Chapter 22 The Lymphatic System, Nonspecific Resistance to Disease
advertisement

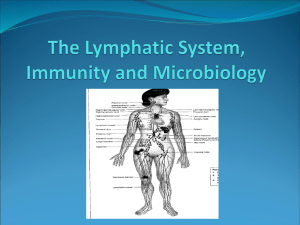
Chapter 22 The Lymphatic and Immune Systems The Lymphatic System Basic organization Lymph fluid in lymph vessels Structures, organs w/ lymph tissue, red bone marrow Functions drain interstitial fluid and proteins transport dietary fats protect against invasion resistance - fight off disease nonspecific resistance - general protection against disease immunity - specific protection susceptibility - lack of resistance Lymphatic Vessels Lymphatic capillaries Blind ended vessels between cells, larger than blood capillaries Not in avascular tissues, CNS, splenic pulp, bone marrow Lymphatic Capillaries Structure/Function regulates fluid flow Anchoring filaments - from lymphatic endothelium attach to surrounding tissues Endothelial cells overlap high hydrostatic fluid pressure separates cells, fluid into caps hydrostatic fluid pressure in cap prevents fluid movement out The Lymphatic System Lymph flow follows venous circulation Lymph vessels have same organization as vascular tree Smaller vessels drain into larger vessels The Lymphatic System (cont.) Lymph returns to venous blood through R,L lymphatic ducts Enter at internal jugular and subclavian veins The Lymphatic System Lymph ducts Right lymphatic duct about ½ inch long drains lymph from upper right side of body Thoracic (left) duct main collecting duct of lymph system 38-45 cm long drains 75% of body begins as a dilation known as cisterna chyli located anterior to lumbar disk #2 The Lymphatic System Flow of Lymph More fluid out of blood capillaries by filtration than returns by absorption - Starling’s Law 3Ll day of lymph fluid Proteins from blood returned by lymphatics Lymph flow by muscle pump, respiratory pump, valves Lymphatic Tissue - General 1º lymphatic organs - site of B and T cell production bone marrow - produces B cells, pre-T cells thymus gland - migrate to thymus gland 2 º lymphatic organs site of most immune responses lymph nodes, spleen – surrounded by connective tissue capsule lymphatic nodules – not surrounded by capsule Thymus Gland Thymus Gland Between sternum, heart 2 lobes Atrophies w/ age Structure/Function Outer cortex pre-T cells migrate to thymus proliferation Maturation dendritic cells macrophages Inner medulla – more of the same Lymph Nodes Lymph Node Structure oval, bean shaped structures along lymph vessels may be deep or superficial scattered throughout body concentrated in mammary glands, axillae, groin filter lymph fluid Lymph Nodes Connective tissue capsule w/ trabeculae extending into cortex Stroma -supportive network of reticular fibers, fibroblasts Lymph Nodes Parenchyma Outer cortex lymphatic nodules inner germinal center site of B-cell proliferation Site of B-cell maturation and plasma cell formation Inner medulla medullary cords of lymphycytes, macrophages, plasma cells Cortex Medulla Lymphatic Tissue - Specific Node fluid flow Enter cortex through afferent vessels Filter, remove damaged cells, microorganisms, foreign substances by reticular fibers macrophages phagocytize some, lymphocytes destroy others exit medulla from hilus by efferent vessels Metastasis cancer cells from tumor trapped in lymph nodes Lymph Nodes Histology Lymphatic Tissue - Specific Spleen largest mass of lymphoid tissue in body Left side of body between stomach/diaphragm thick fibrous capsule w/ artery, vein, efferent lymph vessel organ function: immune function removal of worn out, damaged RBC’s storage of platelets production of RBC’s during fetal life Lymphatic Tissue - Specific Lymphatic nodules (tonsils) oval-shaped nonencapsulated groups of lymphatic tissue scattered in mucous membranes, GI tract, respiratory tract, urinary tract, reproductive tract protect against invasion of inhaled or ingested foreign substances Nonspecific Resistance to Disease Summarized in Table 22.1 Surface Barrier – Skin and mucosa Internal Defenses 1) 2) 3) 4) Antimicrobial proteins Natural killer cells and Phagocytosis Inflammation Fever Nonspecific Resistance to Disease Surface Barrier – Skin and mucosa Mechanical protection intact epidermis mucous membranes line body cavities, mucus prevents drying, traps foreign bodies nose hairs, respiratory tract cilia lacrimal apparatus saliva - dilute microbes, wash them from teeth surface urine flow, vaginal secretions – flow and pH help kill microorganisms defecation and vomiting - expel microbes Nonspecific Resistance to Disease Surface Barrier – Skin and mucosa Chemical protection Skin sebum (unsaturated FA’s) forms layer, prevents bacterial growth perspiration has fatty acids, lo pH lysozyme - enzyme breaks down bacterial walls gastric juice - stomach nearly sterile due to lo pH, 2ish Nonspecific Resistance to Disease 1) Antimicrobial substances produced against pathogens that penetrate 1º defense A. Interferons Released from infected cells Stimulate production of antiviral proteins from neighboring cells B. Complement system 20 plasma and cell membrane proteins Function to complement (enhance) certain immune, allergic and inflammatory systems C. Transferrins – inhabit bacterial growth by binding iron Nonspecific Resistance to Disease 2) Natural killer (NK) cells and phagocytosis NK nonspecific killers that respond before immune system is activated ability to kill virus infected body cells and some tumor cells by poking holes in cells and stimulating cell death Nonspecific Resistance to Disease 2) Natural killer (NK) cells and phagocytosis Phagocytosis ingestion of microbes or foreign material by phagocytes 2 kinds of phagocytosis - neutrophils and macrophages steps chemotaxis adherence ingestion digestion killing Nonspecific Resistance to Disease 3) Inflammation 4 symptoms: Redness Pain Heat Swelling 3 steps in process 1. Vasodilation/increased vessel permeability 2. Phagocyte migration 3. Tissue repair Nonspecific Resistance to Disease Step 1. Vasodilation and increased vessel permeability Release of factors from leukocytes stimulate vascular changes Histamine, kinins, prostaglandins, leukotrienes Vasodilate, increase permeability, stimulate emigration and chemotaxis Cause heat, redness and swelling Nonspecific Resistance to Disease Step 2. Phagocyte migration leukocytosis-inducing factors chemotaxis Emigration neutrophils - rapid monocytes - slower Nonspecific Resistance to Disease Step 3. Tissue repair Tissue regrowth and repair of damage Pus dead phagocytes, damaged tissue if too numerous for easy removal may form abscess Nonspecific Resistance to Disease 4) Fever increase effects of antimicrobial substances inhibits some microbes increase rate of body repair Nonspecific Resistance to Disease Surface Barrier – Skin and mucosa Internal Defenses 1) 2) 3) 4) Antimicrobial proteins Natural killer cells and Phagocytosis Inflammation Fever Immunity Immunity ability of body to defend itself against specific invaders specificity and memory differentiate this from non-specific system two types Humoral (antibody mediated) immunity Cellular (cell mediated) immunity Antigens Antigen - substances that provoke immune response Epitope antigen part that triggers immune response most antigens have many epitopes Antigens (cont.) Chemical nature of antigens large, complex molecules mostly proteins, nucleo-, lipo-, glycosmaller substances may be incomplete antigens hapten react with antibodies but not cause immune response poison ivy toxin usually foreign substances Antigens (cont.) Antigen receptor diversity >1 billion different epitopes recognized by body diversity - genetic recombination, shuffle, reorganize different genes Major Histocompatibility Complex antigens (MHC) unique to each individuals cells, help in identifying foreign bodies 2 classes of MHC antigens class I MHC - all body cells but RBC's class II MHC - only on antigen presenting cells (APC’s), thymus cells, activated T cells Pathways of Antigen Processing For immune response to occur, B and T cells must recognize foreign antigen B cells can recognize, bind to antigens in ECF, blood, lymph T cells only recognize antigen protein fragments presented w/ MHC self-antigens - good/bad proteins Pathways of Antigen Processing During protein digestion and production in cell, small peptides used to stabilize MHC proteins if peptides from normal body cells, no response if peptides from antigens T cells recognize them immune response! preparation of foreign antigen for cell surface known as processing and presenting of antigen Antigen Presenting Cell's (APC’s) macrophages, activated B cells, dendritic cells process exogenous antigens present them w/ MHC class II molecules to T cells Pathways of Antigen Processing Processing of exogenous antigen – produced outside cell 1) 2) 3) 4) 5) phagocytosis/endocytosis digestion vesicles fuse, peptide fragments bind to MHC-II’s exocytosis to membrane move to lymphatic tissue, present antigen to T-cells Pathways of Antigen Processing Processing of endogenous antigen – produced within body cells viral proteins from viral infection of cell produced, incorporated into MHC-I molecules during normal cell growth put on surface of cell identifies cell as infected, signals that cell needs help T and B cell formation Both B and T cells produced from stem cells in bone marrow Development of immunocompetence occurs in different sites B cells complete maturation in Bone marrow Pre-T cells move to Thymus - complete maturation in thymus Immunity - General Before mature cells leave home: both types acquire surface proteins - antigen receptors T cells exit as CD4+ or CD8+ cells w/ different functions CD4+ cells become helper T cells Immunity - General 2 Types of immune responses Cell-mediated immunity Antibodymediated immunity General Initial activation of Helper T cells Helper T cells aid both types of immune responses Pathogens often activate both types of responses Immunity - General 1) Cell-mediated immune (CMI) responses CD8+ cells change into killer T cells with aid from Helper T cells directly attack infecting antigen Effective against: intracellular pathogens some cancer cells foreign tissue transplants Immunity - General 2) Antibodymediated immune (AMI) responses B cells transform into plasma cells with aid of Helper T cells synthesize, secrete specific proteins (antibodies or immunoglobulins) antibodies bind and inactivate antigens Effective against: antigens in body fluids EC pathogens (bacteria) Cell -Mediated Immunity Basic steps 1. Recognition of APC antigen by T cell receptors (TCR’s) – first signal 2. Costimulation for activation 3. Proliferation and differentiation 4. Clone effector cells capable of recognizing initial activator (antigen) 5. Elimination of intruder Cell-Mediated Immunity (cont.) T cell recognition, proliferation, differentiation APC presents antigen TC’s recognize, bind foreign antigen millions of T cells each specific for 1 antigen Need co-stimulator 20 known, cytokines, interleukins, needed for full immune response prevent false activation? Cell-Mediated Immunity (cont.) T cell enlarges, makes clones capable of recognizing antigen Cell-Mediated Immunity (cont.) Clones Helper T (TH) cells - CD4+ after costimulation helpers secrete co-stimulators co-stimulates helper T cells, cytotoxic T cells, B cells Cytotoxic T (TC) cells - CD8+ recognize antigen fragments associated w/ MHC-I molecules, some tumor cells and tissue transplant cells become cytolytic need stimulators from helper T cells Cell-Mediated Immunity (cont.) Tc elimination of invaders 1. Migrate from lymph to infection site 2. Recognize, attach to target antigen/cell 3. Kill invaders 4. Detach, seek out another invader w/ proper antigen Cell-Mediated Immunity (cont.) More Clones Suppressor T (TS) cells produced with other clones downregulate immune system by producing other cytokines Memory T (TM) cells recognize original invading antigen second response rapid due to large numbers of TM cells present Antibody-Mediated Immunity Body contains millions of B cells located in lymphoid tissue each responds to specific antigen Become activated in presence of foreign antigen unprocessed antigen weak response need to process antigen for stronger response Antibody-Mediated Immunity Unprocessed antigen taken into cell incorporated into MHC-II self-antigen activates helper T cells Costimulation production of cytokines Antibody-Mediated Immunity Some B cells change into plasma cells secrete specific antibodies, at high rate for 4-5 days antibodies circulate in lymph and blood to site of invasion Circulating antibodies combine w/ antigens neutralizes antigen immobilizes bacteria agglutinating (clumping) antigens activates complement system enhances chance antigen will be phagocytized Antibody-Mediated Immunity Activated B cells some turn into memory B cells respond more rapidly, forcefully if antigen appears again Antibodies Antibodies (Abs) Globulins (proteins) specific for antigenic determinant of antigen that triggered its production 5 different classes - IgG, IgA, IgM, IgD, IgE Immunological Memory Long lived antibodies and lymphocytes arise during activation of antigen-stimulated B, T cells Immunization possible because memory B cells and memory T cells remain after 1º response w/ secondary exposure system responds more quickly, forcefully secondary response - antibodies produced during second exposure have a higher attraction for antigen Acquired Immunity Self-recognition and Self-tolerance The Immune System - Pathologies Immunology and cancer With development of cancer cell surface proteins (tumor antigens) appear that rarely appear If body recognizes surface proteins as non-self will destroy them most effective in eliminating viral tumor cells Hypersensitivities - allergies first exposure sensitizes to allergen - IgE production next exposure anaphylaxis - massive histamine release local - surface exposure systemic - body The Immune System - Pathologies Autoimmune diseases multiple sclerosis - white matter destruction myasthenia gravis - effects nerve/muscle communication Graves disease - excessive thyroid hormone production Type I diabetes - destruction of pancreatic islet cells glomerulonephritis - impaired renal function rheumatoid arthritis - destruction of the joints Acquired Immunodeficiency Syndrome Human Immunodeficiency Virus Enters cells through receptor mediated endocytosis A retrovirus infects mainly helper T cells uses the CD4 protein on cell surface carries genetic material as RNA inserts genetic material into host DNA w/ enzyme reverse transcriptase cell makes copies of the virus, releases them for further infection May be carried unknowingly in cells for years, being passed on during cloning Activation will destroy Helper T’s Poor immune response to simple things Applied Immunity and HIV Enter the body? Spread? Effect of infection? Cause of death?