File - Wk 1-2
advertisement
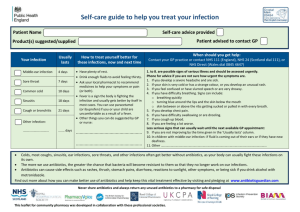
Infection 1. Explain the concept of normal flora and its role in the maintenance of health 2. List the commensal organisms of the skin and common skin pathogens 3. Outline the mechanisms by which normal flora can cause opportunistic infections. 4. Outline the pathogenesis of infection, its effects on the host and the role of host factors in the development of disease 5. Explain how bacteria spread both within a host and between hosts 1. Normal skin microflora are those microorganisms which reside on the skin surface. They are usually non-pathogenic bacteria, and offer protection to the body by preventing pathogenic organisms from colonising on the skin surface, either by using up available nutrients themselves or excreting antimicrobial compounds. This is known as a ‘commensal relationship’, where the parasite benefits and the host is unharmed <’commensal’ = sharing of food’>. Properties of the skin such as saltiness, fatty acids, and the largely impenetrable keratin matrix assist normal flora regulation. 2. Most normal skin bacteria are Gram +ve aerobes. The most common skin commensals are: Staphylococcus epidermidis, Staph auerua Mycobacteria Propionibacterium Corynebacteri Skin viral infections: Human papillomavirus (HPV), responsible for warts Molluscum contagiosum: lesion in children produced by DNA pox virus Herpes viruses: various disease, eg cold sores, herpes zoster variant = chickenpox. HIV: in skin can cause blood vessel tumor, Kaposi’s sarcoma. Skin Bacterial infections: Impetigo: staphlycoccal infections forming subcorneal pustules. Cellulitis: caused by Streptococcus pyogenes, localized inflammation response Tuberculosis/Leprosy: uncommon in developed countries Skin Fungal Infections: Pityrosporum: superficial finga infections (tinea) Deeper funga infections tend to cause chronic abscesses, common in tropical areas. 3. Pathogens are classified as either: o Primary – either always or sometimes cause infection in the host or o Opportunistic – only cause disease in compromised hosts (eg staphlycoccus, epidermidis, candida albicans). Opportunistic organisms become pathogenic when a route for infection (eg an open wound) becomes available in addition to the person being immuno-compromised. This may occur as a result of genetic defects, exposure to antimicrobial drugs or immunosuppressive chemicals (eg chemotherapy) or as a result of an infectious virus. 4. The sequence of events in infection: a. Enter: respiratory inhalation, ingestion in food/water, inoculation by needle or insect/animal bite, close human contact, burns, wounds or any other breach of epithelial integrity. . 1st barriers are the skin and mucosal surfaces and their secretory products. Generally, gastrointestinal, genitourinary, respiratory tract infections occur in healthy persons and are caused by relatively virulent organisms that are capable of damaging or penetrating intact epithelial barriers. b. Establish: Dependant on appropriate conditions for pathogen growth, the populations required to infect the host (‘infective dose’), the organisms virulence, and the activities of the host. Transmission may also occur at this point forwards. c. Evade host defences: pathogens use the properties of their outer layers (cell wall, membrance, capsule) to resist attachment of antibodies, resist phagocytosis, or release enzymes to penetrate host tissues and embed the infection. d. Damage host: Enzyme release causes damage to connective tissues (direct damage). Pathogens also induce inflammatory responses, release endotoxins (by submitting to phagocytosis where host cells lyse) and Exotoxins, which disrupt cell metabolic processes and neurotransmission. e. Resolve: when either the bodies innate or acquired immune system overcome viability of the pathogen, with subsequent subsiding of inflammation, or the conditions for growth change and the pathogenic is unable to maintain a diseasecausing population. 5. Transmission: In a virulent pathogen, with infective dose populations present, transmission to other hosts can be via two routes: o Human to human: vertical (between parent and child, either via gametes, placenta, milk or contact) or horizontal (non-paternal transmission between humans via one of the routes described in part 4.). Numbers of people that can be infected horizontally for a particular pathogen. Show typical incidence. o Animal to human: injection of saliva or faecal contaminant.