Advanced Curriculum Development
advertisement

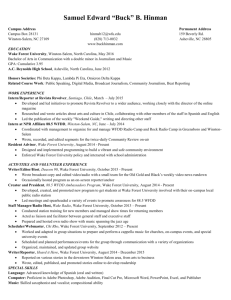
Advanced Curriculum Development: Creating Education Models in Practice Based Learning and Improvement and Systems Based Practice to “Geriatricize” Your Environment Kathryn E. Callahan, MD Helen M. Fernandez, MD, MPH Kirsten Feiereisel, MD William P. Moran, MD, MS Paula M. Podrazik, MD Patty J. Iverson, MA Objectives • Identify the resources, strengths, and needs in your home institution’s educational environment to support the design of a PBLI/SBP curriculum with a geriatric focus • List at least 2 strengths and 2 weaknesses of differing curricular approaches to teaching PBLI and SBP • Generate at least 1 goal and 3 objectives for a curriculum in PBLI/SBP at your home institution • Operationalize the needs, goals, objectives, strengths, and weaknesses of your institution’s educational environment to craft the basics of a curriculum in PBLI or SBP using geriatric content. QI in Ambulatory Geriatrics Implementation of the Practice Improvement Module for Care of the Vulnerable Elderly: CoVE PIM Care of the Vulnerable Elderly Practice Improvement Module (CoVE PIM) Wake Forest School of Medicine CoVE Sites Downtown Health Plaza (IM) Piedmont Plaza (FM) OPD Clinic (IM) Wake Forest School of Medicine Implementing the CoVE PIM Phase 1: Collect practice data to evaluate performance measures All PGY-2’s perform a medical record audit on at least 5 older patients in their continuity clinic panel • • Family Medicine- incorporated into clinic experience Internal Medicine- incorporated into inpatient geriatrics At least 25 patient surveys per practice Submit 1 practice site survey Wake Forest School of Medicine Implementing the CoVE PIM Phase 2: Implement Quality Improvement Project All PGY-3’s review ABIM aggregate data report Develop, implement and evaluate a quality improvement project to target deficiencies One project per site Wake Forest School of Medicine CoVE PIM: Internal and Family Medicine • 2009 Cohort: • 35 residents completed Phase Two. • OPD: 12 residents; 60 charts audited; 25 patient surveys. • DHP: 13 residents; 65 charts audited; 30 patient surveys. • FM: 10 residents; 60 charts audited; 56 patient surveys. • 2010 Cohort: • 38 residents completed Phase One (10 FM/28 IM). • Phase Two starting Fall 2011. • 2011 Cohort: • 38 residents, beginning Phase One. Wake Forest School of Medicine CoVE PIM, operationalized: • IM: Two teams (OPD and DHP), each with: • 2 faculty mentors • 3 Resident Leaders: Team Leader, Communication Czar, Interdisciplinary/Staff Liaison • Additional roles defined as project develops (e.g., Information Technology Liaison, Literature Reviewer) • FM: Two teams, each with: • 1 faculty mentor • 1 Chief Resident Wake Forest School of Medicine CoVE PIM: IM 2009 Cohort Impact • Leadership roles inspire Geriatrics interest: • Team Leaders presented at Grand Rounds • Team Leaders plan Geriatrics fellowship • Systems-Based Practice Outcomes: • Resident-designed Geriatrics Screening Template in hospital-wide EMR • Interdisciplinary team leadership experience • Practice-Based Learning Outcomes: • “I didn’t realize there were guidelines for older adults!” • “I laminated the Falls Algorithm and posted it…” Wake Forest School of Medicine Experiential and Longitudinal QI Curriculum for Geriatrics Fellows • Didactic: QI Curriculum • Application: Practice Improvement Module for Care of the Vulnerable Elderly (CoVE-PIM) • Assessment: – Pre- and Post-Test with the Quality Improvement Knowledge Application Tool (QIKAT) – Structured Interview with fellows – Audit and Feedback with mentored QI project QI Curriculum • Institute of Healthcare Improvement – Courses designed by IHI: self-paced • • • • • • QI 101: Fundamentals of improvement QI 102: The Model of Improvement QI 103: Measuring for improvement QI 104: Putting It All Together QI 105: Human side of QI QI 106: Level 100 tools – Each session duration time is from 30 minutes to 1 hour QIKAT • Assesses prior experience with QI • Three scenarios reflecting quality of care problem: – Identify aim of improvement project – Appropriate measures – Desired outcome for scenario • Assesses attitudes: – Does learner feel QI is essential to future career? – Does learner possess confidence in his/her ability to bring about change? Practice Improvement Module Holmboe et al. JCEHP 2006; 26: 109-19. Curriculum, continued • Fellows reviewed the needs assessment • Three small groups (clinic day); presented ideas for QI projects • Single project identified (cognitive screening) and implemented • Outcomes: – Re-measure process indicator – QIKAT post-test – Qualitative interview with fellows Curriculum for the Hospitalized Aging Patient CHAMP Teaching PBLI/SBP: Incorporating CHAMP Teaching Tools into your Curriculum Paula Podrazik, MD Program Director, Geriatrics Fellowship University of Arkansas for Medical Sciences CHAMP developed at the University of Chicago Supported by a D.W. Reynolds Foundation educational grant 16 http://champ.bsd.uchicago.edu 17 Process Mapping as a teaching tool ”The first step is to draw a flow diagram then everyone understands what his job is. If people do not see the process, they cannot improve it.” W.E. Deming, 1993 A process map or flowchart is a picture of the sequence of steps in a process as it actually occurs. Can be a “higher level” or “drilled-down” view of the process. • In the health care industry useful for – Planning a project – Describing a process – Documenting a standard way for doing a job – Building consensus about the process & correct misunderstandings • In resident & student teaching useful for – Teaching about PBLI– holding the “mirror ” to your practice – Teaching about SBP-understanding the “village” that delivers care CT Abd. needed EMR order Stat? YES Process map of a clinical care issue— ”higher level” process view Call Radiology Tech. NO Patient transported Exam Completed Teaching Case Audit Case Audit: What is it? A structured review of clinical care across a single patient’s hospital stay ▪ ▪ ▪ ▪ Addresses a relevant clinical issue Accepted quality measures exist Performed by the team Fits PBLI construct Inouye S, et al. Ann Intern Med 1992; 119:474. Inouye S., et al. Ann Intern Med 1990; 113:941. Inouye S, et al. JAMA 1996; 275:852. From Whelan, Podrazik, Johnson. Semin Med Pract 2005; 8:70. Developed by Dr. Podrazik @ University of Chicago. Teaching Census Audit Census Audit: What is it? A review of clinical care across patients ▪ ▪ ▪ ▪ Addresses a focused clinical issue Simple quality measures exist Performed by the team Fits PBLI construct From Whelan, Podrazik, Johnson. Semin Med Pract 2005; 8:71. Developed by Dr. Whelan @ University of Chicago. MUSC Aging Q3 http://mcintranet.musc.edu/agingq3 Knowledge to Performance Academic Detailing Resident Cue Participation Falls 9/8/09 – 12/14/09 Activity n (%) Faculty attending in-service Residents attending didactic Detailing encounters 17/27 (77.8%) 37/100 (37%) Detailed 86/100 (86%) Skill - TUG 64/100 (64%) Teaching Attendings detailing Teaching Attendings observing skill - TUG Based on all Teaching Attendings: 18/21 (85.7%) 13/15 (87%) EMR Template