Psychostimulants
advertisement

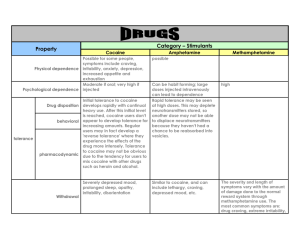
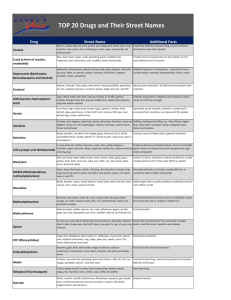
Psychostimulants Psychostimulants GPs and Psychostimulants • GPs are increasingly likely to see psychostimulant use • Most commonly used illicit drug after cannabis • GPs are well placed to identify, manage and minimise health problems that can arise from psychostimulant use. Psychostimulants Psychostimulants Defined • The term ‘psychostimulant’ describes a diverse range of naturally occurring and synthetically produced drugs • Also known as Amphetamine Type Stimulants (ATSs) • Main effect – stimulates CNS activity • Includes many commonly used substances/drugs • Each drug varies in strength and effect, although each has features in common • Most people have used a psychostimulant in the last 24 hours! Psychostimulants Psychostimulants May Be…. 1. Synthesised Compounds Pharmaceuticals Illicitly produced Pseudoephedrine Dexamphetamine Diethylpropion (Tenuate®) Methylphenidate (Ritalin®) Amphetamine sulphate i.e. speed Methamphetamine e.g. ice, meth, crystal Amphetamine-type substances e.g. MDMA (Ecstasy), PMA, MDA etc. 2. Naturally Occurring Compounds Tobacco (nicotine) Adrenaline Khat Cocoa (chocolate) Caffeine Cocaine Guarana Others... Psychostimulants Psychostimulant Forms (1) Common Form Chemical Composition Powder Amphetamine also called sulphate or speed, goey, methamphetamine whizz fast quick Appearance Cost ‘Route’ Administered Fine to $50-100 Snorted, crystallised /gram swallowed, coarse powder injected, shelved White-to yellow, orange or pink Crystal Methamphetamine ‘Crushed ice’ $50 also called hydrochloride large translucent /point ice to white crystals crystal or coarse meth powder Shabu, glass Smoked, snorted, swallowed, injected Psychostimulants Psychostimulant Forms (2) Common Form Chemical Composition ‘Base’ Free-base form of also called methamphetamine wax, paste, point, pure ‘Pills’ Appearance Cost Damp, sticky $30-50 / gluggy powder, ‘point’ paste oily yellow, red brown Dexamphetamine Tablets methylphenidate (Ritalin®), diethylpropion (Tenuate®) ‘Route’ Injected, swallowed, smoked, snorted $30-40 / Injected, tab (illicit swallowed supply) Psychostimulants Patterns of Use • Use tends to: – occur in social settings among diverse groups of people • Trends indicate psychostimulants are increasingly injected • Few patients will meet the criteria for dependence, however: – heavy users tend to use in a ‘binge’ pattern or a ‘run’ usually followed by a period of abstinence – heavy users are frequently polydrug users, with many using depressants to alleviate symptoms associated with the ‘come down’. Psychostimulants Pharmacology • Variable chemical compositions result in differences in pharmacological activity across psychostimulant types • Genetic differences in metabolism • Half life of psychostimulants differ: – amphetamine 12–36 hours – methamphetamine 8–17 hours – (ecstasy) MDMA 7–9 hours – cocaine 45–90 minutes. Psychostimulants Synaptic Activity Psychostimulants Meth/Amphetamine Effects: Onset and Duration Injection Intranasal Effect Intensity Swallowed Amphetamine 1 min 3min 60 min 6 hours 1 min 3min 20 min 30 min Cocaine Duration of effect Psychostimulants Amphetamine Effects Mild Feel good Alert Energy Confidence Sleeplessness Reduced appetite Dry mouth Moderate Feel great Increased libido Increased stamina No need for sleep Crash Suspicion Headache Teeth grinding Anxiety Toxic Extreme agitation Incoherence Increased temperature Dehydration Thought disorder Violent aggression Stroke Heart attack Psychostimulants Psychostimulant Cycle of Use Acquisition Administration Intoxication How and where can GPs assist in reducing harms? Cessation Crash / Withdrawal Intoxicated behaviour Psychostimulants Psychostimulants Psychostimulants Psychostimulants ‘Typical’ Pattern of Use Using Stopping Symptom Severity High Thought disorder Agitation Insomnia Suspicion Increased energy Feel good Exhaustion Depression Oversleeping Overeating No craving Low -7 0 Anhedonia Lack energy Anxiety Sleepless High craving 2 5 Flat mood Emotionally fragile Episodic craving to cues 15 20 25 30+ Days Pead, et al. (1996, p. 37) Psychostimulants Assessment Points • Occupation • Age • Social activities • AOD History – patterns of use, drug type, route, other drug use • Physical health (e.g. stability of weight) • Mental health (emotional lability, psychosis / paranoia) • Current level of intoxication / evidence of withdrawal • Laboratory investigations. Psychostimulants Courtesy of Dr. John Sherman, St. Kilda Medical Centre Psychostimulants Psychostimulants Courtesy of Dr. John Sherman, St. Kilda Medical Centre Psychostimulants Psychostimulants Management of Toxic Reactions Priorities are: • maintain airway, circulation, breathing • control elevated body temperature (hydration, cold water, ice) • control seizures (IV diazepam) • manage psychotic symptoms (antipsychotics) • reassurance, support, comfort, minimal stimulation. Treatment depends on patient’s condition on presentation. Psychostimulants Case Study Rory, a 24 year old student, presents with persistent headache, lethargy, and unexplained weight loss. He is ‘burning the candle at both ends’, working (in a bar) and studying, and states that ‘life is pretty hectic’ at present. Speed helps him get things done. Describe a brief intervention for Rory. Psychostimulants Psychostimulant Withdrawal Crash (Days 1–3) exhaustion depression oversleeping no cravings Peak symptoms (Days 2–10) dysphoria lack energy increased appetite generalised aches and pains re-emergence of mild psychotic features, including: misperceptions paranoid ideation hallucinations anxiety. Residual symptoms (from 1–8 weeks) episodic craving insomnia Fluctuating: irritability agitation restlessness dysphoria lethargy amotivation sleeplessness high craving From Pead et al. (1996, p. 84) Psychostimulants Withdrawal Treatment • Immediate withdrawal treatment – setting (home withdrawal, outpatient, or inpatient) – supportive environment, information and reassurance – provide ongoing monitoring – pharmacotherapies for symptomatic relief – plan long term management strategies • Planning for prolonged withdrawal – anticipate it will be prolonged (i.e. affecting sleep, mood, cravings) – plan for lapse and relapse – pharmacotherapies (short and long term) – prepare harm reduction strategies. Psychostimulants Pharmacotherapies For Psychostimulant Withdrawal • Aim to decrease discomfort • Benzodiazepines – assist sleep or reduce anxiety and agitation – avoid long term prescribing • Antidepressants – tricyclic antidepressants are generally not helpful – SSRI’s may be helpful but symptoms generally resolve within a week of withdrawal • Antipsychotics – available research shows limited efficacy. Psychostimulants Case Study Kylie, a 33 year old lawyer, recently discovered she was pregnant. She has an active work and social life, and consequently, tends to eat poorly. The pregnancy was unplanned. She is concerned about the health of her baby, and her lifestyle that precludes regular eating habits. How would you incorporate an AOD history into your consultation? What triggers may lead you to suspect psychostimulant use? Psychostimulants Cocaine • • • • • • Alkaloid from plant leaf of Erythroxylon coca Known as coke, charlie, snow, okey doke Sold in ‘lines’ CNS stimulant with local anaesthetic actions Also stimulates SNS Blocks reuptake of dopamine, noradrenaline and serotonin. Cocaine Crack Crack in vials Psychostimulants Cocaine: Patterns of Use People who use cocaine tend to: – be middle class, well educated professionals who snort – be injecting polydrug users, occasionally using ‘speedballs’ – use alcohol to enhance cocaine effects Patterns: – usually injected or snorted, occasionally smoked – ‘binge’ or a ‘run’ – bingeing patterns arise from rapid neuroadaptation. People who inject tend to use more often, use greater quantities than snorters, and are at Psychostimulants greater risk of harm. Cocaine: Pharmacology • Blocks reuptake of – dopamine (DA) – noradrenaline – serotonin • DA thought to be responsible for reinforcing effects • Interaction between cocaine and alcohol can produce toxic, if not fatal, effects. Psychostimulants Cocaine: Metabolism • Rapid onset of action (2–8 minutes respectively) • Peak blood levels occur in 5–30 minutes • Action is brief: – half-life of 15–30 minutes if injected – half-life of up to 30 minutes if snorted • Metabolised by liver, 1–2% excreted unchanged in urine • Inactive metabolites can be detected in: – blood or urine for 24–36 hours after use – hair for weeks to months after use. Psychostimulants Cocaine: Acute Effects Desired Acute low dose Euphoria Sociable/gregarious, talkative Confidence, control, energy Reduced need for sleep Temporary increase in functional activity/ efficiency Acute high dose (Overdose) Local anaesthesia Dilated pupils Vasoconstriction Increased respiration, pulse, BP, temperature Stereotyped, repetitive behaviour Anxiety, panic Aggression, hostility Cardiovascular events (e.g. arrythmias, MI) Neurological events (CVA, seizures, blurred vision, dizziness, headache) Psychological events (hallucinations, confusion) Stomach pain, nausea Psychostimulants Cocaine: Chronic Effects • Insomnia • Depression, anxiety • Aggression, violence • Loss of appetite, concomitant weight loss • Muscle twitching • Psychosis – paranoid delusions, hallucinations • Loss of libido / impotence • Heightened reflexes • Increased pulse rate. Psychostimulants Cocaine: Symptoms of Withdrawal • Dysphoria (rather than depression) which may persist (up to 10 weeks). Plus at least two of: – fatigue – insomnia / hypersomnia – psychomotor agitation – craving – increased appetite – vivid unpleasant dreams • Withdrawal tends to peak 2–4 days following cessation of use. Psychostimulants Cocaine: Withdrawal Management • Non-stimulating/non-threatening environment • Possible suicide precautions • To date, no effective pharmacotherapies for withdrawal management • Prescribed medications: – short term use of benzodiazepines (anxiety, agitation, promote sleep) – antidepressants (SSRIs; though continued cocaine use may precipitate toxic reactions). Psychostimulants Cocaine: Problems Associated with Use Physical • Nasal – e.g. rhinorrhoea, epistaxis, ulcers, sinusitis, perforated nasal septum, risk of HCV transmission through sharing snorting and injecting equipment • IDU – e.g. systemic / local infections, vein problems (abscess, cellulitis, phlebitis), bacterial endocarditis, BBV transmission • Cardiovascular complications • Death. Psychosocial • Interpersonal (relationship discord, paranoia – irrational jealousy, alienation) • Occupational (absenteeism, job or productivity loss) • Financial • Legal. Psychostimulants Psychostimulant Interventions (1) • Be non-judgmental, do not insist on abstinence • Engage and retain patient in treatment • Understand patient’s treatment goals • Tailor intervention to suit patient, including level and intensity of referrals • Offer flexible service delivery, consistent with a patient’s changing goals and needs • Provide psychosocial support • Address concurrent mental health needs; e.g. anxiety, bipolar, or attention deficit disorders are common with cocaine use. Psychostimulants Psychostimulant Interventions (2) • Behavioural and psychosocial therapies produce better results than pharmacotherapies • Cognitive-Behavioural Therapy (CBT) helps the patient develop problem solving skills and strategies to: – identify high-risk situations – identify functional drug use – deal with cravings • CBT is more effective and longer lasting than less intensive strategies. Psychostimulants