Immunology - stjpap 2011
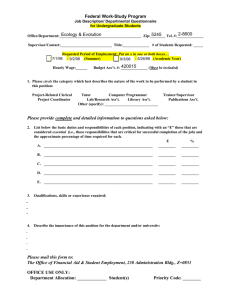
advertisement

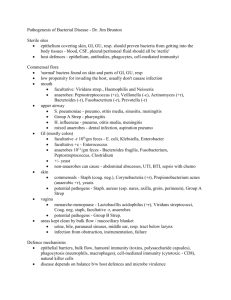
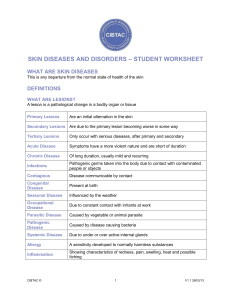
Immunology Innate Immune system: present at birth, non-specific resistance (skin, mucus membrane, salvia, NK cells, monocytes) Acquired Immunity: developed over time with memory + specificity WBCS: Neutrophils: ↑ if bacterial infection/inflammation Bands: baby neutrophils Dendritic cells: Skin Macrophages Eosinophils: ↑ if allergens, parasites, neoplasm, asthma Basophils: secrete histamine + heparin Lymphocytes: (T/B cells) ↑ if viral infection Steroids/ Anti-inflammatory lower resistance to infection Fever ↑cytokines, ↑ metabolic rate, ↑ tissue repair, ↑wbcs Cytokines stimulate inflammation + enhance phagocytes Interferon: polypeptides secreted by cells infected with viruses (viral warning sign) which activate NK cells + macrophages Complement: set of enzymes + plasma proteins that cause “Cascade rxn” to destroy microbe MACROPHAGES Kupfer cells – liver Monocytes- immature macrophages in blood (chemotaxic) Histiocytes/Langerhands – skin Alveolar- lungs Mesangial –kidneys Microglial- CNS The Journey: Margination Diapedesis Chemotaxis Phagocytosis Acquired Immunity: a. Passive- Ab/Ig given to a person from an external source b. Active- you make the Ab (can be from a vaccine with an antigen) Spleen: destroys old RBCs and removes encapsulated bacteria (H. flu + pneumococcal) B-Cells: a. Plasma- make Ig b. Memory- reason for vaccines T-Cells: a. CD4: secrete cytokines (messengers/activators) b. CD8: killer cells for virus c. T suppressor: stops CD8 from killing + decreases function of all immunity cells Epitope- smallest identifiable portion of antigen 3 types of Antigens: 1. Immunogen- molecule (foreign, large, complex) that stimulates immune response II. Haptens- need to be coupled with carrier to stimulate response III. Tolerogen- the more exposure decreases the immune response MCH-1 : on all cells (individualized to you) + presents foreign matter to CD8 cells **CD8 recognize change in MCH-1 and then kill antigen cells MCH-11: help CD4 cells with recognizing APC (antigen presenting cells - macrophages/B-cells) Steps: 1. APC kills antigen and holds out prize 2. CD4 recognizes prize by attaching with APC 3. CD4 activates cytokines/immune rxn 4. T-B cell coop: B-cell presents with Ab-Ag complex and T cell CD4 releases cytokines to ↑ B cells division + production of plasma cells B-plasma cells make the Antibody: 2 heavy + 2 light chains + Fc IgG- crosses placenta, inside Ig, 2nd response, blood/lymph/CSF IgA- outside, neutralizes exotoxins, in breast milk, sweat, saliva, GI secretions, GU secretions, resp. secretions IgM- primary/early response, agglutination rxn, on surface of B-cells IgE- allergens, parasites, degranulation of mast cells IgD- on surface of mature B cells Humoral Immunity = Bcells = extracellular infection = bacteria Cell-Mediated immunity = T cells = intracellular infection = viral Hypersensitivity RXNs 1. Immediate/Anaphylaxis/IgE/allergy to food 2. IgG/IgM (blood transfusions, Rh incompatibility, drug rxn) 3. Ab-Ag circulate and cause tissue damage (SLE) slow + chronic 4. T-Cell mediated (delayed) induced by cytokines (ie: poison ivy, PPD, hepatitis) Autoimmune Diseases: 1. Exogenous Mechanisms: a. Molecular Mimicry- Ag looks like host b. Super-antigenic Stimulation- Ag/Toxin bind to MCH-11 and cause ↑ in Tcell activation 2. Endogenous Mechanisms a. Neoantigens- altered self antigens b. Loss of T-cell suppression, cytokine imbalance, increase in B-cell function Transplants **The greater the difference in HLA the faster/more aggressive the immune attack Autograft: transplant from yourself Allograft: transplant from same species Xenograft: transplant from different species **children can get transplant from parents **parents can NOT get from children Twins> siblings> parents ** cornea, liver, kidney don’t need compatibility Host vs. Graft: your T-cells kill the graft 1. Chronic- organ functions for weeks-years then slowly scar tissue replaces graft (minor MHC diff.) 2. Acute- 7-12 days then rapid destruction (MCH > 50% difference) 3. Hyperacute- antibody mediated b/c of previous exposure to transplants Graft vs. Host Bone Marrow Transplant Rh Dilemma: mom is Rh neg. and first baby is Rh + mom may develop Rh antibodies and 2nd child will be stillborn therefore GIVE Rhogam Gram Stain g- does take the saffron dye b/c thin membrane with 2nd lipid layer g + does NOT take saffron dye b/c of thick membrance Prion- no DNA or RNA found in CSF and causes Mad-Cow disease and KURU Mycoplasm – lack a cell wall, resistant to PCN Spirochetes – depend on vector transmission Endemic- disease occurring predictably in specific area Incidence- # of new cases/time Prevalence- total # of cases/time Epidemic- sudden outbreak in region Pandemic- all over outbreak Incubation Prodrome Acute Convalescense/Chronic Sterile fluids: CSF, blood, urine, synovial, bile, pleural, pericardial (need aseptic technique) Microbial Factors that increase Virulence: 1. Adhesion- bind to cell receptor 2. Evasive- LPS, leukocidin, C-toxins 3. Invasive- phospholipases, elastases, proteases, enzymes that break cell membrane Staph. Aureus: G+ cocci in clusters Strep. Pyogenes: G+ cocci in strings Neisseria Gonorrhea: G- diplococci Ecoli/Pseudomonas: G- rod G + cocci = Staph, Strept, Enterococcus G – cocci = Gonorrhea, N. menigitidis, M. cat G + rod = Bacillis, Listeria, Corynebacterium Aerobic g – neg. = Ecoli, Shigella, Proteus, Enterbacter, H flu, Pseudomonas, Klebsiella, V. cholera, H. pylori Acid Fast = M. leprae, MAC, Tb Commensalism- one benefits + other has no harm or benefit Mutualism- both benefit (Ecoli + our colon) Parasitism- one benefits + the other is harmed/destroyed Vertical Transmission: mother fetus (TORCHES) Ingestion: Hep A+E, cholera, staph (in creams and cakes) Bloody Diarrhea: Salmonella, Ecoli, Campylobacter (mc), Shigella, Yersina Viruses- ↑↑ oncogenesis by changing the DNA Bacteria- reproduce via binary fission Spirochete- helicial, gMycoplasma- smallest free-living unicellular organism Rickettsia- small intracellular parasite Yeasts- monocellular (reproduces via budding) Molds- multicellular (reproduce via hyphae) Exotonins- goes into circulation (Diptheria, Botulinum, Tetani, Cholera) Enterotoxins- GI only (G- neg only) Ecoli, Clostridium perfinges, Cholerae Sublinical infection- doesn’t cross clinical threshold Subacute- btw acute + chronic Fulminant- abrupt onset of sx w/o prodrome Bacteremia vs. septicemia (toxins or bacteria or virus in blood) Latent- dormant SIRS- systemic inflammatory response syndromes Syndrome is sx w/o ID of bacteria OR end organ damage SX: tachycardia > 90; tachypnea> 20 breaths/min; WBCs > 12,000, hyperthermia Sepsis = SIRS + positive blood culture Wet Mount = ID fungus or trichomonsis Tzank smear = ID virus Bandemia = shift to left w/ increase in PMNs Vaccinations Active: Live- MMR, Varicella, Zoster (CI: pregnant or immunocompromised Inactivated- flu, polio, small pox Recombiant DNA Passive: TDap, Rabies, Hep B, Hep A, Snake or Spider Anti-venom PPD: False + BCG False – (neg) HIV + (immunocompromised) o > 5mm = HIV + o > 10 mm = healthcare worker, homeless, Dm, prison, from endemic region o > 15 mm= everyone “Neutropenia with lymphocytosis” Viral infection with shift to right (virus- mono, HIV, flu) “Neutrophilia with lymphopenia” Bacterial infection with shift to left Eosinophilia: Neoplasm, Asthma/allergies, Addison’s, Collagen Vascular Dz, Parasites Never (neutrophils) Let (lymphocytes) Monkeys (monocytes) Eat (eosinophils) Bananas (basophils) Dermatology Layers of skin: 1. Epidermis a. Coreum b. Lucidum- only in palms + soles of feet c. Granulosum- has kerito-hyaline d. Spinosum- w/ dermosomes + Langerhan cells e. Basal – layer with melanocytes 2. DERMIS- thick w/ collagen + fat 3. Sub-Q- blood vessels + eccrine glands Hair Growth: Anagen Catagen Telogen Sweat Glands: 1. Eccrine: in dermis on skin surface 2. apocrine- deep and open thru hair follicle (in axilla/groin) **resp. for body odor Darier sign = rub and make wheal is pos. sign Auspitz sign = Pt scale is remved + there is pinpoint bleeding Nikolsky sign desquamation (separation of skin layers) Koebner phenomenon = minor trauma makes pt scratch (+ in psorias) Wood lamp = UV light to see tinea capitis Acetowhitening = acid allows us to see white penile/vaginal warts Dark Field Exam = spriochetes Folliculitis: hair follicle infection Furnucle: acute, deep seated, 1 hair follicle w/ adjacent tissue Mcc is staph Found in thight, axilla, face, neck, butt Carbuncle: depper, interconnecting, several hair follicles, into dermis + Sub-Q tissue, draning pus; scarring Ass. with systemic sx MCC: staph, pseudomonas Risks: shaving, waxing, steroids, obesity, poor hygiene, humidity, Dm, increased body temp TX: topical mucpirocin (Bacteroban); po antibiotics- Naficillin/Dicloxacillin Hidradentis Suppurativa: sweat glands w/ pus in axilla or groin Chronic infection of apocrine glands MC: Africian American females Risks: smoking, obesity, genetics, occlusions of follicles and glands Occlusion of follicle duct inflammation leads to infection ruptures casuing sinus tract formation SX: tender/inflammated nodules, abscess, sinus with scar tissue formation “DOUBLE OPEN COMEDOMES” DX: BX TX: steroid injection, I+D, surgery, oral antibiotics, isotretinoin Impetigo: break in skin skin infection Mc in children autoinfection “Honey Colored Crusts” on face Non-bullous: lesions scattered + discrete Bullous: vesicles + bulla Non-bullous SECONDARY impetigo = has underlying eczema Staph is MCC Cx: glomerulonephritis w/ strep infection Tx: topical mupirocin Cellulitis: infection of dermis + sub Q with systemic sx and indistinct border Red streaks = lymphangitis SX: red, swollen, hot, tender Etiology: staph, strept, DM- polymicrobial Risks: trauma, ulcer, Dm, Ca, dermatitis DX: g stain, bx, culture, CBC CX: Glomerulnephritis w/ strep TX: wound care/ topical mupirocin/ systemic antibiotics: (strep-PCN, staph- Diclox/Clox, Dm- Unasyn) Erysipelas: more superficial cellulitis w/ only superficial dermis tissue involved more sharply demarcated Necrotizing Fascitis: flesh eating bacteria ( in Sub-Q + fascia) Risk: health pt after trauma Etiology: Strep, Staph, Clostridum Sx: swollen cellulitis, with quick progression along fascia plane Change in color = Red Purple Grey Blue with watery malodorous discharge DX: shock; “Gas gangrene”- Clostridium If in perineum/genitals- “Fourner’s gangrene” TX: surgical debride, po Antibiotics HPV- codyloma acuminatum (genital warts) Sx: + Auspitz Plantar warts: increase in depth in foot w/ pressure painful w/ pressure Anogenital- mc STD in US o HPV that cause cancer: 16, 18, 31 o “cauliflower lesions- small discrete” o DX: pap smear, BX, PCR o TX: cryosurgery HSV-2: MC STD worldwide First case is usually worst however, first case could be asymptomatic Classic sx: primary infection is worst (in sacral nerves) hides in dorsal root ganglion Reactivates in same area due to: UTI, URI, trauma, HIV, immunocompromised Prodrome: tingling, numbness + pain @ site, lymphadenopathy SX: grouped painful lesions with pustules which may form ulcers Dx: Tzank smera (see Giant multi-nucleated cells); Viral culture TX: Acylcovir Cream (tx/prophylaxis) HSV-1: child/acute gingivostomatitis- around mouth/lips On mucus membranes On corena of eye dendritic lesions (do not use steroids) Herpetic Whitlow: painful vesicle on finger/hand (autoinoculation) Herpetizing ecezema: underlying dermatitis Mc is trigeminal nerve DX: viral culture, Tzank smear TX: acyclovir cream Varicella: chickenpox Varicella is teratogenic in 1-2 trimesters Do not give kids ASA Reye’s “a person with herpes zoster can give a PT primary Varicella but not visa versa” MC in winter-spring Invades dorsal root ganglion; comes in crops 1. Prodrome with systemic sx 2. first crop- disseminated pruritic macules + papules on scalp/face spreading to extremities on mucus membranes Vesciular lesions evolve in 12 hrs with clear liquid Shingles (herpes Zoster): along a dermatome; mc in elderly, HIV, immunocompromised prodrome: sharp lancing pain with tingling + tenderness + pruritis “Group vesicles along a dermatome unilateral” Mc dermatome: thoracic > cervical > trigeminal > lumbar DX: viral culture, Tzank Smear TX: po Acyclovir + acyclovir cream (use po acyclovir as prophylaxis in high risk pt) CX: 1. post herpetic neuralgia 2. Ophthalmic Zoster (CN V) blindness (Hutchingson’s sign- vesicle on tip of nose) 3. Ramsay Hunt Syndrome: CN VIII- in ear canal deafness Molluscum Contagiosum: “central umbilication” with molloscum bodies Round, firm, skin colored waxy pearly papules; keratotic plug releases exudate w. pressure Etiology: pox virus MC : in kids on face/eye; in adults- STD on genital DX: Bx; keratotic plug Pityriasis Rosea: herpes virus- hearld patch (large+ red) 1-2 weeks early then Christmas tree pattern on trunk Cutaneous Tb: ↑ risk in homeless, poverty, HIV 1. Tb chancre- firm, red/brown, painless papule, with LAD 2. Lupus Vulgaris- apple red jelly lesions DX: BX: caseating granulomas with acid fast bacilli; PPD, CXR, sputum g stain TX: RIPE Leprosy (Hansen’s): mc in Africa, South Asia, South America Affects skin, mucus membranes, PNS, eyes DX: BX- granulomas with nerve involvement and acid-fast bacilli First sign = numbness temp loss light touch pain deep pressure SX: plaques are anaesthetic + hypopigmented TX: Dapsone, RIF, Clofazimine; steroids; thalidomide Dermatophyte infections: RISKS: steroids, poor hygiene, occlusive clothing, athletes, increased temp DX: KOH w/ hyphae, wood lamp TX: topical- corporis, cruris, pedis; po- capitis/manuum; 1. Tinea corporis-annular/scaly lesions with central clearing + active border 2. Tinea capitis- crusted/scaling; “black dot” appearance b/c hairs breaks on scalp a. Hair loss not permanent, may have occipital LAD b. Kerion: prurlent scalp mass with abscess c. Tx of choice: griseofluvin 3. Tinea barbea- on beard; looks like folliculitis, but painless when you pull hair a. Tx of choice: terbinafine 4. Tinea unguim- Nails are lustless ass. with co-infection with tinea pedis a. TX of choice: terbinafine 5. Tinea Manuum- palms usually unilateral ass. with tinea pedis 6. Tinea Cruris- Jock itch 7. Tinea Pedis – MC (btw 4th and 5th digits) Tinea Versicolor- Malassezia furfur (not a dermatophyte) Pityrosporum yeast infection “fine dust scaly covering which does NOT tan in summer” TX: topical ketoconazole or selenium sulfide Candidiasis: muco-cutaneous transmission HIV + ororpharyngeal/ esophageal Women vulvovaginal (thick cottage cheese discharge); pendulous breasts Risks: immuncompromised, Dm, Cancer, Antibiotic use, trauma Satelite lesions- sharply demarcated w/ white TX: Nystatin; po fluconazole Vesicular Bullae Bullous Pemphigoid: autoimmune rxn + Nikolksky Subepidermal blister with immune activation Prodrome: erythema before blisters then lesions on extremities (flexor) 2 phases: 1.non-bullous: pruritis/eczema 2. bullous: vesicles; bulla with clear fluids Can be drug enduced diuretics, nsaids, antibiotics DX: reveals IgG or C3 at dermal-epidermal junctions TX: po + topical steroids + immunosuppressants Pemphigus Vulgaris- MUCOSAL LESIONS w/ pain and w/o pruritis Autoimmune rxn against keritinocytes with loss of adhesion Blisters break easily with clear fluid DX: immunoflourescence IgG + C3 Fatal if not treated with steroids (po) + immunosupressants Tx: Azathioprine, Methotrexate ACNE: due to androgens Black head- melanin plug TX: OTC, po antibiotics, Benzoyl peroxide, sebum suppressants Rosacea: peaks in 30-40s; ass. with Parkinson’s Related to vascular hyperactivity Red skin on nose, cheeks, forehead Ass. with Rhinophyma, Blepharophyam, metrophyma TX: Metronidazole; avoid triggers of food, alcohol, humid weather, clonidine DO NOT use topical fluorinated steroids on face!! Hypersensitivity Vasculitis: immune complex rxn- inflammation of arterioles/capillaries/venules Immune rxn to drug/infection/molecular mimicry/ Ag-Ab block capillaries Leads to vascular damage ischemia + necrosis Hx: drug/strep infection/ SLE/ arthritis (can become systemic) “Palpable purpura on legs + ankles with pain may form ulcers” DX: BX TX: Antibiotics, dapsone/immunosuppressants + prednisone Erythema Multiforme: “target iris lesions” 50% idiopathic + 50% drug/infection Lesions: involve on hands, feet, face, neck + mucus membranes with oral lesions <10% desquamation EM-minor: no mucus membranes/ no bulla EM-major: SJS is bullous SJS is < 30% desquamation with 2+ mucosal sites TEN: always a drug rxn + Nikolsky sign > 30% desquamation Mc drugs: NSAIDS, sulfa, antibiotics TX: 1. stop drug 2. TPN 3. Burn unit 4. debridement 5. systemic steroids Drug Eruptions: due to clinical situation + drug Due to excessive use, pharmacological side effect Drugs: PCN, cephalosporins, NSAIDS, INH, streptomycin, sulfa, chloramphenicol TX: antihistamine, topical steroids PT with mono (EBV) if you give ampicillin will have drug rxn 4-5 days after therapy HIV + rxn with sulfa drugs Drug Hypersensitivity- due to Pts genetics Drug acts as hapten (↑ eosinophils) Staph Scalded Skin Syndrome (Ritter’s disease) “exfoliative toxin” from staph usually in children < 2 y/o DX: bx, g stain TSS: staph/strep toxin Risks: foreign bodies (tampons, nasal packing, trauma, wounds/burns) Sx: shock, ↓BP ↓BV multisystemic organ failure (3 + organ systems involved) Non-dependent edema on face, hands, feet DX: g stain of wound + BX (increase in lactic acid, decrease in perfusion) Toxic Erythema Nodosum “painful, tender, deep nodules on ant. Legs in sub-q fat” Felt on palpitation, lesions change in color- “purple brown yellow green” Dx: CRP, WBCs, CXR to r/o sarcoidosis There is a spontaneous resolution in 6 weeks does not breakdown or ulcerate Xerosis: dru skin (rough, scaly) Sx: pruritis Atopic Dermatits: type 1 hypersensitivity: IgE/Mast cells histamine + heparin Family hx of atopy Chronic lichenification/fissures Infants = extensor surfaces Adult =flexor surfaces TX: phototherapy Nummular Eczema: “round coined shaped” lesions do Tzank Smear to r/o tinea Dyshidrotic Eczema: chronic vesicular hand-foot dermatitis Vesicles ass. with atopy, stress, hot weather, extreme pruritis “tapioca looking” in clusters TX: burrow wet dressings; Triamcinolone Contact Dermatitis: cell mediated (T cell) Delayed hypersensitivity rxn Poison Ivy/ poison oak occur after 2nd exposure TX: burrow solution/wet dressings with topical or po steroids Statis Dermatitis: due to venous HTN and venous insufficiency Proteins/rbcs deposit in sub-q tissue brown hemosiderin deposits because breakdown of RBCs; found on medial ankles edema on legs (Venous statis/ulcers on medial ankles) DX: Doppler see venous insufficiency Diaper Dermatitis: candida/fungal due to exposure of urine/feces “satellite lesions” TX: nystatin + pt education Perioral Dermatitis- facial/mouth “confluent-papulopustular lesions” Hx: young women w/ prolonged used of topical steroids sprays for asthma Only around peri-oral + nasal-labial folds TX: avoid steroids and give antibiotics Seborrheic Dermatitis: in axilla, groin, face, hands In areas of sebaceous glands IN infants: “cradle cap” – thick/yellow brown greasy scaling In adults: dandruff on scalp, eyelashes, beardm eyebrows TX: selenium sulfide shampoo; ketoconazole shampoo Lichen Simplex Chronicus: end stage of pruritic/eczema hyperplasia (“thick skin”) Hyperpigmentation, hyperkeratosis, plaques with lichenification TX: high potent topical steroids + anti-histamines Psoriasis: genetic T-cell immune rxn Increase in epidermal proliferation hyperkeratosis/ keratinocytes Triggers: stress, class 1 steriods, Koebner rxn SX: salmon plaque w. distinct border w/ silvery white scales On extensor surfaces; “pitting” of nails + Auspitz; bx shows increased mitosis of keratinocytes Lichen Planus: Tcell mediated rxn; destruction of keratinocytes + basal cell layer Pruritic, penis, polygonal, purple, plaque with fine white scales on flexor surfaces Oral lichen planus- lesions on tongue/buccal mucosa “Wickham’s striae” – fine white lines in mouth Seborrheic Keratosis: “pasted on plaque” Brown/black velvety/warty/ plugged follicle Mc in female > 30 y/o Actinic Keratosis: pre-malignant lesions to skin cancer Sx: yellow-brown/dry rough scales TX: topicl 5FU or surgery/debridement Androgenetic Alopecia: mc in males- occipital temporal with frontal thinning Gradual/genetic; mc in Caucasian males Action of androgen on hair follicle (increases in 40s) Mc type of hair loss; ↓ anagen phase w/ ↑ telogen phase Females: central regression (maintain frontal hairline) o Ass. with acne, hirsutism, virilization TX: minoxidil, finasteride Telogen Effluvium- triggered by stress (happens 2-4 months after stress) Anagen effluvium- drug enduced happens immediately (due to chemo) Alopecia areata- hairloss in round areas w/o inflammation No pinpoint dots; “EXCLAMATION POINT hairs” Affects any hair on body; mc in young adults/children If hair regrows- fine grey/white Alopecia totalis- loss of hair on scalp/face Alopecia universalis- loss of all body hair Etiology- T cells ineract with HLA “peri-follicular lymphocyte infiltrate” autoimmunity Hutchinson’s sign: back streak on nail- Melanoma Subungal hematoma: blood under nail b/c of trauma Splinter Hemorrhages: thin longitudinal red subungal lines; sx of infective endocarditis Oncholysis: nail is white, detachment of nail from it’s bed @ distal end Onychomycosis: “2 feet, 1 hand” ass. with tinea manuu + pedis TX: terbinafine Felon: Sub-Q infection of pulp of digit b/c of penetrating injury Etiology: staph/strept TX: I+D Fleas: “breakfast-lunch-dinner” bites on lower legs (hx of pets) Bed bugs: nocturnal (pt feels itchy before sunrise) Bites are also in groups of threes TX: permethrin spray Pediculosis (lice): transferred by fomite, person-person Itching in temporal-occipital lobe TXL permetherin/ pyrethin/lindane Scabies: burrows into hand/groin/axilla/fingers Risk: hospital, nursing home work Lesions in interdigital web spaces May cause secondary rxn from eggs Increased pruritis at night Spiders: 1. Black Widow: black with red hour glass; neurotoxic only- N/V, musclar cramping in back, abdominal 2. Brown Recluse: tissue toxin- fever, chills, N/V/ arthralgia a. Brown w/ yellow head + violin markings b. Sx: “red-white-blue” discoloration skin necrosis Ticks: 1. Dermacentor: causes RMSF neurotoxin 2. Ixodes Scapularis Lymes disease (spirochete) with erythema migrans Cuteneous mets from cancer: 1. Virchow’s noes (left supraclavicular node) 2. Sister Mary Joesph’s- peri-umblical node 3. Paget’s diease- on unilateral breast cancer Acanthosis Nigricans: thickening of skin in neck/axilla/groin May be associated with carcinoma, obesity, Dm, steroid, INH Dermatomyositis: symmetric muscle weakening, abnormal electromyogram, ↑ CK Heliotrope Rash- periorbital; hypopigmenation Gottren papules- over bony prominence on hands Hyperthyroidism: skin is smooth, flushed, mosit, warm Hypothyroidism: skin is dry, cool, pale, brittle hair Scurvy: Vit C deficiency hyperkeratotic ecchymsis like papules on shins Hair twists in corkscrews + breaks easily Sarcoidosis: erythema nodosum- acute/painful panniculitis Inflammation of sub-q tissue on shins African American young women Lupus (SLE): Discoid SLE “scarring plaques with atrophic scars” Subacute- shawl-like annular plaque on sun-exposed area Systemic- butterfly rash w/ photosensitivity Reiter’s Syndrome: “can’t see, can’t pee, can’t dance with me” Conjunctivitis, urethritis, arthritis Scleroderma- autoimmune disease C- calcinosis deposits on skin R- raynaud’s phenomenon (vasospasm) E- esophageal dysmotility S- sclerodactyly- thick fingers T- Telangietasias Peutz-Jeghers: Lentigines on skin, mouth, mucosa Pt has polyps with increased risk for GI Cancer DX: Barium study at 10 and colonscopy at 25 Vitiligo: depigmenation, autoimmune, ass. w/ thyroid diease, Dm, addison’s, lack of melanocytes Xeroderma Pigmentosum: allergy to light Albinism: lack of tyrosinase in melanocytes White skin, white-yellow hair, light blue eyes Ass. with nystagmus Melasma: hyperpigmentation in sun-exposed areas (face) Cholasma: ass. with pregnancy, hormones, disappears spontaneously Neurofibromatosis (genetic): Crow’s sign, Lisch nodules in eyes 1st sign- Café au Lait spots > 3 spots Mortality ass. with cancer Squamous Cell Cancer: malignant; hx of actinic keratosis Risks: UV exposure, outdoor occupation, white skin, HPV virus Sx: ulcerated/ crusted/ hyperkeratotic/ pink-red/ top of ear + nose Basal Cell Cancer: MC skin cancer “translucent pearly papules w/ fine telangiectasia with large black ulcerations Melanoma: enlargement/ elevation of nevi with new mole Asymmetry, irregular borders, least common but most fatal Keloids: hypertrophic scars w/o collagen Opthomology Macula- good for detailed vision/ made of cones Fovea- dense amt of cones Choroid- provides nutrition to retina thru vessels Palpebrae fissure- open btw upper and lower lids Canthus- corners where eyelids meet Ptosis- drooping of eyelids Ectropion- lower lid turns out Entropion- lower lid turns in Proptosis= exophthalmos protruding eyes Hordeolum= sty (mcc: staph) Chalazion- hard, nontender swelling on lid Blepharitis- inflammation on lid margins, dandruff on eye lashes Pinguecula- yellow nodule on conjunctiva Pterygium- intrusion onto cornea of scarring/nodule Scotomas- vision field loss Miosis- constriction of pupil (PNS) Mydrias- dialation of pupils (SNS) Anisocoria- large pupil cannot constrict Adies Tonic pupil- no light rxn Argyll Robertson pupil= small irregular, no light reaction sx of syphilis Cover-uncover test- detects strabismus Strabismus- can not align eyes diplopia 1. Non-paralytic- short muscle pulls eye in 1 direction (deviation is constant) 2. paralytic- paralysis of muscles- deviation depends on direction Esotropia- eye goes in Exotropia- eye goes outward Hypertropia- upward deviation Hypotropia- downward deviation Amblyopia: “lazy eye” because of poor muscle tone Myopia- nearsightedness (can’t see far away) need concave lens Hyperopia- farsighted- can’t see up close (light focuses behind retina) need convex lens Astigmatism- corneal surface not spherical Grave’s disease (hyperthyroidism) lid lad/ exophthalmos Macular Degeneration- MCC of vision loss in US (loss of central vision- gradual) Viral Conjuctivitis: mcc is adenovirus pre-auricular LAD with watery discharge no change in vision, no photophobia Bacterial Conjunctivitis- staph, H. flu, strep pneumo, pseudomonas, gonorrhea, diphtheria sx: yellow-green discharge; crusty eyes sx: chemosis- membranes that line eyelids- surface of eyes of swollen tx: polytrim (tx of choice) mcc of neonatal conjunctivitis- Chlamydia o Tx: Azithromycin + ceftriaxone Allergic Conjunctivitis- IgE, histamines/LT Puffy red conjunctiva, thin watery discharge Cobblestne papillae and no LAD Keratoconjunctivits Sicca (Sjogren’s disease) Dry, red, scratchy eyes with irritation no tear film DX: Schirmer test Pinguecula- caused by trauma, UV exposure, drug windy weather Dacrocystitis- lacrimal sac infection Mcc- staph/strep Chronic- staph. Epidermis/ candidia Sx: red tear sac, swelling, pain with purulent discharge Dx: must do CT scan to r/o tumor Tx: antibiotic- Augmentin (po) with warm compresses Blepharitis: inflammation of eyelid Etiology: bacterial or seborrheic Lacrimal tearing, photophobia, dry flakes on lid; ass. on meibomian gland Hordeolum- sty (eyelid margin) blocked meibomian gland Etiology- staph, painful TX: topical antibitics (bactroban) Ectropion: ass. with CN VII (Bell’s palsy) palsy Drooping eyelid, light sensitive, excessive lacrimation Corneal Abrasion: due to trauma Dx: fluoresicein stain with coabalt blue lamp Tx: remove foreign body with cotton tip applicator Anterior uveitis (iritis)- “ciliary flush w/ small pupils, deep eye pain, photophobia” Posterior uveitis (choroditis)- painless floaters in eye Intermediate uveitis- Cilitis Dx: slit lamp exam Tx: mydriatics/steroids Subconjunctival Hemorrhage- bleeding in eye Cause: blunt trauma; Vision is NOT affect but you need to r/o a ruptured globe Open angle Glaucoma- “PERIPHERAL VISUAL LOSS” Increased cup: disc ratio IOP > 21 Acute Ancle Glaucoma Blurry vision, ocular pain, MID-DIALATED Pupil IOP > 40 Causes: SNS stimulation relaxation of ciliary body pulls on suspensory ligament casues mydraiasis and iris falls forward Cloudy, steamy cornea, halos around lghts DX: Schiotz tonometer TX: iridotomy, pilocarpine (causes myosis), diuretics, timolol Ulcerative Keratitis: 1. HSV-I: dendritic lesions on cornea- see with fluorescien slit lamp exam a. Tx: DO NOT GIVE STERIODS (tx with antivirals) II. Herpes Zoster (shingles) – CN V = ophthalmic branch Hutchinson’s sign- vesicle on tip of nose Tx: antivirals + steroids III. Bacterial Keratitis Sx: purulent discharge, ulceration HYPOPYON- pus in ant. chamber of eye MCC in contact lens users: pseudomonas MC protozoa in contact lens users: Acanthomoeba NON-Ulcerative Keratitis Causes: syphilis, Tb, SLE, viral o TX: topical antibiotics Corneal Ulcer- cx of keratitis corneal scarring Blunt Trauma with Ruptured Globe Sx: pear-shaped, teardrop pupils points to site of rupture Orbital ecchymosis, bloody chemosis, conjunctival hemorrhage Dx: CT scan; slit lamp exam Hyphema- hemorrhage in ant. Chamber (assume ruptured globe) Metal-foreign bodies form “rust ring” MRI: contra-indicated Orbital blowout fx. Sx: ocular pan loss of upward gaze; diplopia Orbital ecchymoss; palpable bony step offs DX: xray of maxillary sinuses: Water’s view Chemical Eye Burn: alkali burn is more damaging Immediate irrigation with Morgan lens Orbital Cellulitis: can lead to meningitis Mcc- staph Sx: painful ocular movement, fever, decreased ocular motility; decreased vision Sx: proptosis, limited EOM, edema DX: CT scan TX: IV antibiotics Retinal Detachment: vitreous fluid lead to more damage (tear flaps) Sx: sudden painless unilateral vision loss “Dark curtain pulled down over vision” Central Retinal Artery Occlusion Ass. wth cardiovascular disease (embolic) Sx: sudden painless unilateral vision loss Pale retina with cherry red fovea Papilledema- caused by venous stasis + HTN Sign of increased IOP Sx: swollen optic disc ratio with blurred margins + loss of vessels Nonproliferatve Diabetic Retinopathy: Hallmark: MICROANEURYSMS- 1st detectable sign Hard exudates, ischema cotton wool spots Leading cause of adult blindess “hazy disc margins” macular edema Flame-shape hemorrhage superficial retinal hemorrhage Dot + blot hemorrhage deep retinal hemorrhage Proliferative: NEOVASCULARIZATION can result in retinal detachment pre-retinal vitreous hemorrhage boat shaped hemorrhage HTN retinopathy: prolonged narrowing of arteries blurred optic disc papilledema retinal streak hemorrhages; AV nicking; copper wiring macular star soft exudates (infarct) Otolaryngology Turbinates: superior: drain thru sphenoid sinus; middle: drain thru paranasal sinus; inferior: drain thru nasal-lacrimal ducts Paranasal sinuses drain thru ostia Parotid duct- Stenson’s duct Submandibular duct- Wharton’s duct Conductive hearing loss- external/middle ear Sensorineural hearing loss- problem with chochlea or nerve (inner ear) Weber’s test- tuning fork on head conductive: lateralized to affected ear sensorineural: lateralzes to unaffected ear Rhinne test- normal if sensioneural hearing loss (AC> BC) abnormal- BC> AC (if conductive hearing loss) Conductive Hearing Loss I. Cerumen Impaction II. Otitis Externa a. Pain on tragus/pinna movement; canal edematous b. Tx: corticosporin otic solution III. Foreign Body- unilateral discharge from ear a. Tx: insect- lidocaine with mineral oil; removal; prophylactic antibiotics IV. Otitis Media- mcc: strep pneumo, H flu, M cat a. Hearing loss ass with children’s speech impairment E tubes b. Tubes if: >3 in 6 months; > 4 in 12 months c. TX: amoxicillin + Sudafed V. Serous Otitis Media (Tm retracted) a. Dx: decreased mobility of Tm b. Tx: Sudafed + antibiotics VI. Tm perforation- from trauma/AOM a. Tx: topical or po antibiotics + tympanoplasty VII. Myringosclerosis- white calcium on Tm VIII. Tympanosclerosis- stiff/fibrosis of Tm IX. Otosclerosis- immobilization of stapes bones @ oval window a. Prevents ossicles from moving (3 bones become 1) b. Sx: low frequency hearing loss + tinnitus tx: hearing aids X. Cholesteatoma- benign lesion behind Tm a. Sx: chronically draining ear (fails to respond to antibiotics tx) b. Tm perforation with cheesy white debris Sensorineural Hearing Loss I. Presbycusis (MCC of sensorineural loss) a. Sx: bilateral, hx of noise trauma, may have tinnitus b. Affects high-frequency hearing loss; worsened by nosiy enviroments II. Acoustic Neuroma (CN VIII tumor) a. Unilateral hearing loss, tinnitus, vertigo, ass. with ataxia b. Brain stem dysfunction; ass. with Bell’s Facial Nerve Palsy III. Meniere’s disease- hearing loss in 40s; increase in endolymph a. Unilateral low frequency hearing loss b. SX: aural fullness, tinnitus, episodic vertigo tx: decrease in salt intake, diuretics, steriods IV. Toxin mediated- drug induced, high frequency loss a. Drugs: ASA, NSAIDS, diuretics, aspirin, chemo Perforated Tm- hx of diving, airplane flight Sx: hearing loss w. tinnitus + purulent otorrhea Acute OM- mc in children b/c ET tubes can lead to conductive hearing loss Mc etiology: strep pneumo, M Cat, H flu Can’t see “cone of light” on Tm TX: antibiotics, tympanometry, AVOID ANTIHISTAMINES Recurrent OM 3 n 6 months, 4 in 12 months Otitis Media Effusion- mc in divers/flights Decrease in Tm mobility or retracted May have hearing loss dx: tympanometry Chronic OM- caused by pseudomonas, proteus, staph SX: fullness of ears/pain, purulent discharge Barotrauma- change in pressure btw inner and outer ear Inability to equalize pressure flying/diving Tx: decongestants, myringotomy, Valsalva (auto-inflation) Mastoiditis- “post auricular fluctuance” Casues: Strep pneumo, M Cat, H flu Edema over mastoid; CT: see bony destruction Labrynthitis- viral infecton Sx: vertigo, hearing loss, decrease in balance, N/V, nystagmus, tinnitus CT: r/o tumor or CVA tx: steroids, sedatives, antivert Vertigo- motion perceived when there is none Causes: peripheral or central brain lesions; CN VIII dysfunction- acoustic neruoma Note: nystagmus is horizontal (rotational) with peripheral lesions Nystagmus is vertical (bidirectional) with central lesions Allergic Rhinoconjunctivitis- IgE + mast cells Sx: sneezing, rhinorrhea, polyps filled with eosinophils, itching + red eyes Risks: family hx of atopy, trees, grass, pollen, ragweed Tx: antihistamines, LT antagonists, steroids, vasoconstrictor eye drops Urticaria- superficial lesions w/ pruritis + blanch with pressure Angioedema- deep in SUB-Q tissue; edema of eyes, lips, hands, feet (puffy and not pruritic) Vasomotor Rhinitis- non-allergic Increase in cholinergic gland activity (PNS dysfunction) Sx: rhinorrhea, all allergy tests are normal, no nasal pruritis, no sneezing Blood vessels contract then dialate to increase mucosal secreation TX: topical anticholinergics, steroids, antihistamines Rhinitis Medicamentosa: overuse of topical nasal decongestants (ephedrine, phenylephrine) Tx: stop nasal medication take oral decongestants Atrophic Rhinits: change in cells: ciliated columnar replaced by stratified squamous Dry nasal turbinates; anosmia-loss of smell OZENA- foul green discharge/ epistaxis Sinusitis- mc is Maxillary Obstruction of ostia or loss of cilia function Risks: recent URI, allergic/chronic rhinitis, polyps Etiology: o Acute- bacterial (strep pneumo, h.flu, viral, fungal) Sx: sinus pain, yellow-green discharge, sinus pressure < 1month o Chronic- anaerobes (staph, strep) > 3months; no fever, dull HA, cough o Fungal- non-fulmnant (increase in eosinophils) only one sinus affected Mc-aspergillosis, usually HIV + Dx: CT (water’s view-maxillary sinus) Cx: osteomyelitis, cellulitis, mucocele, polyps, meninigits TX: antibiotics- Amoxicilln, Decongestants Viral Rhinitis- common cold Etiology: rhinovirus, parainfluenza, coronavrus, adenovirus Incubation: 1-5 days (may last 7-2 weeks) Watery mucosal discharge, sneezing, clear rhinorrhea, low fever, HA TX: antipyretcs, analgesics, decongestants CX: secondary bacterial infection Nasal polyps- small sac, non-tender, grey grape like mass, Risk factor: cystic fibrosis Asthmatic + nasal polyps hypersensitive rxn to ASA Influenza (the flu)- abrupt onset of high fever Sx: myalga, HA, photophobia, N/V/ non-productve cough TX: oseltamivir, zanamivir; flu vaccine (effective 10 days after admin) EBV (mono): transmission via saliva; one infection- life long immunity Incubation: 2-5 weeks Prodrome: LAD, HA, fever, fatgue, splenomegaly Rash with Amoxacillin DX: monospot/ throat culture CX: GBS (Gullan Bare- ascending paralysis) Herpangina- Coxsackie A virus Hand, Foot, Mouth disease vesicular lesions on dorsum of hand/palms (may ulcerate) Sx: acute fever, sore throat, gray-white papulovesciular lesions on red base that ulcer (on soft palate, tonsils, uvula) HSV- herpes Gingivostomatitis/Pharyngitis 1st episode of HSV Sx: cervical LAD, fever, malaise, myalgia, grouped vesicles on red skin on buccal mucosa Tx: acyclovir Gonococcal Pharyngititis G neg diplococcus; sore throat with LAD Risk: sexually active (oral) dx: culture on Thayer Martin Media Diptheria- sx due to toxin only forms pseudomembrane on pharynx CX: aspiration-blocks airwayl; sepsis DX: DpT vaccine q 10 years Peritonsillar Abscess/Cellulitis: Strep pyogenes, H. flu, Strep viridans, Staph SX: TRISMUS, odynophagia, DEVIATED UVULA, peritonsillar swelling with LAD TX: I+D, IV PCN or cephalosporin Retropharyngeal Abscess- deep space infection of neck Posterior to larynx/ trachea; sx: neck pain, stridor, drooling, stiff neck, swelling, LAD, dysphagia TX: IV- PCN CX: pericarditis, airway obstruction Intra-oral ulcerative Lesions (Necrotizing Gingivitis) “Trench mouth”- painful gingivitis/foul breath Risks: tobacco, immuno-compromised, stress, poor hygiene (periodontal disease) Apthous Ulcer- on buccal/labial mucosa Painful small round ulcer with yellow center with red border Oral Candidiasis- Thursh “white plaque on mouth/tongue” can be removed tx: Nystatin Oral Leukoplakia- hyperkeratotosis, precancerous Risks- trauma, alcohol, tobacco White and can not be removed Erythroplakia- red/velvety- more likely to become cancer then leukoplakia Oral Lichen Planus- autoimmune disease Sx: purple, polygonal, papules, pruritic Wickham’s striae- white striations on buccal mucosa Tx: topical steroids, cyclosporine mouthwash Glossitis- red, smooth tongue, painful; causes: nutritional def./drug rxn/dehydration Sialdenitis- infection of submandibular glands Risk: Sjogren’s syndrome- decreased salivation, pus massaged from duct, swelling of gland DX: US Parotidititis- inflammation of Parotid glands (stenson’s); causes: MUMPS sx: preauricular/postauricular LAD Ludwig’s Angina- Cellulitis of submaxillary space, and sublingual and submental spaces Sx: tongue displace, edema, dysphonia, trismus, drooling, stridor Dx: CT, culture tx: IV antibiotics; ICU- b/c risk of airway obstruction Voice Sounds: I. Raspy- harsh voice due to edema with low pitch II. Muffled- talks very low (cause- painful dysphonia) III. Shaky- decreased respiratory force (elderly) IV. Acute hoarseness- mcc: viral infection or vocal trauma a. If vesicles on soft palate- coxsackie virus/herpes Vocal Cord Paralysis- recurrent laryngeal nerve injury; hx of chronic intubation Vocal Cord Lesions- if smooth + paired vocal abuse Leukoplakia on Vocal Cords- premalignant (in smokers, sx of hoarseness w/o pain) Anterior Epistaxis- mc epistaxis (Kiesselbach’s plexus) Hx of digital trauma/ foreign body/ URI/ allergies “unilateral bright red bleeding with no sensation of post-nasal drip” TX: pinch nose and lean forward silver nitrate/lidocaine packing (merocel) Posterior Epistaxis- mc: sphenopalantine artery Risks: HTN, bleeding disorder, cocaine abuse Sx: hemoptysis, hematemesis, no visualzed source “post nasal drip, bilateral bleed with dark red blood” Osler-Weber-Renu: disorder of blood vessels- excessive bleeding Sx: telangiectasias on lips, tongue, nasal mucosa Cx: hemorrhage hypovolemic shock EPIGLOTTITIS- H. flu infection; thumbprint sign; risk of aspiration/blocked airway; TX: surgery to intubate CROUP- parainfluenza, viral URI, steeple sign, tx: nebulizer, epinephrine, steroids Pulmonology Bronchioltis- RSV in children < 2 y/o; sx: wheezing, dyspnea, SOB, apnea; Peaks in winter RSV is a risk factor for asthma + allergies Cx: BOOP- pneumona is interstitial w. scarrng + obstruction Dx of choice- nasal smear Tx: epinephrine, humidfer, hospitalize infant < 6 months Influenza (the flu, most pathogenic-type A) Most infectious disease of human kind; mc in winter Inflammatory mediators: THN-alpha, Interleukin-6 Sx: abrupt fever, dry cough, pharyngitis, high fever, cervical LAD DX of choice- viral culture TX: zanamivir, oseltamivir PNEUMONIA CAP- < 48 hrs of hospital admission; etiology- strep pneumo (mcc), H.flu, Staph, Influenza (viral) Atypical- mycoplasma, Legionella, Chlamydia Nosocominal > 72 hrs in hospital/ nursing home Pathogens- pseudomonas, Ecoli, proteus PNEUMONIA FACTS ………………………………………………………………………………… Mc in winter; viral mc in children; bacterial mc in adults; infants/neonates don’t have classic sx Classic sx: rales, cough, ↑tactile fremitis, ↑ vibrations (+ bronchophony/egophony), breath sounds ↓, dullness to percussion, chest pan DM- strep, staph Sickle Cell- strep pneumo, H. flu COPD- Strep pneumo, H.flu, M Cat HIV- Tb, PCP Alcoholic- Klebsiella/ anarerobes Neonate- mc is bacterial- strepB, Ecoli, staph (then think viral- CMV, HSV) Infant- mc is atypical (chylamida- has ass. conjunctivitis) Toddler- mc is viral: RSV, adenovirus (then think bacterial- strep pneumo, h. flu) Adult- mc is atypical- mycoplasma/ mcc in adults s strep pneumo DX: CXR (gold standard- but note there may be “lag”- normal CXR with new onset of sx), g stain, sputum culture, WBC TX: o Outpt CAP- macrolide; Outpt CAP w. comorbdities- macrolide + fluroquinolone o CAP w/ hospitalization- fluoroquinolone o Cap in ICU- anti-pseudomonal fluroquinolone + AMG o Nosocominal- anti-pseudomonal fluroquinolone + AMG PICKING THE RIGHT PATHOGEN IN PNEUMONIA……………………………………………… Strep Pneumo: mcc of CAP; g+ cocci in chains; rust colored sputum; tx: PCN H. flu: pleomorphic g- coccobacilli; tx: cephalosporin, ampcillin Staph Aureus: g+ cocci in clusters; risks: CF, IVDA, can by CAP or nosocominal CXR: empyema, cavitation in lungs tx: Naf, Ox, Clox, Diclox + RIF Klebsiella: g- rod; Nosocomal; risks: Dm, alcoholic; “RED APPLE JELLY SPUTUM” Found in upper right lung fields; tx: 3 gen cephalosporin E. Coli: g- rod tx: 3 gen cephalosporin Pseudomonas: g- rod; RISKS: CF, nosocominal tx: Pipericillin + AMG Anaerobes: risks: poor dental hygiene, aspiration Sx: foul smelling breath/ Bad taste in mouth TX: Clindamycin Mycoplasma pneumonia- walking pneumonia; NO gram stain appearance “Bullous myringitis, skin rash” Mc in young adults (fall-spring) Dx: COLD AGGLUTIN titers tx: erythromycin Legionella- risks: exposure to water source: air-conditioner Dx: Urine Antigen Assay TX: macrolide (erythromycin) Chlaymydia pneumonia- longer prodrome (in neonates) TX: DOXYCYCLINE Chlaymydia psittaci- hx of exotic birds TX: DOXYCYCLINE M. Cat- g- diplococci + pre-existing lung disease TX: Macrolide PCP: HIV + dx: silver sputum stain tx: Bactrim, pentamidine, prednisone Fungal: o Coccidiodes- risks: southwest US o Histoplasma- bat/bird feces; travel to Mississippi-Ohio valley o Aspergillus: immunocompromised; CXR: fungus ball o Cryptococcus: HIV + o Blastomyces: travel to MID-WEST US o TX for all fungual pneumonia: AMPHOTERCIN B Pleuritis: mc sx: localized sharp chest pain which increases with breathing Etiology: young healthy pt wth hx of viral UR DX: pleural friction rub- “grating sound” on stethoscope Pleural Effusion: mc sx: SOB/dyspnea Decreased tacticle fremitus, dullness to percussion HOOVER sign- lagging expansion on affected side Etiology: CHF, liver disease, pneumonia, cancer 1. TRANSUDATIVE pleural effusion- ↑ hydrostatis pressure / ↓ oncotic pressure a. SYSTEMIC factores- capillaries are not inflammated pleural fluid is PROTEIN POOR b. Causes: left CHF, PE, liver cirrohosis, pancreatitis (increase in amylase) 2. EXUDATVE pleural effusion- cappilares are inflamed pleural fluid is Protein rich a. Cause: decreased lymph clearance; pneumonia, lung infecton, empyema, lung cancer DX: CXR- blunting of costophrenic angle; cytology to r/o cancer If continuous effusion tap to remove fluid or pleurodess- fibrosis with chemicals Pneumothorax: SOB, chest pain, decreased breath sounds on affected side 1. primary- no lung disease; tall/thin boys w/ family hx 2. secondary- lung disease (COPD, asthma, TB) 3. Tension Pneumo- due to trauma Mediastinal shift + tracheal deviation; decreased tactile fremitus Hamman crunch: pre-cordial crunching with heart beat TX: immediate needle decompression @ 2nd ICS CXR- visceral-pleural line with increased radiolucency TX: 1. asymptomatic + <15% hemithorax observe 2. symptomatic + < 15 % hemithorax aspiration w/ needle cath 3. Secondary Spontaneous pneumothorax chest tube COPD- #1 risk factor is smoking 1. Chronic Bronchitis- Blue Bloater a. Sx: productive cough x 3 months, rales, ronchi b. CXR: increase in interstitial markings at base c. Risks: overwight, frequent chest infections 2. Emphysema- pink puffer/increased AP diameter; Permanent enlargement of air spaces w/ blebs on CXR a. Centriacinar- mc in smokers; in upper lobes b. Panacinar- mc in PT with alpha-1 antitrypsin deficiency c. Distal Acinar- alveolar ducts/sacs involved; decrease in elastic recoil i. CXR: hyperlucent, small heart, lungs are lucent w/ blebs + flat diaphragm COPD in general: ↓↓ FEV-1 with ↑↑ total lung capacity ↑ residual volume SX: dyspnea, wheezing, barrel chest ↑ AP diameter, clubbing of nails, ↑ rbcs b/c of hypoxa polycythemia Decreased diaphragmatic excursion/ increased + prolonged expiratory time Cx: Cor Pulmonale- right sided heart failure 2 TX that alter the course of disease: o 1. Smoking Cessation o 2. Oxygen therapy > 15 hrs/ day o DRUGS only help: 1. bronchodalators (Ipratropium) 2. Bronchodialators (Albuterol) 3. Theophyline (prevent heart failure) 4. Steriods Pulmonary HTN > 20 mmHg Cor Pulmonale- “right sided heart failure in absence of left” o MCC: COPD, also: lung fibrosis, PE o Causes: right ventricular hypertrophy (increase in afterload/ resistance) o Sx: exertional dyspnea, syncope, hepatomegaly, peripheral edema, ascites, JVD o DX: EKG- right ventricular hypertrophy/ tall P waves, inverted T waves, right axis deviation o CXR: prominent pulmonary vessels with increased pulmonary artery pressure Idiopathic Pulmonary fibrosis Pro-inflammatory state- increases fibrosis O2 perfusion Sx: SOB, DOE, clubbing, cyanosis, fine-late inspiratory crackles at base CXR: ground-glass patchy appearance, honeycombing PFT: restrictive pattern, decreased FEV-1; normal FEV1: FVC ratio DX: BX (gold standard) Sarcoidosis- noncaseating granulomas Young African American Female SX: erythema nodosum on pre-tibial area, lupus-like butterfly rash CXR: bilateral hilar LAD PFT: restrictve pattern (↓ FEV-1 with ↑FEV-1: FVC ratio) Silicosis- DOE, cough, cor pulmonale, clubbing, JVD CXR: egg shell calcifications Risks: sandblasting, quarry work, metal factory, miner, glass Asbestosis- cancer causing (mesothelioma) Sx: DOE, SOB, cough, rales, cor pulmonale CXR: pleural thickening, fibrosis, honey combing pattern Berylliosis- risks: aerospaces/rocket building/ nuclear weapons/ computers/ oil-gas industry Has associated dermatitis rash; dx: BelPT test; CXR: ground glass with hilar LAD TX of SPN: 1. Low CA risk- serial CXR q 3months x 1year then q 6 months x 5years 2. Moderate Ca risk BX 3. HIGH Ca risk surgical resection Malignant: grows 4-8 months Benign: fat n nodule w/ halo sign PE Virchow’s triad: venous stasis, hypercoaguable state, endothelial injury Mc sx: SOB V/Q mismatch Best definitive test: pulmonary angiography TB Risks: homeless, HIV +, endemic areas, crowded living “soft caseous necrosis” with hilar LAD Sx: apical rales, anorexia, weight loss, night sweats, productive cough CXR: ghon’s complex, apical infiltrates w/ cavitations