- ePrints Soton
advertisement

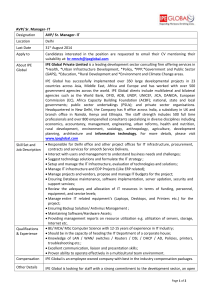
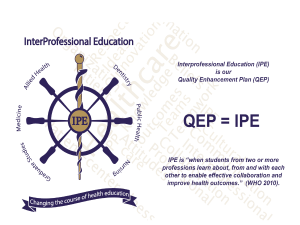
LESSONS LEARNT FROM A NATIONAL STUDY OF PRE-REGISTRATION INTERPROFESSIONAL EDUCATION IN THE UNITED KINGDOM Dr. Deborah Craddock University of Southampton Introduction Crucial ability to learn and work in a multidisciplinary team (WHO 2008). Interprofessional education (IPE) aims to reinforce inter-professional practice (DOH 2000a; DOH 2000b; Carpenter, 2005). IPE is a mandatory requirement in the United Kingdom (UK) for pre-registration training in health and social care (DOH & QAA, 2006). Varying models of IPE in undergraduate curricula (Roberts et al., 2000) Evidence base for the effectiveness of such programmes is growing (Hammick et al., 2007; Hean, Craddock & O’Halloran, 2009). Research Aim: To explore the potential influence of IPE at pre-registration level, using podiatry as an exemplar. Research Objectives: 1. To evaluate health and social work students’ awareness of podiatrists’ roles on two occasions1 across participating HEIs; 2. To explore health and social work students’ views of interprofessional learning (IPL) on two occasions1 across participating HEIs; 1 Sample 1: students at the start of their Level 1 IPE initiative; Sample 2: students on completion of their IPE Level 1 initiative Methodology Two prospective cross-sectional surveys Ethical approval Multi-stage sampling:- (1) sampling of HEIs & (2) sampling of students Questionnaires were administered to a volunteer sample of pre-registration health and/ or social work students in Higher Education Institutions within the UK at 2 separate time points. Inclusion criteria: Students registered on a health or social care programme participating in an IPE initiative that involved podiatry students. Questionnaire Pack Questionnaire pack- informed by (1) key informant interviews and (2) research evidence Validated tools – Readiness for Inter-professional Education Scale [RIPLS] & Generic Role Perception Questionnaire Face validity Content validity Pilot Study [test (i) n=67; test (ii) n=62] Test re-test reliability Internal consistency Key informant interviews Sample: Sample 1: Sample 2: 1151 students participated in 1060 students participated in the Sample 1 phase [81.1% the Sample 2 phase [81.2% (933) female, 18.9% (218) (861) female, 18.8% (199) male]: mean age 24.38 male]: mean age 24.32 (SD=8.167) years in 6 HEIs (SD=7.84) years in 5 HEIs. Excluding students registered on a BSc (Hons) podiatry Excluding students registered on a BSc (Hons) podiatry programme: Sample 1 sample size- 964 students [82.2% programme 967 students (792) female, 17.8% (172) [81.7% (790) female, 18.3% male]: mean age 23.62 (177) male]: mean age 23.82 (SD=7.50) years in 6 HEIs (SD=7.46) years in 5 HEIs. Female : Male (Parsell and Bligh 1999; Cassidy 2007) Objective 1 Evaluating health and social work students’ awareness of podiatrists’ roles on two occasions1 across participating HEIs; 1 Sample 1: students at the start of their Level 1 IPE initiative; Sample 2: students on completion of their IPE Level 1 initiative 41.4% (399) participants in Sample 1 and 51.4% (497) participants in Sample 2 participated in an IPL group that included a podiatry student. Of these participants in Sample 1, only 20.4% (48) participants who claimed to be aware of podiatrists’ roles, perceived there to be no difference between chiropodists and podiatrists. In Sample 2: greater percentage number42.7% (180). Perceptions of podiatrists’ roles: carrying out nail surgery for an ingrown toenail (Sample 1: 82.2%, 792; Sample 2: 80%, 774) manufacturing shoe devices (Sample 1: 54.5%, 525; Sample 2: 54%, 522) surgically removing bunions (Sample 1: 57.2%, 551; Sample 2: 57.5%, 556) At Sample 2 only, podiatrists were also identified as the key professional who treats verrucae (70.2%, 679). Other roles: Managing walking and mobility problems Assessment of patients/ clients for vascular disease Managing ulcerations Assessing children for gait or developmental anomalies Only at HEI B did students have a greater understanding of podiatrists’ roles between Sample 1 and Sample 2 (Sample 1: Md=8, Sample 2: Md=10, U=7513, z=-5.294, p<0.001, r=-0.3) Note: Higher median scoreSample 2 Educational theory underlying IPE initiative Sample 1: A Kruskal-Wallis Test highlighted a significant HEI D recorded the highest difference in students’ median knowledge score (Md=8.5) knowledge of podiatrists’ roles and their institution of origin HEI K and HEI H recorded the lowest median knowledge score (Md=6) Sample 1: H=38.948, 5df, p<0.001, n=964; Sample 2: H=122.87, 4df, p<0.001, n=967. Sample 2: HEI D and HEI B recorded the highest median knowledge scores (Md=9) HEI K recorded the lowest median knowledge score (Md=6) Students’ knowledge podiatrists’ roles was better if they had participated in an IPE group that involved a podiatry student (Md=7) than students who did not or were unsure as to whether they had participated in an IPE group that involved a podiatry student (Md=6) (Sample 1: U=101791.00, Z=-2.596, n964, p=0.009; Sample 2: U=72529.5, z=-10.272, n=967, p<0.001). Podiatry students’ awareness of their own profession’s roles was greater in Sample 2 than Sample 1 (Sample 1 Md=10, n=187; Sample 2 Md=12, n=93; U=4703.5, z=6.301, p<0.001). A positive correlation was evident between age and knowledge of the podiatrists’ role (Sample 1: spearman’s rho= 0.097, n=964, p=0.001; Sample 2: spearman’s rho= 0.059, n=067, p=0.032 for a one tailed test) respectively. Generic Role Perception Questionnaire A Mann-Whitney U test revealed a significant difference between Scale with 20 items that has good students’ perceptions of podiatrists’ internal consistency (Cronbach roles in Sample 1 (Md=92, n=964) alpha=0.7; n=43) (MacKay, 2004) and in Sample 2 (Md=97, n=967) [U=404704.5, z=-5.012, p<0.001, r=-0.11]. GRPQ (MacKay, 2004) Principal Components Analysis with Oblimin rotation In Sample 2 a significant difference was observed in students’ total Sample 1- four components GRPQ scores between health and solution (Cronbach alpha=0.776) social work students who participated in an IPE group that involved a podiatry student (Md=94, n=497) and students who either did Sample 2- three components not or were unsure as to whether solution (Cronbach alpha=0.78) they had participated in an IPE group with a podiatry student (Md=99, n=470) [U=101817.50, z=-3.451, p=0.001, r=-0.11]. Objective 2 Exploring health and social work students’ views of interprofessional learning (IPL) on two occasions1 across participating HEIs; 1 Sample 1: students at the start of their Level 1 IPE initiative; Sample 2: students on completion of their IPE Level 1 initiative) IPE has been introduced into preregistration curriculum to: help health and/or social care professionals to be able to work more effectively together NOT weaken the power of the professions (Sample 1: 82.7%, (Sample 1: 97.5%, 1098; 952; Sample 2: 74%, 784) Sample 2: 94.6%, 1003) Increase cost effectiveness of enhance the quality of care patient care (Sample 1: 52.2%, given to patients (Sample 1: 601; Sample 2: 57.5%, 610) 95.4%, 1098; Sample 2: 92.8%, 984) Minimise the risk of any duplication of health service Improve communication skills delivery (Sample 1: 45%, 518; (Sample 1: 94.4%, 1086; Sample 2: 53.8%, 570) Sample 2: 91.3%, 968) Increase confidence in professional roles (Sample 1: 87.3%, 1005; Sample 2: 82%, 869) Students’ Perceptions of IPE Disagreement that campus based IPE opportunities were perceived as being more meaningful than placement based learning opportunities (Sample 1: 46.3%, 533; Sample 2: 51.1%, 542) Rivalries exist in placement locations that expose students to stereotypical views of professions (Sample 1: 43.5%, 500; Sample 2: 47.2%, 501) Key Motivational Influence: use of clinical/ social scenarios in group-work activities (Sample 1: 81.6%, 939; Sample 2: 71.1%, 753) Commitment to IPE: Positive correlation - age and level of commitment to IPE (Sample 1: spearman’s rho = 0.243, p<0.001; Sample 2: spearman’s rho = 0.165, p<0.001 for a one tailed test) Commitment was strongly influenced by: facilitators’ attitudes towards IPE (Sample 1:75.5%, 835; Sample 2: 74%, 784) Modal response of 6 - the majority of participants were working practices of staff only fairly committed (Sample (72.4%, 833; Sample 2: 66%, 1: 49.5%, 570; Sample 2: 46.9%, 700); 497) to IPL. Students induction to the IPE initiative (62.2%, 716; 56.2%, 596) Commitment to IPE Yet the majority of respondents had not read any information about IPE (Sample 1: 65.7%, 756; Sample 2: 60.8%, 644) Primary information sources accessed by students who had read information about IPE: Sample 1 N (21%; 242) Sample 2 n (21.8%, 231) Websites 47.5%, 115 Course materials 40.7%, 94 Course materials 47.1%, 114 Websites 30.3%, 70 Books 18.6%, 45 Books 27.3%, 63 Journals 22.5%, 52 Discussions 17.8%, 43 Students who had read information: – Developed a better appreciation of the need for multidisciplinary team members to meet on a regular basis in order to plan and discuss issues (Sample 1: U=99499.5, z=2.569, p=0.01, r=-0.08; Sample 2: U=82170, z=-3.704, p<0.001, r=-0.11). – Enabled students to gain an appreciation of the existence of rivalries in placement locations that may expose students to stereotypical views of other professions (Sample 2: U=87109.5, z=-2.223, p=0.026, r=-0.07). Readiness for Inter-professional Learning Scale Principle Component Analysis Kaiser-Meyer-Oklin value = Sample 1: 0.932; Sample 2: 0.938 Bartlett’s Test of Sphericity (p<0.001) Oblimin rotation with Kaiser Normalisation Sample 1 and 2: 2 component solution Comparisons with Parsell and Bligh (1998; 1999) & McFadyen et al. (2005) Component 1 Teamwork and collaboration Component 2 Professional identity and roles RIPLS Subscale Comparisons Sub-scale 1 Sub scale 2 Subscale 3 Teamwork and collaboration Professional Identity (1999) and Negative Professional Identity (1998) Roles and Responsibilities (1999) + Roles (1998) Items 1-9 Items 10-16 Items 17-19 Parsell et al., (1998) (n=914) Items 1-9 Item 12 Item 18 48% variance explained Item 11 Item 17 Items 13-16 Item 19 McFadyen et al (2005) (n=308) Items 1-9; 10, 11 Item 12 (n=308) 44% variance explained Items 13-16 Item 17 Craddock Sample 1: n=1151 45.4% variance explained Items 1-9 Items 10-12 Items 13-16 Items 17-19 Factor Analysis Parsell and Bligh (1999) (n=120) 42% variance explained Craddock Sample 2: n-1060 52.7% variance explained Items 18-19 Cronbach Alpha Measure of Internal Consistency of Each Sub-scale Study Sub-scale 1 Sub scale 2 Subscale 3 Teamwork and collaboration Professional Identity (1999) and Negative Professional Identity (1998) Roles and Responsibilitie s (1999) + Roles (1998) Parsell and Bligh (1999) (n=120) 0.88 0.63 0.32 Parsell et al., (1998) (n=914) 0.85 0.46 - McFadyen et al (2005) (n=308) 0.80 0.21 0.40 Craddock (n=1151) 0.88 0.66 Craddock (n=1060) 0.92 0.79 Pre-registration health and social work students’ perceptions of IPL Significant difference between: Students’ total RIPLS scores in Sample 1 (Md=80, n=1151) and Sample 2 (Md=76, n=1060), U=498010.00, Z=-7.474, p<0.001, r=-0.16. – Findings echoed in relation to each sub-scale – Students’ total RIPLS scores in Sample 1 and Sample 2, for HEIs B, E, K and H. Students at HEIs B and K had the highest RIPL and HEI F had the lowest. Lessons Learnt Student Preparation Assessment Task Enhancing knowledge of professional roles Focus of learning outcomes Make-up of IPE groups Formal & informal learning opportunities Lessons Learnt Key role of facilitators- staff training Key factors influencing students’ attitudes towards IPE Induction process Working practices of staff Lessons Learnt: Value of placement based learning (Guest et al 2002; Lumague et al., 2006; Robson and Kitchen, 2007) Recognised reservations: practicability (Cook et al., 2001) Lack of clinical experience (Young et al., 2007) Placement Based Learning not possible? Stimulus materials in IPE initiatives linked to the practice setting. Existence of rivalries in practice (Robson and Kitchen, 2007) Lessons Learnt: RIPLS (Parsell and Bligh, 1999) Timing of IPE Role of reading about IPE Target course materials where links are incorporated to key IPE websites > age of students > Target & engage younger students e.g. induction level of commitment – (see, Stephens et al., 2007) References Carpenter, J. (2005) Evaluating the Outcomes of Social Work Education. London and Dundee: Social Care Institute for Excellence and Scottish Institute for Excellence in Social Work Education. Cook, A., Davis, J. and Vanclay, L. (2001) Shared learning in practice placements for health and social care students in East London: A feasibility study. Journal of Interprofessional Care, 15(2): 185–190. Department of Health (2000a) A Health Service of all the Talents: Developing the NHS Workforce. Consultation document on the review of workforce planning. London: Department of Health. Department of Health (2000b) The NHS Plan: A plan for investment, a plan for reform. London: The Stationery Office Ltd. Department of Health and QAA (2006) Department of Health Phase 2 Benchmarking Project – Final Report. London: Department Of Health; and Gloucester: Quality Assurance Agency for Higher Education. Hammick, M., Freeth, D., Koppel, I., Reeves, S. and Barr, H. (2007) A best evidence systematic review of interprofessional education (Best Evidence Medical Education Guide No 9). Medical Teacher, 29(8): 735–751. Hean, S., Craddock, D. and O’Halloran, C. (2009) Learning theories and interprofessional education: A user’s guide. Learning in Health and Social Care, 8(4):250-262. MacKay, S. (2004) The role perception questionnaire: A tool for assessing undergraduate students’ perceptions of the role of other professions. Journal of Interprofessional Care, 18(3): 289–302. References: (continued) McFadyen, A.K., Webster, V., Strachan, K., Figgins, E., Brown, H. and McKechnie, J. (2005) The readiness for interprofessional learning scale: A possible more stable sub-scale model for the original version of RIPLS. Journal of Interprofessional Care, 19(6): 595–603. Parsell, G. and Bligh, J. (1998) Shared goals, shared learning: Evaluation of a multiprofessional course for undergraduate students. Medical Education, 32(3): 304–311. Parsell, G. and Bligh, J. (1999) The development of a questionnaire to assess the readiness of healthcare students for interprofessional learning. Medical Education, 33: 95–100. Roberts, C., Howe, A., Winterburn, S. and Fox, N. (2000) Not so easy as it sounds: A qualitative study of a shared learning project between medical and nursing undergraduate students. Medical Teacher, 22(4): 386–391. Robson, M. and Kitchen, S.S. (2007) Exploring physiotherapy students’ experiences of interprofessional collaboration in the clinical setting: A critical incident study. Journal of Interprofessional Care, 21(1): 95–109. Stephens, J., Abbott-Brailey, H. and Pearson, P. (2007) It’s a funny old game: Football as an educational metaphor within induction to practice-based interprofessional learning. Journal of Interprofessional Care, 21(4): 375–385. Young, L., Baker, P., Waller, S., Hodgson, L. and Moor, M. (2007) Knowing your allies: Medical education and interprofessional exposure. Journal of Interprofessional Care, 21(2): 155–163. World Health Organisation (2008) Now more than ever: The World Health Report 2008. Geneva: WHO.