BRAIN DEATH: Outstanding ethic
advertisement

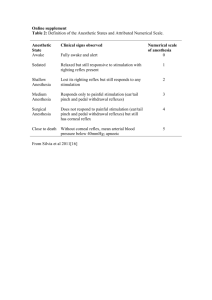
Lecture at the Faculty of Medicine King Saud University, Riyadh on March 12, 2014 by Dr Omar Hasan Kasule MB ChB (MUK), MPH (Harvard), DrPH (Harvard) Faculty of Medicine King Fahad Medical City Riyadh omarkasule@yahoo.com. A 60-year old comatose accident victim suffering from severe multi-organ traumatic injury and with a signed organ donation card was evaluated in the ER of a remote rural hospital. There was no other plausible cause of reversible coma or of brain death. Clinically: no pupillary reflexes, fixedly-dilated pupils, no corneal reflex, no eye movements, no blink reflex, no vestibule-ocular reflex, no cranial reflexes, and no gag reflex. Findings were equivocal regarding the apnea test, cephalic reflexes, and motor response to pain. Investigations: jugular vein partial oxygen pressure could not be determined. The EEG was isoelectric. Bedside trans-cranial Doppler showed no cerebral circulation. Family members with the exception of the mother were certain of death and asked the physician not to institute any life support and to call the organ harvesting team. The doctor was not sure what to do he however convinced the family to start life support to keep the organs viable until the transplant team arrived by helicopter. While walking along the corridor, a nurse overheard members of the family talking about a 15-year old cousin of the victim lying in a hospital in the A 40-year old billionaire stage 4 cancer victim with multi organ failure in ICU and on artificial life support Determined clinically dead on the basis of clinical signs repeated after 6 hours (pupillary reflexes –ve, fixedly-dilated pupils, corneal reflex –ve, eye movements –ve, blink reflex –ve, cold water test –ve, cranial reflexes –ve, apnea test –ve, cephalic reflexes –ve, motor response to pain –ve, gag reflex –ve). All confirmatory tests were also negative (jugular oxygen partial pressure -ve, EEG=0, CT angiography). Family members begged the physicians not to withdraw life support and not declare death until his beloved last daughter arrives from London. She might die from shock if she does not see him alive before death. They were willing to pay for the extra days of ICU stay. A 90-year old deeply comatose man with multiple organ failure was admitted to the last available ICU bed and was put on artificial life support minutes when the family refused a DNR order. A few minutes later ambulances started bringing in over 100 casualties from an air crash site. The head of the ICU carried out a rapid assessment of the comatose man showed equivocal clinical signs of brain death; some indicating death and others not. None of the confirmatory tests was positive Ethical issues relating to brain death are analyzable according to the purposes of the Law, maqasid al shari’at, and principles of the law, qawa’id al fiqh, to reach conclusions of practical importance. Motivation to declare death earlier: the need to harvest viable organs earlier, save intensive care resources, and obtaining tissues for research before deterioration. Violation of the principle of intention, qa’idat al qasd, which requires that actions be judged by underlying intentions and that the end does not justify the means. In this case the nobility of the ends and their public interest are motivating factors. The requirement, by the principle of certainty, qa’idat al yaqeen, of evidence-based proof of death are partially fulfilled by brain death criteria, tests, and examinations. There is consensus on clinical tests in determining brain stem death but no such consensus exists for confirmatory instrumental tests. The principle of custom, qa’idat al ‘aadat, is partially fulfilled because there is no universal consensus on criteria of brain deat Brain death criteria vary by country, by institution, and over time. Do we do brain death testing routinely or are we selective? Is repetition of the testing needed after 6, or 24 hours? How soon shall we act after brain stem death is confirmed clinically? Relevance of cerebral death vs brain stem death difference? Feasible?(a) other causes of reversible coma (b) plausible cause of brain death Protection of life, maqsad hifdh al nafs, vs and mistakes in death determination protecting resources, maqsad hifdh al mal, vs delayed death determination Pressure for organ donation: specific individual vs. general public Near death vs dead The criteria and determination of brain death do not fully conform to principles of intention, certainty, and custom. Considerations of organ harvesting, ICU costs, and research have been a driving force behind development of brain death criteria. These criteria have been changing with development of knowledge and technology and have not reached the level of universal consensus having variation by country and by institution. There is consensus about the reliability of clinical tests of brain stem death Brain stem death, determined by clinical examination with or without instrumental confirmation, should remain the mainstay of death definition The public interest in organ harvesting and saving ICU resources overrides the doubts that we may have about clinical criteria of brain death Legal rulings, fatwa, on brain death should be reviewed every 3 years to take into consideration new developments in medical knowledge and technology.