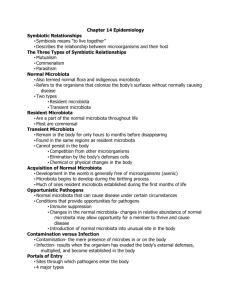
Normal Microbiota in Hosts
advertisement

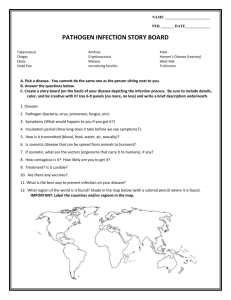
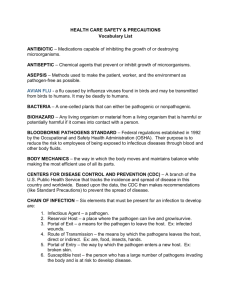
Disease, Disease Transmission, and Epidemiology Chapter 14 Symbiotic Relationships Between Microbes and Their Hosts • Types of symbiosis – Mutualism – Commensalism – Parasitism Table 14.1 The Three Types of Symbiotic Relationships Figure 14.1 Mutualism as shown by wood-eating termites Symbiotic Relationships Between Microbes and Their Hosts • Normal Microbiota in Hosts – Organisms that colonize the body’s surfaces without normally causing disease – Two types • __________microbiota • __________microbiota Symbiotic Relationships Between Microbes and Their Hosts • Normal Microbiota in Hosts – Acquisition of normal microbiota • Development in uterus is free of microorganisms • Microbiota begin to develop during birthing process • Much of your resident microbiota is established during first month of life Symbiotic Relationships Between Microbes and Their Hosts • How Normal Microbiota Become Opportunistic Pathogens – Opportunistic pathogens • Normal microbiota that cause disease under certain circumstances – Conditions that provide opportunities for pathogens • • • What is a disease? • Infection – – Most infections are eliminated by the bodies defenses • Disease – Infections may lead to disease – • Causation of Disease – Germ theory of disease • Disease caused by infections of pathogenic microorganisms – Robert Koch developed a set of postulates to prove a particular pathogen causes a particular disease • Exceptions to Koch’s postulates – HIV/AIDS » Not ethical – Syphilis » Not culturable in lab The Nature of Infectious Disease • Manifestations of Disease: Symptoms and Signs • Symptoms – • Signs – • Asymptomatic – Infections that lack symptoms but may still have signs of infection and can be transmitted Classification of Infectious Diseases • Terms used to classify infectious disease – _________disease (rapid onset, short period of time ex. Common cold) – _________disease (develop slowly, continual or recurrent ex. Hepatitis C, TB) – _________disease (pathogen remains inactive for a long period of time before becoming active ex. shingles) • The Stages of Infectious Disease – Many infectious diseases have five stages following infection • ____________period (time between infection and first symptoms and signs of disease) • _____________period (short time, mild symptoms) • ____________(severe stage, signs and symptoms most evident) • ____________(gradual decline of signs and symptoms as body returns to normal due to immune response or drug treatment) • _____________(patient recovers no signs or symptoms) – Patient can be infectious at any stage of disease depending on the causative agent Number of microorganisms or intensity of signs or symptoms Figure 14.10 The stages of infectious diseases Incubation Prodromal period period (vague, (no signs or general symptoms) symptoms) Illness (most severe signs and symptoms) Time Decline (declining signs and symptoms) Convalescence (no signs or symptoms) How do we acquire a disease causing organism? • Most pathogens cannot survive for long outside their host – A successful pathogen needs to overcome the innate and adaptive defenses long enough for the pathogen to multiply and exit the host • It is a disadvantage for the pathogen to actually kill a host, since the opportunity to be transmitted may be limited and it loses the source of nutrients • Reservoirs of infection • Reservoirs of infection – • Reservoir may or may not be harmed by pathogen • Three types of reservoirs – __________reservoirs – __________reservoirs – __________reservoirs • Human reservoirs – The principle living reservoir- the human body – – Infected individuals who are ___________ but infective to others (before or after onset of illness) – Some individuals remain asymptomatic and infective for years (ex. Tuberculosis, syphilis, and AIDS) • • Animal Reservoirs – __________or Zoonotic diseases (150 diseases) • Diseases naturally spread from animal host to humans – Acquire zoonoses through various routes • _____________with animal or its waste (E. coli O157:H7) • __________animals (tape worm) • ____________(Rabies) • ____________(Lyme Disease) • Nonliving Reservoirs – _______________________can be reservoirs of infection • Presence of microorganisms often due to contamination by feces or urine • Can be naturally occurring in environment (Tetanus and botulism) • Water (Example: parasitic eggs or E. coli) • Meats and vegetables The Movement of Pathogens Out of a reservoir: ______________ • Pathogens leave host through portals of exit • Many portals of exit are the same as portals of entry • Pathogens often leave hosts in materials the body secretes or excretes Figure 14.11 Portals of exit Eyes (tears) Ear (earwax) Nose (secretions) Broken skin (blood) Mouth (saliva, sputum) Skin (flakes) In females: Mammary glands (milk, secretions) Vagina (secretions, blood) Anus (feces) Seminal vesicles (semen and lubricating secretions) Urethra (urine) Movement of a pathogen into a host • Portals of Entry – Sites through which pathogens enter the body – Four major pathways Broken • • • • skin Insect bite Ear Conjunctiva of eye Mouth Placenta Anus Vagina Penis Urethra • Portals of Entry – Skin • Outer layer of dead skin cells acts as a barrier to pathogens • Some pathogens can enter through openings or cuts • Others burrow into or digest outer layers of skin • Portals of Entry – Mucous membranes • Line the body cavities that are open to the environment • Respiratory tract is the most common site of entry – Entry is through the nose, mouth, or eyes • Gastrointestinal tract may be route of entry – Must survive the acidic pH of the stomach • Portals of Entry – Placenta • Typically forms effective barrier to pathogens • Pathogens may cross the placenta and infect the fetus – Can cause spontaneous abortion, birth defects, premature birth – Listeria (lunch meats) • Portals of Entry – Parenteral route • Not a true portal of entry – A way portals of entry can be bypassed • Mechanically depositing pathogens directly into tissues beneath the skin or mucous membranes – Hypodermic needles – Thorns, nails, etc.. Modes of Infectious Disease Transmission • Transmission is from a reservoir or a portal of exit to another host’s portal of entry • Three groups of transmission – • – • – • Contact Transmission Direct Contact • One person physically touches another – Handshake – Sexual intercourse – Fecal-oral Contact Transmission Indirect Contact • Transfer of pathogens via inanimate objects (called fomites) – Clothing – Doorknobs – Glasses and eating utensils Ex. Scabies: Bedding serves as fomite involved in transmission Contact Transmission: Droplet • Transmission of a pathogen through inhalation of respiratory droplets. – Large microbe saturated droplets fall to the ground no farther than 3 feet from release. • Close proximity necessary – Coughing – Sneezing • Examples of diseases: – Cold, Flu Vehicle Transmission: Airborne • Transmission of a pathogen that is suspended in the air and travels through the air to another host • Very difficult to control! • Remains suspended indefinitely – Coughing – Sneezing • Examples of diseases: – Tuberculosis, Measles Vehicle Transmission: Food • Usually digestive tract diseases • Contamination can occur in a variety of different ways • Animals can harbor pathogens – Salmonella – E. coli O157:H7 • Inadvertently added during food preparation – No handwashing • Staphylococcus aureus – Cross-contamination • Cutting board used on meat and vegetables for your salad • Meat and vegetable processing facilities Vehicle Transmission: Food • – – Toxin causes illness not the living organisms – Staphylococcus aureus and Clostridium botulinum Vehicle Transmission: Food • – • Undercooked hamburger or chicken – Symptoms do not usually appear for at least 1 day • Diarrhea – Thorough cooking before consumption will kill the organisms – E. coli O157:H7 – Salmonella Vehicle Transmission: Water • Can involve large numbers of people • 1993 Cryptosporidium parvum (intestinal parasite) – Watery diarrhea 10-15L a day – Infectious dose: less than 10 organisms – Milwaukee, WI • Infected ~400,000 people from municipal water source Vector Transmission – – 1. Biological Vector • An organism transmits and serves as host. • – Ex: Malaria: Part of life cycle of protozoan, Plasmodium, occurs inside the Anopheles mosquito 2. Mechanical Vector – Ex: Trachoma (Blindness): Chlamydia trachomatis carried on feet of fly from infected person's eye to eye of new host Epidemiology • Epidemiology focuses on the effect of a pathogen in a population – The study of where and when diseases occur and how they are transmitted in a population. • Why is this field important? – Earth’s population is becoming over populated. – Humans are relying more on mass food production and distribution – Travel to other countries very readily. – Leads to higher incidence, number of new cases of a disease in a population) – Prevalence, the total number of cases, new and already existing in a population Occurrence of an infectious disease can be classified in terms of geographic distribution and frequency. • • • • • Sporadic Endemic Outbreak Epidemic Pandemic Sporadic • Example: • Plague in U.S. • Endemic • Endemic disease can lead to epidemic Example: • Pertussis in U.S. • Common cold • Influenza Year Reported Cases* 2000 7,867 2001 7,580 2002 9,771 2003 11,647 2004 25,827 2005 25,616 2006 15,632 2007 10,454 2008 13,278 2009 16,858 2010 27,550 2011* 18,719 *Total reported cases include those with unknown age. Outbreak • Implies a cluster of cases occurring during a brief period of time and attacking a specific population, usually food borne • E. coli O157:H7 from contaminated food sources Seventy-seven people sick and one died in a salmonella outbreak caused by contaminated ground turkey: Centers for Disease Control 2011 Epidemic • Affecting an unusually large number of individuals within given region or population • Epidemic may lead to pandemic • H1N1 was epidemic in US in 2009 • Pandemic- epidemic on more than one continent – Example 2009 H1N1, also known as Swine Flu, breaks out and quickly spreads to more than 70 countries. Pandemic • A disease affecting an increased proportion of the population over a wide geographic area, most often worldwide Example: • AIDS • Local and state level health departments rely on doctors and hospitals to report infectious diseases. • In some cases the disease occurrence is nationally recorded to the Center for Disease Control (CDC). – Weekly updates can be viewed of the notable diseases in the Morbidity and Mortality Weekly Report (MMWR). Epidemiology of Infectious Diseases • Hospital Epidemiology: Nosocomial Infections – Control of nosocomial infections • Disinfection, good housekeeping, bathing, sterile procedures, and HAND WASHING! • • CDC reports that on average, health care workers wash their hands before interacting with patients only __________________ Figure 14.20 The interplay of factors that result in nosocomial infections Factors that influence nosocomial infections:>>>>> Immunocompromised patients Presence of microorganisms in hospital environment Infection can result from any one of these factors but usually it is a product of all three Nosocomial infection Transmission of pathogens between staff and patients and among patients Emerging Disease • What is an emerging Disease? • Examples: – West Nile virus – HIV/AIDS – Cat Scratch Fever Factors that contribute to disease emergence • Microbial evolution • Advances in technology • Mass production, widespread distribution and importation of food • Climate Change Reemerging Diseases • Resurgence of old diseases due to: – – – Diseases include: TB, Pertussis Tuberculosis reemerging in US • Mycobacterium tuberculosis – Causes an infection of the lower respiratory system – Inhalation of airborne bacteria from infected persons – 9 million people each year develop TB • 2 million deaths • About 2 billion people world wide are infected • 14,000 cases annually in US usually from foreign born individuals. Increasing at rate of about 2% each year. Pertussis commonly called whooping cough • Bordetella pertussis • Causes an infection of the lower respiratory system • Before DTP vaccination 50% of individuals would develop pertussis. • Vaccination significantly decreased this disease – Since 1980s number of cases has increased significantly affecting adults and adolescents. • Individuals are not up to date on booster shots which are intended to boost immunity • Immunity to the DTP vaccine declines after a few years – No protection by age 12