Case Scenario 1 History & Physical 4/3/12 HISTORY: Patient is a 62
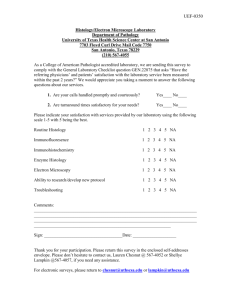
advertisement

Case Scenario 1 History & Physical 4/3/12 HISTORY: Patient is a 62-year-old white female with a history of classical Hodgkin lymphoma nodular sclerosis of stomach diagnosed in 2010. Patient was treated and has been disease free for more than a year. Patient presents now with cervical adenopathy. Over the last 3 months she has lost 10 pounds, had a low-grade fever, and experienced some night sweats. PHYSICAL EXAMINATION: Unremarkable except for significantly enlarged palpable tender left supraclavicular lymph nodes measuring more than 2.5 cm. No axillary lymphadenopathy. Heart and lungs and abdomen are unremarkable. No edema of the legs. All other systems are normal. Imaging 4/5/12 CT scan of chest: Multiple soft tissue densities in the bilateral supraclavicular areas. Suspect lymphoma. 4/5/12 CT abdomen/pelvis: Unremarkable. Procedure 4/9/12 Excisional biopsy of left supraclavicular node: Follicular lymphoma, grade 2 Oncology 6/11/2012 Patient has completed two courses of CHOP+rituximab. 1. Assign a histology code to each potential primary. 2. Assign a topography code to each potential primary. 3. Assign a grade code to each potential primary. 4. Apply the appropriate Hematopoietic Multiple Primary Rules to this case scenario. Indicate how many primaries this patient has and which rule was used to determine the number of primaries. 5. Indicate the primary site, histology, and grade for each primary. Case Scenario 2 History 3/14/12 Patient is a 73-year-old white female who has been having blood work followed for the last 2 years with close monitoring of CBC. She has had lymphocytosis since January 2012. Physical exam was within normal limits with no lymphadenopathy or organomegaly. She reports now to hematology for bone marrow biopsy. Procedure 3/14/12 Bone marrow biopsy: Peripheral blood smear: Lymphocytosis Bone marrow aspirate, particulate clot section and bone marrow core biopsy: Hypercellular bone marrow with trilineage hematopoiesis and involvement by chronic lymphocytic leukemia/small lymphocytic lymphoma. Oncology 9/10/12 Patient completed 8 cycles of CVP. Blood work indicates patient currently in remission. 1. Which module should be used to determine the primary site and histology for this case scenario? 2. What histology should be assigned to this case? 3. What primary site should be assigned to this case? 4. What grade should be assigned to this case? 5. For cases diagnosed 2012 and after when should the histology code 9670/3 be used? Case Scenario 3 Oncology 5/2/12 Patient has history of extranodal diffuse large B-cell lymphoma (DLBCL) treated with partial gastrectomy at another facility in 2004. Patient has had night sweats for the last 3 months and weight loss of about 15 pounds. Abdominal CT scan showed lymphadenopathy of abdominal nodes. Fine needle aspiration of abdominal nodes 2 weeks ago diagnosed DLBCL. Patient presents today for a VAD insertion as well as chemotherapy. 1. Assign a histology code to each potential primary. 2. Assign a topography code to each potential primary. 3. Assign a grade code to each potential primary. 4. Apply the appropriate Hematopoietic Multiple Primary Rules to this case scenario. Indicate how many primaries this patient has and which rule was used to determine the number of primaries. 5. Indicate the primary site, histology, and grade for each primary. Case Scenario 4 History & Physical 4/11/12 65-year-old white male presents with abdominal pain, weight loss of 20 pounds in last 6 months, and general malaise. Abdomen is distended. Slight swelling noted in left neck. Imaging 4/18/12 CT abdomen/pelvis: Large 15 cm mass involving terminal ileum, cecum, and adjacent mesentery. No lymphadenopathy present. 4/26/12 PET/CT: 2.5 cm glucose avid mass at base of tongue; left cervical node with adenopathy. Probable lymphoma. Procedures 4/24/12 Colonoscopy with biopsy of intestinal mass: Diffuse large b-cell lymphoma (DLBCL) 5/1/12 Biopsy of base of tongue: DLBCL 1. Assign a histology code to each potential primary. 2. Assign a topography code to each potential primary. 3. Assign a grade code to each potential primary. 4. Apply the appropriate Hematopoietic Multiple Primary Rules to this case scenario. Indicate how many primaries this patient has and which rule was used to determine the number of primaries. 5. Which module should be used to determine the primary site and histology for this case scenario? 6. Indicate the primary site, histology, and grade for each primary. Case Scenario 5 History & Physical 2/29/12 Patient is a 70-year-old white male with history of chronic lymphocytic leukemia (CLL) diagnosed in 2010. Patient has done well but blood work changed now and patient complains of just not feeling well including abdominal discomfort. Imaging 02/29/12 Abdomen/Pelvis x-ray: Bilateral renal masses present. These were not seen in the past. 04/04/12 PET scan: Intense areas of hypermetabolic activity corresponding to known bilateral renal masses. Left upper retroperitoneal lymphadenopathy identified, most likely malignant. Procedures 03/13/12 Right kidney mass biopsy: Diffuse large b-cell lymphoma 4/10/12 Bone marrow biopsy: Negative for lymphoma 1. Assign a histology code to each potential primary. 2. Assign a topography code to each potential primary. 3. Assign a grade code to each potential primary. 4. Apply the appropriate Hematopoietic Multiple Primary Rules to this case scenario. Indicate how many primaries this patient has and which rule was used to determine the number of primaries. 5. Which module should be used to determine the primary site and histology for this case scenario? 6. Indicate the primary site, histology, and grade for each primary. Case Scenario 6 History & Physical 5/1/12 Patient is a 67-year-ol black female diagnosed in 2007 with essential thrombocythemia and treated with Hydrea. Patient is seen now because of fatigue and bone pain. Splenomegaly identified on physical exam. On 12/4/09 the patient had a bone marrow biopsy showing primary myelofibrosis which the physician states is a transition from the essential thrombocythemia. Procedure 5/4/12 Bone marrow biopsy: Primary myelofibrosis. ADDENDUM: JAK2 gene mutation is present. Progress Note 5/11/12 Patient seen today to discuss bone marrow biopsy results. Diagnosis is primary myelofibrosis transformed from essential thrombocythemia. Patient will receive blood transfusion today. 1. Assign a histology code to each potential primary. 2. Assign a topography code to each potential primary. 3. Assign a grade code to each potential primary. 4. Apply the appropriate Hematopoietic Multiple Primary Rules to this case scenario. Indicate how many primaries this patient has and which rule was used to determine the number of primaries. 5. Indicate the primary site, histology, and grade for each primary.