1,65
advertisement

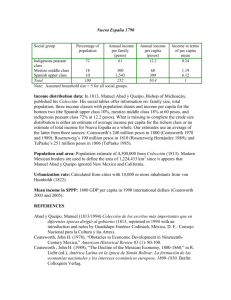
II Jornades SOHIB ¿Se puede mejorar la estimación del riesgo cardiovascular con información Genètica? Jaume Marrugat Research Group on Cardiovascular Epidemiology & Genetics, Program of Research on Imflamatory & Cardiovascular Disorders, IMIM, Barcelona, Spain. Spanish Cardiovascular Research Network HERACLES (RETICS-ISCIII) Justification of primary prevention of coronary heart disease • Greatest cause of death in developed countries. In ~35% of cases its onset symptom is sudden death. • Most cases are related to lifestyle & other modifiable factors, whose improvement results in reduced CHD incidence. Cumulative incidence of CVD adjusted for the competing risk of death for men and women according to aggregate risk factor burden at 50 years of age, in the Framingham Heart Study ≥ 2 risk factors 1 major risk factor ≥ 1 increased risk factor ≥ 1 suboptimal risk factor All risk factors optimal Adjusted Cumulated Incidence 0,7 0,6 69% Men 0,5 Women 50% 50% 46% 0,4 36% 39% 0,3 0,2 0,1 <3% a Framingham i 10% a Girona 5% 0 50 60 70 80 90 50 Attained age Lloyd Jones.Circulation. 2006;791-798 60 70 80 90 8% Changes in population LDL & HDL cholesterol 1995-2005 FEMALE 0.012 0.012 MALE 1995 (mode=133.3) 2000 (mode=142.4) 2005 (mode=131.1) density density 0.008 0.008 1995 (mode=151.6) 2000 (mode=148.5) 2005 (mode=126.8) p-value<0.001 0.000 0.000 0.004 0.004 p-value<0.001 0 50 100 150 200 250 300 350 0 50 100 LDL cholesterol (mg/dL) MALE 0.040 200 250 300 350 LDL cholesterol (mg/dL) FEMALE 1995 (mode=51.6) 2000 (mode=50.1) 2005 (mode=55.9) 0.020 p-value=0.351 0.010 0.010 p-value=0.644 density 0.020 0.030 0.030 1995 (mode=42.3) 2000 (mode=44.1) 2005 (mode=44.7) 0.000 0.000 density 150 10 30 50 70 HDL cholesterol (mg/dL) 90 110 10 30 50 70 HDL cholesterol (mg/dL) 90 110 Grau M & REGICOR Inv. Eur J Cardiovasc Prev Rehabil. 2007. 14: 653-9. Girona population aged 35-74 years Población de Girona de 35-74 años 1995 2005 Hombres n=1748 n=4458 p-trend HTA Conocida HTA Total HTA Tratada HTA Bien controlada 20% 45% 37% 15% 30% 44% 45% 38% 0,01 NS 0,018 0,011 Mujeres HTA Conocida HTA Total HTA Tratada HTA Bien controlada 22% 39% 38% 22% 26% 35% 47% 45% 0,002 NS 0,018 0,011 Grau M & REGICOR Inv. Eur J Cardiovasc Prev Rehabil. 2007. 14: 653-9. Cambios en la prevalencia de hipertensión arterial 1995-2005 30 Trends in MI incidence rates in the population aged 35 to 74 years i Gerona 1990-2003 Atack rate men Atack rate women 300 250 200 150 100 50 0 Gil M REGICOR. Rev Esp Cardiol 2007-60-349. Disease prevention Screening POPULATION Population Genetic Characteristics individuals Patients Risk Factors Primordial prevention Disease Primary Prevention Inappropriate Life Styles Patients Reccurrences Secondary Prevention Population distribution of total cholesterol Japan Finland CHD CHD 190 230 mg/dL Population distribution of total cholesterol & CHD incidence CHD incidence CHD incidence 200 220 mg/dL Population & MI patient distribution of total cholesterol in high incidence countries Population MI patients 200 mg/dL 220 Homes Dones REGICOR adaptada versió 2010 The ideal risk function… Braunwald, JACC 2006 Many events Highest High Risk Intermediate Lesser # of events Low CHD risk, and 10-year CHD event incidence in the REGICOR population cohort (n=3200) Incidencia Población % Casos 60 50 Porcentaje 40 30 20 10 0 <5% 5-9,9% 10-14,9% Riesgo REGICOR 15-20% 20% - CHD risk, and 5-year CHD event incidence in the primary care VERIFICA cohort (n=4500) Incidencia Población % Casos 60 50 Porcentaje 40 30 20 10 0 <2,5% 2,5-4,9% 5-7,6% Riesgo REGICOR 7,7-9,9% 10% - Low CVD risk Stimulate healthy lifestyles, appropriate weight and follow-up Moderate High Intensive intervention on risk factors What else can be done in XXIst century? No risk factor reaches individually the ideal AUC …so we combine factors… …that are usually correlated among them Libby P. EHJ 2010; 31: 777 Risk modifiers influence atherogenesis through effects on inflammation as reflected by biomarkers of the acute phase response Potential biomarkers in CV diseases • The 22 more abundant proteins, including albumin & immunoglobulins, constitute 99% of the plasmatic proteome mass. • Many biologically interesting molecules circulate in very small concentrations: – Troponin: – Insulin: – TNF: nanomolar (10-6) concentration picomolar (10-9) concentration femtomolar (10-12) concentration Anderson, N. L. et al. The human plasma proteome: a nonredundant list developed by combination of four separate sources. Mol. Cell. Proteomics 3, 311–326 (2004). Biomarkers Plasma: >2x104 >2x104 Anderson, N. L. et al. Mol. Cell. Proteomics 3, 311–326 (2004). >3x105 Área bajo la curva de muerte o eventos CV mayorescon factores emergentes. Proteína C reactive; Péptido natriurético B, Péptido natriurético N-terminal pro–auricular, aldosteronemia sérica,renina plasmática; fibrinógeno; inhibidor del activador del plasminogeno tipo 1; Dimero D; homocisteína; y el cociente albumina en orina / creatinina. Reclassification • Recently some researchers proposed level of reclassification as a measure of added utility: Net Reclassification Improvement* • They categorized individuals into meaningful CHDrisk categories (say <5%, 5-10%, 10-15%,>15%) based on risks predicted using models with and without the new marker and measured the amount of “reshuffling”. •*Cook, Circulation 2007. Steyerberg et al Epidemiology 2010; 21:128-38 Adjusted AUC for different models with traditional risk factors and CIMT in ARIC Study AUC area under the curve; CI confidence interval; CIMT carotid intima-media thickness; TRF traditional risk factors. Nambi et al. JACC . 2010; 55: 1600-7 Number and % reclassification with CIMT and plaque information are added to traditional risk prediction models in ARIC Study Reclassification Overall sample Men Women Nambi et al. JACC 2010; 55: 1600-7 Overall NRI 9.9% 8.9% 9.8% Clinical NRI (5-10 10-20 or 10-20 >20%) 21.7% 16.4% 25.4% Some informative non-invasive tests • Ultrasound carotid intima media thickness (IMT). • Ankle brachial index is inexpensive, easy-tomeasure with some training. C-IMT & ABI do not indicate increased CVD risk … but existing disease! IMT Estenosis Possible factors for the reclassification of candidates to CVD primary prevention • • • • • • • HS C reactive Protein > 1g/l, Family history of early ECV, Obesity (BMI > 30), or waist > recommended values, Microalbuminuria or renal failure, Inappropriate diet (self-administered short questionnaire) Insufficient exercise (self-administered short questionnaire) Adverse genetic profile (predisposition/genetic burden), • Carotid IMT • Feeble/undetectable paedial pulse or ABI<0.9 Preclinical disease Heritability (h2) • The proportion of total phenotypic variance that is explained by genetic variance at the population level. MYOCARDIAL INFARCTION: h2 = 0.56. (Nora JJ, et al. Circulation 1980;61:503-8.) CORONARY HEART DISEASE MORTALITY: h2 =0.53-0.57 (Zdravkovic S, et al. J Intern Med 2002;252:247-54. Wienke A, et al. Twin Res 2001;4:26674.) CAROTID ARTERIOSCLEROSIS: h2 = 0.09-0.67 (Xiang AH, et al. Arterioscler Thromb Vasc Biol 2002;22:843-8; Fox CS, et al. Stroke. 2003;34:397-401; Juo SH, et al. Stroke 2004;35:2243-7; Swan L, et al. Atherosclerosis 2003;166:137-41; North KE, et al. Arterioscler Thromb Vasc Biol 2002;22:1698-703; Hunt KJ, et al. Stroke 2002;33:2775-80.) INTROCORONARY CALCIUM: h2 = 0.42 (Peyser PA, et al. Circulation 2002;106:304-8.) Coronary heart disease: Complex disease • Polygenic: different loci/genes are defining the individual susceptibility. • Allelic heterogeneity: different variants in each locus/gene are defining the individual susceptibility. • Gen-gen interactions. • Environment-environment interactions • Gen-environment interactions New variants for MI or CAD via GWAS Myocardial Infarction Genetics Consortium 32 Allelic dosage and MI risk 3 p=2x10-18 2,23 2 OR 1,69 1 1,43 1,22 1.00 0 1 2 3 4 Allelic dosage quintiles (9 SNPs) MIGen Consortium. Nat Gen 2009;41:334-41. 5 Graphic CV risk representation (35 to 74 y) by REGICOR risk function with CRF and with CAD genetics alone Average 10-year CV risk Riesgo de IAM a 10 años (%) 50% REGICOR/Genetica Genetic risc+smoking+hypertension+dyslipaemia 45% -Tabaquismo REGICOR/Genetica Genetic risc+hypertension+dyslipaemia -Tabaquismo - HTA REGICOR/Genetica Genetic risc+dyslipaemia 40% -Tabaquismo - HTA - Hipercolesterolemia REGICOR/Genetica Genetic risc alone 35% 30% 25% 20% 15% 10% 5% 0% 35 40 50 45 55 60 65 70 edad (años) Age (years) J P J P exp β CRFp *CRFp,i βSNPj *SNPj,i β CRFp *CR FP βSNPj *SNPj j1 p1 j1 p1 prob(event i | CRFp,i , SNPj,i ) 1 S • Proof of concept—Do novel genetic markers, non associated with classical risk factors, differ between subjects with and without CHD? • In silico case-control study: on the Wellcome Trust Case Control Consortium public data • Prospective validation—Incremental value: • Cohort studies: • REGICOR • Framingham •… Distribution of the number of risk alleles in cases and controls Distribution of the number of alleles in CHD cases and controls Number of risk alleles in the 9 variants of interest (0 to 18 alleles) OR per allele = 1.18 Lluis-Ganella C…Elosua R. REC 2010 (in press) Odds ratio for the cumulated number of MI risk alleles 7 alleles is the median (and reference group) Alleles # Controls # Cases OR (95% IC) Lluis-Ganella C…Elosua R. REC 2010 (in press) P value Odds ratio for CHD across genetic score quintiles Genetic score quintiles Alleles # Controls # Cases Lluis-Ganella C…Elosua R. REC 2010 (in press) OR (95% IC) P value Comparison of the effect (OR) of quintiles of the cumulated # of adverse alleles with that of total cholesterol Total Cholesterol < 160 (7%) 160-199 (17%) 200-239 (38%) 240-279 (26%) >=280 (12%) Q5 vs. Q1 OR 0,52 1 1,20 1,65 1,93 3,74 1 1,21 1,40 1,88 2,20 2,20 Quintiles OR Lluis-Ganella C…Elosua R. REC 2010 (in press) Comparison of the effect (OR) of quintiles of the cumulated # of adverse alleles with that of hypertension PA OR Optimal Normal HT grade I (28%) HT grade II-III (13%) Q5 vs. Q1 (20%) Normal High (18%) (21%) 1 1 1,32 1,68 1,86 1,86 1 1,21 1,40 1,88 2,20 2,20 Quintiles OR Lluis-Ganella C…Elosua R. REC 2010 (in press) • Proof of concept—Do novel genetic markers, non associated with classical risk factors, differ between subjects with and without CHD? • In silico case-control study: on the Wellcome Trust Case Control Consortium public data No improvement in c-statistics (AUC). • Prospective validation—Incremental value: Significant • Cohort studies:improvement in reclassification • REGICOR • Framingham •… NRI: 15.2 % Some advantatges of determining the cardiovascular risk genotype over other biomarkers Genetic characteristics : • Does not change with age or sex • Does not change with food • Does not change with drugs • Does not have intra-individual variability • Need to determined only once in life (or until new markers are found) CHD/CVD screening • Population • Individuals • Individuals • Patients • Patients Risk charts: screening basic system First level of Reclassification Biomarkers Genetic predisposition Second level of reclassification Exercise test, ABI, C-IMT Non-invasive angiography Diagnostic Confirmation Coronary angiography PCI / other revascularization RI Imaging Biomarkers, Genetic risk Preclinical disease: IMT-c & ABI CVD SK Simplified figure for potential use of emerging risk factors and imaging techniques in CV primary prevention Classical Risk Factors Low <5% 10-year CVD Risk REGICOR Promoting healthy life-styles and appropriate BMI. Follow-up / 5 years Interme diate 5-10% >1 additional tests† High >10% >1 additional tests † † HS C reactive Protein > 1g/l, Family history of ECV prematura, Carotid IMT, Feeble/undetectable paedial pulse or ABI<0.9, Obesity (BMI > 30), or waist > recommended values, Microalbuminuria or renal failure, Inappropriate diet, Insufficient exercise Adverse genetic profile (once in a life span) Intensive intervention on risk factors. Annual follow-up Non-invasive coronary angiography for vulnerable plaque* Treatment of lesions Very high risk Coronary angiography Exercise test Assymptomatic population with no CVD history Extremely high risk WWW.REGICOR.ORG Number/1,000 <= 2.4 2.4 to 4.8 4.8 to 7.2 7.2 to 9.6 9.6 to 12.0 No data STANDARDISED CARDIOVASCULAR MORTALITY ~ 2004 MEN ESC Report Cardiovascular Diseases in Europe 2006. WHO data; June 2006. Positive remodeling (+), Soft plaque (+), Fibrous plaque (+), Calcification (-) Coronary angiography LAD Tomografía computerizada multicorte con multidetectores Motoyama et al. ACC 2006 Clarifying Uncertainity • Non-invasive tests – Coronary Calcium score (CT) increases with age, low predictive capacity, – Magnetic Ressonance Limited resolution expensive – CT MD expensive, high irradiation, but promising… Standardized CAD mortality rates in Europe (1995-2002) Fed. Rusa Lithuania Bulgaria Rep. Checa Hungría Rumanía Polonia Finlandia Irlanda Cuba Estados Unidos Reino Unido Alemania Suecia Austria Men 2002 Noruega Men 1995 Canadá Grecia Holanda Italia Suiza Luxemburgo Portugal España Argentina Chile Francia Mortality / 100.000 Japón 0 100 200 300 400 500 600 World Health Statistics. World Health Organization. Geneve, 2000. (versión on-line en http://www.who.int/ncd_surveillance/infobase/web/InfoBasePolicyMaker/Reports/). Incidence & mortality of CHD in men (x100.000) and levels oxidized LDL (U/L) adjusted for triglyceride, in chronic CHD men, in Europe. South Helsinki N=125 Estocolmo N=133 800 700 600 500 Ausburgo N=159 Barcelona N=135 Central North 70 Oxidized LDL Incidence (x100.000) Mortality (x100.000) 68 66 64 62 400 60 Roma N=12 4 300 200 Atenas N=120 Grau M, Marrugat J; AIRGENE Study Group European Heart Journal 2007; doi: 10.1093/eurheartj/ehm446 58 56 100 54 0 52 Ecological analyses of IMTmean vs. coronary heart disease mortality in Europe D. Baldassarre et al. IMPROVE Study JACC 2010. doi:10.1016/j.jacc.2009.11.075 25-year CHD mortality in the 7-Countries Study by cholesterol levels in different world areas 30 Northern Europe CHD mortality rate, % 25 USA 20 15 10 Southern continental Europe Serbia Southern Mediterranean Europe 5 Japan 0 2,6 (100mg/dl) 5,15 (200mg/dl) Kromhout D. Eur Heart Journal 1999; 20: 796-802. 7,75 (300mg/dl) Colesterolemia total, mmol/ l 25-year mortalirty risk Diagram of the effect of cholesterol on CHD mortality risk by regions. 20 18 16 14 12 10 8 6 4 2 0 RR=1,7 Anglo-saxon Mediterranean RR=1,7 <200 200-239 240-300 Total Cholesterol >300 mg/dL 25-year mortalirty risk Diagram of the effect of cholesterol on CHD mortality risk by regions. 20 18 16 14 12 10 8 6 4 2 0 Anglo-saxon Mediterranean Absolute difference of risk among regions <200 Kromhout D. Eur Heart Journal 1999; 20: 796-802. 200-239 240-300 Total Cholesterol >300 mg/dL Framingham function over-estimation of the 10-year CHD-event risk in Girona WOMEN MEN Estimateds/observed ratio 5 After calibration 4 3 Women 2 Men 5 0 35-44 y 45-54 y 55-64 y 65-74 y Age Group Estimated/observed rate 1 4 3 2 1 0 35-44 y 45-54 y 55-64 y Age group Marrugat et al. J Epidemiol Comm Health 2003;57:1-6. 65-74 y <3% of population Many “false Positive” CCS Sensitivity of 98% & Specifity of 27% for CCS>0 to predict CAD events at 37 months in men aged ~52 years CIMT Sensitivity of 96% & Specificity of 49% for CIMT>0.55mm to predict CAD in men/women aged ~62 years. Kondos GT. Circulation 2003;107:2571-2576. Belhassen L. J Am Coll Cardiol, 2002; 39:1139-1144 1: No history of angina, heart attack, stroke, or peripheral arterial disease. 2: Population over age 75y is considered high risk and must receive therapy without testing for atherosclerosis. 3: Must not have any of the following: Chol>200 mg/dl, blood pressure >120/80 mmHg, diabetes, smoking, family history, metabolic syndrome. 4: Pending the development of standard practice guidelines. 5: High cholesterol, high blood pressure, diabetes, smoking, family history, metabolic syndrome. 6: For stroke prevention, follow existing guidelines. HTA Newton-Cheh C et al. Nat Genet. 2009 May 10. HTA Newton-Cheh C et al. Nat Genet. 2009 May 10. Heredabilidad de diferentes fenotipos relacionados con arteriosclerosis INFARTO AGUDO DE MIOCARDIO: h2 = 0.56. (Nora JJ, et al. Circulation 1980;61:503-8.) MORTALIDAD POR CARDIOPATÍA ISQUÉMICA: h2 =0.53-0.57 (Zdravkovic S, et al. J Intern Med 2002;252:247-54. Wienke A, et al. Twin Res 2001;4:266-74.) ARTERIOSCLEROSIS CAROTIDEA: h2 = 0.09-0.67 (Xiang AH, et al. Arterioscler Thromb Vasc Biol 2002;22:843-8; Fox CS, et al. Stroke. 2003;34:397-401; Juo SH, et al. Stroke 2004;35:2243-7; Swan L, et al. Atherosclerosis 2003;166:137-41; North KE, et al. Arterioscler Thromb Vasc Biol 2002;22:1698-703; Hunt KJ, et al. Stroke 2002;33:2775-80.) CALCIO INTRACORONARIO: h2 = 0.42 (Peyser PA, et al. Circulation 2002;106:304-8.) Validación de los 9 marcadores genéticos de riesgo coronario independientes de los factores de riesgo cardiovascular • Primera Fase: Validación de un chip diagnóstico para analizar el riesgo coronario: • Estudio caso-control: in silico en la base de datos pública del Welcome Trust Consortium (WTCCC) • Segunda fase: Validación de la capacidad predictiva de los marcadores incluidos en el chip: • Estudios de cohorte: • REGICOR • PROCAM • Framingham (in silico) Los 9 genes de riesgo coronario INDEPENDIENTES de los factores de riesgo cardiovascular SNP Cromoso ma Alelo de riesgo Alelo raro Frecuencia alelo raro OR (por copia alelo de riesgo) Beta de alelo raro rs1333049 9 C C 0,47 1,35 0,30010 rs602633* 1 C A 0,23 1,18 -0,16551 rs17465637 1 C A 0,28 1,13 -0,12222 rs501120 10 T C 0,13 1,19 -0,17395 rs1515098* 2 T C 0,34 1,21 -0,19062 rs1474787* 6 A A 0,25 1,23 0,20701 rs9982601 21 T T 0,13 1,20 0.1823 rs12526453 6 C G 0.45 1,12 -0,1133 rs6725887 2 C C 0,14 1,17 0,1570 rs9818870 3 T T 0.17 1,15 0,1398 rs3184504 12 T T 0.38 1,13 0,1222 * rs602633, rs1515098 y rs1474787 se encuentran en desequilibrio de ligamiento con rs599839, rs2943634 y rs6922269, respectivamente. Comparación de la OR del # de alelos adversos con la de los niveles de colesterol total Colesterol < 160 (7%) 160199 (17%) 200239 (38%) 240279 (26%) >=280 (12%) -- -- -- OR 0,52 1 1,20 1,65 1,93 Nº Alelos 4 (5%) 5 (11%) 6 (16%) 7 (20%) 8 (21%) 9 (14%) 10 (8%) 11 (5%) OR 0,70 0,74 0,92 1 1,16 1,54 1,65 2,09 Extremos 3,74 3,00 Comparación de la OR del # de alelos adversos con la de los niveles de HTA PA (20%) NAlta (18%) (28%) HTA II-III (13%) 1 1 1,32 1,68 1,86 Nº Alelos 4 (5%) 5 (11%) 6 (16%) 7 (20%) 8 (21%) 9 (14%) 10 (8%) 11 (5%) OR 0,70 0,74 0,92 1 1,16 1,54 1,65 2,09 OR Optima N (21%) HTA I -- -- -- Extremo 1,86 3,00