Pathophysiology of blood
advertisement

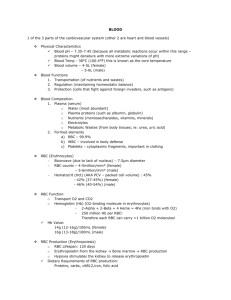
Pathophysiology of red and white blood cells, disturbances of hemostasis and coagulation Prof. J. Hanacek, MD, PhD. Remarks to physiology of blood 1. Main functions of blood • Transport of various substances (O2, CO2, nutrients, metabolites, minerals, ......) • Transport of heat (heating, cooling) • Signal transmission (hormons,...) • Carrier proteins – e.g. albumin • Buffering and defence systems (antibodies, white blood cells, oxidants-antioxidants, buffer systems) • Remove products of metabolism • Body homeostasis-temperature, water, electrolytes 2. Composition of blood • Blood cells (RBC, WBC, platelets) • Plasma (electrolytes, nutrients, metabolites, proteins, fat, carbohydrates, vitamins, gases....) 3. Development of blood cells • Hematopoietic tissues - red bone morrow (in adult) - spleen, liver, other organs (pathologic conditions) • Pluripotent stem cells myeloid, erytroid, lymphoid precursor cells hematopoietic growth factors • Myeloid precursor cells myelopoiesis monocytes tissue macrophages (in bone morrow) mast cells, maturation eosinofils, neutrophils, basophils • Lymphoid precursor cells lymphopoiesis LyT, LyB (in spleen and lymph nodes) maturation 4. Factors and hormones involved in prolifaration and maturation of blood cells • Erytropoietin (EPO) proliferation and maturation of ER (from kidney) • Thrombopoietin prolifaration and maturation of (from kydney) • Paracrine factors: megacaryocytes platelets - colony stimulating factors (CSF) - stem cells factor release CSF and IL 3, 6, 11, 12 Androgens, Thyroid hormons (in bone morrow) CSF and IL formation are inhibited by TGF beta and by TNF alfa A. Abnormalities of red blood cells I. abnormalities in mass of RBC 1. Anemias 2. Polycythemias Anemias Definition: Reduction below the normal level in the number of RBC, the quantity of Hb, and the volume of packed RBC (Htk) per 100 ml of blood Classification: • According to the mean corpuscular volume (MCV) of RBC: Normal MCV 90 fl - micro- normo cytic anemia - macro • According the mean corpuscular Hb (MCH): Normal MCH 30pg - hypo - normo chromic anemia - hyper Etiopathogenetic classification a) reflects steps in Er-poiesis RBC production defective RBC production b) reflects life-span of Er RBC loss Causes leading to defective RBC production: ● hemoglobinopaties - e.g. sickle cells disease, ● impaired globin synthesis – e.g. thalassemias ● RBC membrane defects – e.g. hereditary spherocytosis ● enzyme deficiency - ATP due to pyruvate kinase - G- 6 - phosphate dehydrogenase Causes leading to decreased and/or defective RBC production Disseminated malignancies - e.g. brest cancer, leukemias... Serious chronic disease - e.g. inflammatory, endocrine.... Lack of essential vitamins - e.g. B12, folic acid, C vitamin... Lack of iron Bone morrow failure Causes leading to RBC loss Bleeding - e.g. peptic ulcer, polyps in colon, GIT malignancies, hemorhoids, esophageal varices... Hemolysis - e.g. due to decreased resistance of RBC (defects in RBC membrane, defects in RBC metabolism) or due to changed microenvironment surrounding RBC (mechanical, imunologic, toxic influences) Aplastic anemia (AA) – insufficient number of RBC is produced Pathogenesis: - multifactorial disease genetically determined - primary proliferation defect of the hemopoietic system - immune reaction directed against hemopoietic system Mechanisms probably involved in AA development • immune reaction mediated by T-cells or less frequently by B-cells • many IL are produced in excess in patients with AA, e.g. IL-2, TNF – they inhibit activity of bone morrow function • abnormal sensitivity of hemopoietic cells is assumed, so probably, hemopoietic tissue is primarilly diseased Cosequences: If the immune reaction is strong enough it wipes out abnormal cells acute severe aplasia If the immune reaction is rather weak mild chronic pancytopenia will develop Causes of AA • Direct toxicity – Iatrogenic causes - radiotherapy - chemotherapy – Benzen – Intermediate metabolites of some common drugs • Immune-mediated causes – Iatrogenic causes, e.g. - transfusion-associated graft-versus host disease - Eosinophilic fasciitis - Hepatitis-associated disease - Pregnancy - Intermediate metabolites of some common drugs - Idiopathic AA Iron deficiency anemias (IDA) • Characteristics - serum Fe<0.4mg/l, serum ferritin • Main causes: - Blood loss – the most common cause of IDA in adults (0.5mg Fe lost/1ml blood) - Fe recycling is decreased (the 2nd most common worldwide) – occurs with chronic infections (Fe regained by the macrophages decreased releasing of Fe for Hb production reuse of Fe - Fe uptake from GIT is too low (malnutrition) - Fe absorbtion is reduced due to: 1. Achlohydria (atrophic gastritis...) 2. Malabsorption in upper part of GIT, Fe-binding food components (fytates, tannic acid) -Fe requirement (growth, pregnancy, breast-feeding) - Apotransferrin defect Iron deficiency inhibition of Hb synthesis hypochromic microcytic anemia Sideroblastic anemia – hypochromic anemia caused by inability of RBC to use of Fe in Hb synthesis Pathogenesis: genetic defect linkaged to X-chromosome (men are more severely affected) mitochondrial lesions sequestration of Fe complexes in the mitochondria of erythroblasts sideroblasts Megaloblastic anemia due to abnormalities in DNA synthesis Main causes: - abnormalities in the absorbtion and metabolism of folate or B12 vitamin Consequencies: inhibition of DNA synthesis cell cycle is slowed down during erythropoiesis delay in RBC maturation Hb synthesis in cytoplasm is unchanged size of ER (megaloblasts) megalocytes in blood Megalocyte = MCV > 100 fl formation of granulocytes and megacaryocytes is also disturbed premature destruction of megaloblasts in bone morrow (inefficient erythropoiesis) and shorten life of megalocytes (premature hemolysis) Main disorders of folate absorbtion and metabolism • folate uptake • folate requirement • malabsorbtion, e.g. diseases of small intestine(terminal part) • cobalamine deficiency Causes: - too litle folate uptake with food - intrinsic factor deficiency - competition for vitamin B12 (bacterias, broad fish tapeworms- Diphyllobothrium latum) - absence of the terminal ileum or its inflammation- site of absorbtion of cobalamine - defective transcobalamin II Pernicious anemia (PA) - the most common type of megaloblastic anemia - „pernicious“= highly injurious and in the past fatal Pathogenesis: defective gastric secretion of intrinsic factor - congenital deficiency - atrophy of gastric mucosa - partial or complex gastrectomy Consequences: - megaloblastic anemia - neurologic disorders Posthemorhagic anemia • normochromic, normocytic anemia caused by sudden loss of blood Main cause – strong bleeding, lost of large amount of blood during relatively short time Course of posthemorhagic anemia 1st step – substitution of lost plasma volume plus Er from depots 2nd step – acceleration of hemopoiesis mass of Er in bone morrow Recovery of normal number of Er after bleeding – afer 4 – 6 weeks Recovery of normal Hb concentration can last 6 – 8 weeks Hemolytic anemias (HA) Schyzocytes Characteristic signs: – premature destruction of Er – erythropoiesis can be normal – abnormally short life span of Er – erytropoiesis is accelerated Causes and pathogenetic mechanisms of HA development – inherited – acquired Causes of acquired HA – infections, systemic diseases (e.g. lupus erythematosus) – poisons – drugs, toxins (endo- or exogenous) – disturbances of liver and kidney – abnormal immune reactions – e.g. transfusion reaction, hemolysis of newborns, autoimmune reactions Causes and mechanisms of inherited HA Mechanisms: – defect of Er membrane – defficiency of glycolytic enzymes – disturbances in Hb synthesis – others Other pathomechanisms particiating in HA development – physical destruction – trauma, arteficial heart valves, super-long march or run ? – heat and irradiation Disturbances of white blood cells 1. Leukemias Main pathogenic mechanisms – structural changes of the normal genes (protooncogens oncogens) – loss or inactivating genes (antioncogens) – activation of oncogens and loss of antioncogens leads to: – increased proliferative activity of the cells – cell loses ability to diferentiate and to apoptosis Some oncogens related to leukemias: – Philadelphia chromosome =translocation of ABL gene from chromosome 9 to chromosome 22 and its fusion to gene BCR Acute myeloblastic leukemia (AML) - disseminating, clonal proliferation of inmatured hematopoietic cells - 90% of AL in adults is myeloid type Possible causes of AML: – irradiation – chemical agents, e.g. benzene – viruses Main manifestations of AML: - cytopenia and blast present in blood - neutropenic fever - anemia, thrombocytopenia - hyperuricemia, hyperkaliemia, hyperphosphatemia - number of blast cells in peripheral blood > 50,000/l leucostasis Consequencies: blood viscosity rigidity of blast cells increased risk of leucostasis agglutination - bleedinng to brain - lung and kidney failure Disorders of hemostasis • Hemostatic system is composed of: – plasma coagulation factors – platelets – vessel wall – inhibitory (anticoagulant) factors – fibrinolysis system – dissolving excessive fibrin clots Hemorhagic diathesis (HD) = increased bleeding tendency Main causes: - disorders of coagulation, fibrinolysis, platelets - vascular defects Consequences: • if coagulation and fibrinolysis is inadequate - minimal mechanical injury hematomas bleeding into joints • if trombocytes and vascular wall are damaged - punctate, tiny cutaneous bleeding Pathogenetic mechanisms leading to disturbancies of coagulation and fibrinolysis in patients suffering from sepsa activation tissue factor sepsa (endo)toxin cytokines inhibition fibrinolysis by PAI-1 depression of inhibitory system deposition of fibrin organ failure Levi et al. Eur J Clin Invest 1997;27: 3-9