulation Citrates (Na, lithium Chelates calcium Nontoxic, reversible Interferes with blood chemistry Transfusions, coagulation Fluorides (Na) Chelates calcium Inhibits cell metabolism Interferes w/ enzymatic tests Preserves blood glucose