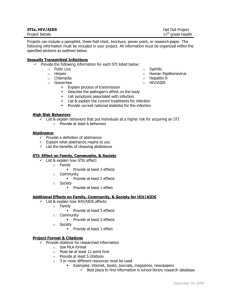
Infectious & Communicable Diseases
advertisement

Infectious & Communicable Diseases Chemeketa Community College 1 Are we at risk? Patient contact Co-workers Hygiene Hazardous scenes 2 Overview Infectious diseases affect entire populations Important to understand population demographics Their ability to move internationally Age distributions Socioeconomic considerations Genetic factors Study of an infectious disease cluster is regional; consequences may be international. Think of consequences of person-toperson contacts 3 World map according to land mass World According To Global Population World Map Showing People With HIV Reflections of Health Care Spending Public Health Agencies Local – that’s YOU! State Health dept Federal US DHS CDC & P • Monitors • Studies & researches • Manages OSHA 8 Agency responsibility relative to isolation from exposure Exposure plan Maintenance and surveillance Appointing a DO Schedule of standards implemented PPE • • • • • gloves protective eyewear face shields masks gowns 9 BSI Procedures for evaluation of circumstances and counseling Personal, building, vehicular, equipment disinfection and storage Correct handling Correct disposal After action analysis 10 Guidelines, Recommendations, Standards, Laws PPE must be available to all employees at high risk All employees must be offered HB vaccine All high risk employees must be offered protection from bloodborne pathogens including TB testing, measles vaccination. 11 Host Defense Mechanisms Nonspecific and surface defense mechanisms Flora Enhances effectiveness of surface barrier by interfering with establishment of agents Can be responsible for infection Skin Intact skin defends against infection by: • Maintaining an acidic pH level • Preventing infection 12 Host Defense Mechanisms Gastrointestinal (GI) System Resident bacterial flora provides competition between colonies of microorganisms for nutrients and space; helps prevent proliferation of pathogenic organisms Stomach acid may destroy some microorganisms Eliminates pathogens through feces 13 cont. Host Defense Mechanisms Upper Respiratory system Turbinates Mucous Mucociliary escalator Normal bacterial flora Lymph tissues of tonsils and adenoids permit rapid local immunological response 14 cont. Host Defense Mechanisms Genitourinary (GU) tract Natural process of urination and bacteriostatic properties of urine help prevent establishment of microorganisms in GU tract Antibacterial substances in prostatic fluid and vaginal fluid help prevent infection in GU system. 15 cont. Host Defense Mechanisms Internal Barriers Protect against pathogenic agents when external lines of defense are breached. Include Inflammatory response Immune response 16 cont. Inflammatory response A local reaction to cellular injury Generally protective and beneficial May initiate destruction of the body’s own tissue 17 Three separate stages Cellular response to injury Decreasing energy stores Cell membrane deteriorates, begin to leak Vascular response to injury Capillary permeability increases, = edema Leukocytes collect Phagocytosis Leukocytes engulf, digest, destroy invaders 18 Immune response Possesses self-non-self recognition Produces antibodies------Some lymphocytes become memory cells Is self-regulated to activate only with invading pathogens IgG IgM IgA IgD IgE 19 Immune response cont. B-cells Produces antibody T-cells Processes antigen for B-cell, Killer T cells are stimulated to multiply by presence of antigens on abnormal cells Helper T cells turn on activities of killer cells Suppressor T cells turn off action of helper and killer T cells Inflammatory T cells stimulate allergic reactions, anaphylaxis, autoimmune reactions 20 Approach to a call Wear appropriate PPE Patient Assessment: Focused history and physical History of present illness • • • • • • Onset - gradual or sudden? Fever Antipyretic usage (ASA, APAP) Neck pain or rigidity? Difficulty swallowing, secretions? How did sx change over time? 21 Approach to a call cont. Past medical history Chronic infections, inflammation Use of steroids, antibiotics Organ transplant and associated medicines Diabetes or other endocrine disorders COPD or respiratory complications 22 Detailed History and Physical Assess skin for temperature, hydration, color, mottling, rashes, and petechiae Assess sclera for icterus Assess patient reaction to neck flexion Assess for lymphadenopathy in neck Assess digits and extremities for purulent lesions 23 After the Call Upon disposition of patient, dispose of supplies, bag linen, disinfect ambulance and equipment Reprocessing methods for EMS durable equipment • • • • Sterilization High-level disinfection Intermediate-level disinfection Low-level disinfection 24 Stages of an infectious disease Stage of Disease Begins Ends With invasion When agent can be shed Communicable period When latent period ends Continues as long as agent is present Disease period Follows Of variable incubation period duration Latent period 25 The Ryan White Act Ryan Wayne White 1971 – 1990 Dx - Hemophilia at 3 days old Tx - Factor VIII and blood transfusions 1984 – Dx - AIDS 1990, 1996, 2000, 2006 – Ryan White law passed 26 What does it mean? Funding for HIV/AIDS treatment Health care provider employees must be notified within 48 hours if an exposure is found to have occurred. Employers must name a DICO to coordinate communications between hospital and agency 27 Ryan White Act - 2006 Staffers removed provisions of bill dealing with Emergency Responders Hospitals no longer required to test or reveal results within 48 hours Efforts to reinstate underway 28 Individual Responsibilities Be familiar with laws, regulations Proactive attitude – infection control Maintain personal hygiene Attend to wounds Effective hand washing after every patient contact Remove or dispose of work garments- handle uniforms properly 29 Individual Responsibilities Handle and launder soiled work clothes properly Prepare food and eat in appropriate areas Maintain general and psychological health Dispose of needles and sharps appropriately Don’t wipe face and/or rub eyes, nose, mouth etc. 30 Pathophysiology Infectious Agent •Virulence •Dosage Means of Transmission Host •Host Resistance •Protective Measures •Direct •Indirect Routes of Exposure •Airborne •Bloodborne •Foodborne (Fecal/Oral) What’s That Mean Exposure does not necessarily equal infection The chain of elements must be intact Transmission can be controlled 32 We’ll talk about... HIV Hepatitis A Hepatitis B Hepatitis C Hepatitis non-ABC Tuberculosis Meningococcal meningitis Pneumonia Rabies Hantavirus Chicken pox Mumps 33 And these too Rubella Measles Whooping cough Influenza Mononucleosis Herpes simplex Syphilis Gonorrhea Chlamydia Scabies & Lice Lyme disease Gastroenteritis 1&2 34 Infectious agents Bacteria Prokaryotic • Nuclear material is not contained within a distinctive envelope Self-reproducing without host cell – BUT require host for food, support S/S depend on cells and tissues infected 35 Toxins - often more lethal than bacterium Endotoxins Exotoxins Can be localized or systemic infection 36 Viruses Eukaryotic • Nuclear material contained within a distinct envelope Must invade host cells to reproduce Can’t survive outside of host cell 37 Other Microorganisms Prions Slow viruses – particles of protein • Accumulate in nervous tissue and brain tissue Mad Cow Disease Fatal familial insomnia Alzheimers Disease Parkinsons’ Disease 38 Fungi Protective capsules surround the cell wall and protect fungi from phagocytes Broad-spectrum antibiotics can cause fungal infections • Pneumonia • Yeast infections 39 Protozoans Single-celled microorganisms More complex than bacteria Live in soil – opportunistic infections – fecal-oral or mosquito bites Malaria Some forms of Gastroenteritis Trichomoniasis (STD) 40 Parasites – Helminths (worms) Roundworms Live in intestinal mucosa S/S – abdominal cramping, fever, cough Pinworms Common in US • 20% of children in temperate climates are infected Live in distal colon S/S – anal itching Hookworms 25% world population – rare in US • Walking barefoot in contaminated area • S/S – epigastric pain, anemia 41 Human Immunodeficiency Virus (HIV) - Slim Disease Present in blood and serum-derived body fluids Directly transmitted person-person Indirectly transmitted via Blood transfusion, organ transplant, contaminated needles 42 Adults and children estimated to be living with HIV/AIDS as of end 2006 2002 North America 1,200,000 980 000 Caribbean 440 000 540,000 Latin America 2,000,000 1.5 million Eastern Europe Western Europe & Central Asia 1.2 million 570 000 1,800,000 East Asia & Pacific North Africa 1.2 million 1,800,000 South & Middle East & South-East Asia 600,000 550 000 8,000,000 6 million 700,000 Sub-Saharan Africa 30,000,000 29.4 million Total: 44 42 million 00002-E-4 – 1 December 2002 Australia & New Zealand 15 000 750,000 45 46 Spread of AIDS in Africa Various stats about Africa: - Sub-Saharan Africa has 10 percent of the world’s population but is home to more than 60 percent of all people living with HIV and AIDs - In 2005, 3.2 million people in the region became newly infected, while 2.4 million adults and children died of AIDs Likelihood of contacting the HIV virus per 10,000 exposures: Blood Transfusion 9,000 - 90% chance, Childbirth 2,500 - 25% Chance, Needlesharing injection drug use 67 - 0.67% Chance, Percutaneous needle stick 30 0.3% Chance, Anal intercourse 50 - 0.5% Chance, Penile-vaginal intercourse 10 0.1% Chance, Oral intercourse 1 - 0.01% Chance Many countries have over 15% of their adult population carrying the virus. Swaziland - People Living with HIV/Aids: 220,000 - Population with HIV/Aids: 38.8% Botswana - People Living with HIV/Aids: 350,000 - Population with HIV/Aids: 37.3% Lesotho - People Living with HIV/Aids: 320,000 - Population with HIV/Aids: 28.9% Zimbabwe - People Living with HIV/Aids: 1,800,000 - Population with HIV/Aids: 24.6% South Africa - People Living with HIV/Aids: 5,300,000 - Population with HIV/Aids: 21.5% Namibia - People Living with HIV/Aids: 210,000 - Population with HIV/Aids: 21.3% Zambia - People Living with HIV/Aids: 920,000 - Population with HIV/Aids: 16.5% Malawi - People Living with HIV/Aids: 900,000 - Population with HIV/Aids: 14.2% United States - People Living with HIV/Aids: 984,000 - Population with HIV/Aids: 0.6% 48 Statistics US- >1,185,000 through 2003 Most 25-49 y/o 24-27% undiagnosed HIV 2005- est. 45,669 AIDS dx Oregon – 5,855 through 2005 2005 – 284 new cases (AIDS primary Dx) New York, California, Florida leading 49 As of the end of 2006… 44 million people worldwide were living with HIV/AIDS. 3.5 million of these are children Approx. 50% of adults living with HIV/AIDS worldwide are women. 6.5 million HIV infections worldwide occurred in 2005 alone - 18,000 day. 40,000 new HIV infections/yr in the U.S, half are younger than 25 years of age (70% men, 30% women). 50 By the end of 2006… 30 million people have died of AIDS worldwide. 14 million orphans have been left behind. 51 AIDS Origins - First Reports In Africa - First known case! Man in Republic of Congo died in 1959, had his blood frozen for an immunology experiment. In the U.S: A 15-yr old male prostitute died of Kaposi’s Sarcoma in 1969. Frozen tissue sample had HIV antibodies - not reported until 1999. In Europe: A Danish surgeon who had worked in Zaire. She died mysteriously in 1976. 52 First reports, cont…. June 1981: reports of new disease in male homosexual community in U.S. 5 men in LA area diagnosed with PCP (pneumocystis carinii pneumonia), a type of pneumonia carried by birds. Very unusual, since PCP is usually only found in profoundly immune-suppressed patients. 53 First Reports (Cont.) July 1981: reports of Kaposi’s sarcoma (KS), a very uncommon cancer, found in 26 gay men in NYC and California. Very unusual, since KS had only been seen in older men of Jewish or Italian ancestry (mostly in lower legs). 54 At the same time… 1982: Similar cases outside the U.S. (Zambia, Uganda). 1983: Zaire. Soon cases were identified in all Western European countries and in Australia, New Zealand, and parts of Latin America (Brazil, Mexico). 55 Origins of AIDS - What we know There are two types of the virus: HIV-1 and HIV–2. HIV-1 appears to have spread from Central Africa. HIV-2 has so far been confined mainly to West Africa. 9 of the 11 known sub-types are found in the Republic of Congo probable origin. 56 Causative agent - HIV-1 & HIV-2 Seeks cell receptor CD4+ T cells Found on surface of T helper cells Both types are seriologically distinct but share similar characteristics HIV infected T-cell 57 Origin of HIV-1 Cross-species transmission from chimpanzee (Pan troglodytes troglodytes). Simian virus closely related to HIV jumped from monkeys to humans, later mutated into current form SIVcpz. Genetic evidence (75-85%). Several species of monkey carry HIV-like simian viruses. Believe virus jumped at least 8 times from ape to human. 58 Origin of HIV-1, cont. Consumption of “bushmeat” The slaughter and selling of monkey body parts provides families with meat and income. This is a long-standing practice - but has decreased in the past few decades due to: Commercial logging driving out animals. Bans on hunting/trading simian body parts Better roads, easier access to other food. The blood-to-blood contact of killing these animals is a prime suspect in humans acquiring the HIV virus. 59 HIV-1 is far more pathogenic; most cases world-wide are HIV-1, Group M First case in US of HIV-1, Group O, identified in 6/96 HIV-antibody tests in US detect HIV-1 Group M, with 99% accuracy; HIV-1 Group O with 50-90%. HIV-2 – milder symptoms, slower development – mainly in West Africa. US cases: 79 60 Why The Rapid Spread? International Travel 'Patient Zero‘ - Gaetan Dugas Analysis of several of the early cases of AIDS infected individuals were either direct or indirect sexual contacts of the flight attendant. The Blood Industry In some countries such as the USA paid donors were used, including intravenous drug users. • This blood sent worldwide. • Also, in the late 1960's hemophiliacs benefit from Factor VIII. To produce the coagulant, blood from thousands of individual donors had to be pooled. 61 Why The Rapid Spread? Drug Use The 1970s - increase in availability of heroin following the Vietnam War and other conflicts in the Middle East, The development of disposable syringes and the establishment of 'shooting galleries' provided another route. What other theories have there been about the origin of HIV? Conspiracy theories - manufactured by the CIA vs genetically engineered. 62 Occurrence highest: High-risk sexual behavior IV drug and steroid abuse Transfusion recipient between 1978-1985 Hemophilia or other coagulation disorders requiring blood products Infant born from HIV-positive mother Other factors Coexisting STD’s (esp. with ulceration) Penile foreskin 63 Why all the fuss over AIDS? AIDS is killing over 3 million people each year worldwide. No other disease is spreading at this rate. 64 Why all the fuss over AIDS? It has an extraordinary capacity for change and rapid global spread. Hard to make a vaccine. There is a long asymptomatic period between infection and illness. Can be passed on during this period. Many people with disease seem outwardly healthy. 65 Why all the fuss over AIDS? HIV/AIDS is more serious than many common diseases because of the age groups it attacks. Mainly kills people in their 20s to 40s society’s most productive group. 40% increase in 14-22 age group 70% are unknown carriers Death of these young people has left behind 14 million AIDS orphans. 66 Why all the fuss over AIDS? Therapy: HIV/AIDS requires the use of some of the most EXPENSIVE and TOXIC drugs in medical history. $2,000 - 4,000 per month Need to be 98% compliant to be effective 67 Initial case definition established by CDC in 1981. 1987 & 1993; s/s include tuberculosis, recurrent pneumonia, wasting syndrome, HIV dementia, sensory neuropathy. 68 69 Classifications & Categories Category A Acute retroviral infection 2-4 weeks after exposure Mono-like illness; lasts 1 – 2 weeks • Fever • Adenopathy • Sore throat 70 Transient decrease in CD4+T cell counts Seroconversion; 6-12 weeks after transmission • CD4+T cell count return to normal levels Asymptomatic infection; persistent generalized lymphadenopathy; gradual decline in CD4+T cell count 71 Category B Early symptomatic HIV Decreased CD4+T cell count Common complications • Localized Candida infections • Oral lesions • Shingles • PID • Peripheral neuropathy • Fever/Diarrhea lasting more than one month 72 Category C Late symptomatic HIV Represents all AIDS-defining diagnoses CD4+T cell count 0 to 200 per uL Severe opportunistic infections • Bacterial pneumonia (Pneumocystis Carinii Pneumonia) • Pulmonary tuberculosis • Debilitating diarrhea • Tumors in any body system, including Kaposi’s sarcoma • HIV-associated dementia Advanced HIV: CD4+T cell counts 0-50 per uL. 73 Nervous system - toxoplasmosis of CNS Immune system - major site of compromise Respiratory system pneumocystis carinii pneumonia Integumentary system - Karposi’s sarcoma 74 13-30% transmission to infants born to HIV-infected mothers Breast feeding can result in HIV transmission Virus has occasionally been found in saliva, tears, urine, bronchial secretions. Vector transmission has not been known to occur. Risk of oral sex is not quantified; believed low. 75 Patient management Out-of-hospital care - supportive. BSI as appropriate Effective hand washing Use of eye protection, masks and gowns highly recommended when exposure to large volumes of body fluids. 76 HCW infection: Non-intact skin exposure (6/2000) – 56 + 138 ? Susceptibility and resistance Infectiousness may be high during initial period after infection and at endstage Race and gender are not risk factors for susceptibility. 77 Care in use of medical equipment mandatory Disinfection of equipment mandatory Early diagnosis, treatment, counseling for health-care providers is mandatory. 78 HIV testing OraQuick Rapid HIV 1 / 2 test Oral fluid, plasma, whole blood 20 – 40 minutes Accuracy • Positive – 99.3% • Negative – 99.8% 79 80 Post-exposure prophylaxis < 72 hours non-occupational exposure Highly active antiretroviral therapy (HAART) • PMPA (tenofovir) – 28 days Repeat testing 4-6 weeks after exposure; again at 3 months, 6 months, 1 year 81 WHO Recommendations for a First Line Regimen in Adults and Adolescents • d4T+3TC+NVP • ZDV+3TC+NVP • d4T+3TC+EFZ • ZDV+3TC+EFZ d4T (NRTI) alternative name Stavudine ZDV (NRTI) alternative names Zidovudine or AZT EFZ (NNRTI) alternative name Efavirenz NVP (NNRTI) alternative name Nevirapine 3TC (NRTI) alternative name Lamivudine 82 Hepatitis A viral disease Produces pathologic alterations in the liver 83 Hepatitis-A Causative agentHepatitis A virus Most common type of viral hepatitis Once infected, person is immune to HAV for life 84 Statistics Oregon 2005 – 1.3/100,000 (49 new cases) 1955 – 86.7/100,000 Marion County: 632 Multnomah County: 1,512 National – 1/3 of Americans show past infection (immunity) 85 Many infections asymptomatic Liver may be affected Often occurs without jaundice, esp. children Only recognizable by liver function studies Only hepatitis virus that does not lead to chronic liver disease or chronic carrier state. 87 Routes of transmission Stool of infected person Contaminated water, ice or food Sexual and household contact can spread virus Can survive on unwashed hands for 4 hours 88 Susceptibility and resistance No clearly defined populations at increased risk. 75% of people with H-A have sx. In developing nations with poor sanitation, infection is common In developed nations, often associated with day care, nursing homes 89 S/S Onset is abrupt with fever, weakness, anorexia, abdominal discomfort, nausea and darkening of urine, sometimes followed w/in a few days by jaundice/icterus. Mild severity lasting 2-6 weeks. Rarely serious. 90 Patient management Care is supportive for fluid intake and prevention of shock. Person is most infectious during first week of symptoms BSI mandatory. 91 Immunization Prophylactic IG may be administered within two weeks after exposure If traveling to Africa, the Middle East, Central and South America, Asia - get immunized. 92 Hepatitis A vaccine available for 2 y/o or older Close contact with people who live in areas with poor sanitary conditions Male-male sex Illicit drugs Children in populations with repeated epidemics Chronic liver disease or clotting factors disorders 93 Hepatitis-B Causative agent - H-B virus. Potential secondary complication - liver necrosis HBV usually lasts < 6 months Carrier state may persist for years 94 Statistics National – 60,000 new infections (2004) Oregon – 2005; 99 cases acute HB 404 cases chronic carriers Marion County: 195 Multnomah County: 556 95 Routes of transmission Blood, semen, vaginal fluids, saliva, blood transfusion, dialysis, needle and syringe sharing, tattooing, sexual contact, acupuncture, communally-used razors and toothbrushes. HBV stable on environmental surfaces > 7 days Transmission by insects and fecal-oral route not demonstrated. 97 S/S Within 2-3 months, infected persons gradually develop non-specific symptoms such as anorexia, n/v, fever, joint pain, generalized rashes, sometimes jaundice. Risk of developing chronic infection varies inversely with age. 98 1% of patients develop full-blown liver crises and die with mortality increasing > 40 y/o. 5-10% infected people become asymptomatic carriers. 99 Patient management Out-of-hospital - supportive BSI Effective handwashing Care in use of equipment. Careful handling of sharps High-level disinfection of equipment esp. laryngoscopy blades is mandatory. 100 Immunizations: Recombivax HB and Engerix B are effective. Vaccines: initial, onemonth, six-month provide long-lasting immunity in 95-98% of cases. Postexposure prophylaxis HBV vaccine HB IG 101 Hepatitis C Causative agent - H-C virus. Organ affected - liver. Most frequent infection secondary to needlestick & sharp injury 85% infected healthcare workers become chronic carriers 102 Health care workers - 2.7 - 10% probability of infection when exposed to contaminated blood. Transmission by household and sexual contact low. Can’t occur from food and water. 103 Statistics Oregon: 2005; newly reportable; 1,337 July-Dec. (chronic) – 50 acute cases Marion County: 4 Multnomah County: 17 National – new infections per year has declined (240,000 in 1980’s – 24,000 in 2004) 104 S/S Same as for HBV but less progression to jaundice Chronic liver disease common with >80% developing chronic liver disease. Apparent association between HCV infection and liver cancer 106 Patient management Same as for HBV Immunization: Prophylactic administration of IG not supported by current data Post exposure testing important Vaccine may be available 107 Hepatitis non-ABC Hepatitis D; infects a cell with other hepatitis virus When virus active in HBV patients, resulting disease extremely pathogenic Hepatitis E not bloodborne; is spread like H-A 108 Hepatitis G - newly identified Major epidemics documented in young adults. Women in 3rd trimester especially susceptible to liver disease 109 S/S Onset abrupt with s/s resembling HBV Always associated with HBV Patient management Same as for HBV Immunization HB vaccine can indirectly prevent H-D, but has no effect on H-E. 110 Tuberculosis Causative agent mycobacterium tuberculosis 8 million new TB/yr worldwide 3 million die of disease 111 TB Epidemic in US Immigration Transmission in high-risk environments • Prisons, homeless shelters, hospitals, nursing homes • National – 1953; 84,350 – 19,707 deaths 2005; 14,097 – 662 deaths Oregon: 106/100,000 (11/03) 103 - 2005 112 Rate of TB for HIV patients 40x rate of TB for non-HIV persons Routes of transmission: Airborne droplet Prolonged exposure to infected person Reservoirs include some cattle, badgers, swine 114 Susceptibility and resistance Period of incubation 4-12 weeks. Period for development of disease 6-12 months after infection. Risk of developing disease highest in children < 3, lowest in later childhood and high among adolescents, young adults and elders. High in immuno-compromised patients; HIV-infected, underweight, undernourished. 115 S/S: First infection usually subclinical These bacteria lie dormant but can reactivate into secondary TB Most common site of reactivation TB is in apices of lungs. Patients present with chronic productive/non-productive cough (persistent for 2-3 weeks), low-grade fevers, night sweats, weight loss, fatigue Hemoptysis common. 116 Body systems affected; Indirectly affects respiratory system including larynx Left untreated, TB can spread to other organ systems and cause other sx. Cardiovascular; pericardial effusions may develop Skeletal: Generally affects thoracic and lumbar spine, destroying intervertebral discs Chronic arthritis of one joint is common CNS Causes a subacute meningitis and forms granulomas in brain 117 Patient care Primarily supportive Prevent shock 118 Routine evaluation of Health care workers PPD (purified protein derivative) • Positive reaction indicates past infection CXR Sputum stain and culture Remember; TB is communicable with prolonged exposure to droplet infection. 119 Drug therapy Prophylactic INH; recommended routinely for persons <35 y/o who are PPD positive; not recommended > 35 due to hepatic complic. Therapeutic: Isoniazid, Rifampin, Pyrazinamide, Streptomycin Side effects of INH Paresthesias, seizures, orthostatic hypotension, N/V, Hepatitis 120 Meningococcal meningitis Causative organism: Neisseria meningitidis, meningococcus Tissues affected: Colonize lining of throat and spread easily through respiratory secretions Est. 2-10% of population carriers, but are prevented from illness by throat’s epithelial lining. 121 Statistics Oregon – 2005: 56 cases Oregon – 1994 – 2003: 887 Marion County: 111 Multnomah County: 182 122 Modes of transmission: direct contact w/ secretions during intubation, suctioning, CPR etc. 123 S/S: Onset is rapid; Fever Chills Joint pain Neck stiffness or nuchal rigidity Petechial rash Projectile vomiting Headache 124 ~10% may develop septic shock; acute adrenal insufficiency, DIC, coma may result. Death may occur in 6-8 hours. 125 Pediatric patients; infants 6 mo - 2 y/o esp. susceptible; maternal antibodies protect neonates to 6 mo. Infants display nonspecific s/s: Fever, Vomiting, Irritability, Lethargy, Bulging fontanelle High-pitched cry 126 Patient management: Protective measures with surgical masks to patient. Prophylactic tx available; rifampin, etc. Immunizations: especially for older children and adults. 127 Other infectious agents cause meningitis: Streptococcus pneumoniae (bacterial) 2nd most common cause in adults Most common cause of pneumonia in adults and OM in children Spread by droplets, prolonged contact or soiled linen. 128 Hemophilus influenza type B (bacterial) Gram negative rods. Prior to 1981, leading cause of meningitis in children 6 mo-3 y/o. Although tx with antibiotics very effective, >50% infected children have long-term neurological deficits. Implicated in epiglottitis, septic arthritis, generalized sepsis. 129 Viruses (aseptic meningitis) A variety known to cause meningitis Not considered communicable 130 Pneumonia Causative organisms Bacterial Viral Fungal 131 Pneumonia (cont) Systems affected Respiratory - pneumonia CNS - meningitis ENT - otitis, pharyngitis media Routes of transmission Droplet, Direct contact, Soiled linen 132 Susceptibility Pulmonary edema Flue Exposure to inhaled toxins Chronic lung disease and aspiration Geriatrics Pediatrics with low birth weight and malnourishment 133 Other high-risk groups Sickle cell disease Cardiac disease Diabetes Kidney disease Hiv Organ transplants Hodgkins disease Asplenia 134 Statistics 2005 (Tri-county area) – 165 cases Death highest in > 84 y/o 135 S/S Sudden onset chills, high-grade fevers, chest pain with respirations, dyspnea. PEDS: fever, tachypnea, chest retractions are ominous. Purulent exudates may develop in one or more lobes. Patient may have productive cough with yellow-green phlegm. 136 Patient management Several antibiotics effective to treat bacterial pneumonia Protective measures for health-care workers. Immunizations: Vaccine exists for some causes 137 Tetanus Causative organism; Clostridium tetani Live mainly in soil and manure Also found in human intestine 138 Statistics 500,000 cases/year worldwide 45% mortality 100 cases/year in U.S. Patients > 50 y/o Oregon: 1992-2001; 6 Marion County – 1997: 1 139 Affects musculoskeletal system Mode of transmission Wounds, burns, other disruptions in skin. Puncture wounds introducing soil, street dust and animal or human feces. Dead or necrotic tissue favorable environment. 140 S/S Muscular tetany Painful contractions, esp. trismas or lockjaw and neck muscles; secondarily of trunk muscles. PEDS: abnormal rigidity may be first sign. Painful spasms with risus sardonicus Can lead to respiratory failure. 141 Patient management: Support vital functions Valium for muscle spasms Consider paralytics Magnesium sulfate Narcotics Antidysrhythmics Administration of antitoxin - TIG 142 Post exposure of tetanus immune globulin - keep immunizations UTD. Immunizations: Booster before elementary school, every ten years thereafter. 143 Rabies - hydrophobia Acute viral infection of the CNS Causative organism - rabies virus Affects nervous system Route of transmission Saliva from bite or scratch of infected animal. Person-person transmission theoretically possible. Airborne spread in bat caves rare 144 Statistics Oregon; 1994 – 2003; 77 Marion County: 1996 – 2 1998 – 2 2001 – 1 2007 – 4 animals (bats) 145 Hawaii is only area in US that is rabies-free. Wildlife rabies (in us) common in Skunks Raccoons Bats Foxes Dogs Wolves Jackals Mongoose Coyotes. 146 Susceptibility: Mammals highly susceptible. Incubation period usually 3-8 weeks (rare; 9 days - can be as long as 7 years). 147 S/S: Sense of apprehension H/A Fever Malaise Poorly defined sensory changes. Progresses to weakness or paralysis Spasm of swallowing muscles (causes hydrophobia) Delirium Convulsions W/O medical care, disease lasts 2-6 days; often results in death. 148 Patient management: EMS workers; transmission never documented. After bite: Thorough debridement of wound Free bleeding and drainage. Vigorously clean wound with soap and water and irrigate with 70% alcohol. Prophylactic Tetanus vaccine Administration of human rabies immune globulin Over several weeks 149 Hantavirus Known to be associated with hemorrhagic fever with renal syndrome; occurs in Asia. Also associated with a syndrome of severe respiratory distress & shock in Southwestern U.S. Deermouse Transmitted via inhalation of aerosols of rodent urine and feces 150 Statistics Oregon: 1993 – 2003; 5 cases • 2006 – 7 cases NM – 2006 – 68 cases 151 S/S Typically healthy adults Onset of fever and malaise – 1 – 5 weeks later Followed several days later by respiratory distress Fever, Chills H/A GI upset Capillary hemorrhage Kidney failure, hypotension, severe infection may ensue Death from poor cardiac output 153 Severe HPS Evolution of HPS 1 2 Large effusion assoc. w/ HPS 3 154 Patient management Supportive BSI 155 Chickenpox Causative agent; variella-zoster virus (member of the Herpes virus group). System affected; primarily integumentary 156 Statistics 4 million/yr in US Most 1 – 4 y/o • Associated with Daycare 157 Shingles is a local manifestation of reactivation of latent viral infection Mainly airborne Soiled linen implicated. Incubation period 10-21 days 158 S/S: Chickenpox More severe in adults Begins with respiratory symptoms, malaise, low-grade fever. Rash begins as small red spots that become raised blisters on a red base. Eventually dry into scabs. Rash is profuse on trunk Itching Patient management: Isolation until all lesions are crusted and dry. 159 Disease self-limited Complications Secondary bacterial infections Aseptic meningitis Mononucleosis Reye syndrome 160 Mumps Causative agent:Mumps virus Acute, communicable systemic viral disease Glands most commonly affected: Parotid Testes Pancreas 161 S/S: Mode of transmission; droplet spread, direct contact Incubation period; 12-25 days. Immunity general after recovery 30% asymptomatic Fever, swelling and tenderness of salivary glands, esp. parotid. After onset of puberty; • Orchitis • Testicular atrophy 162 Patient management: EMS workers - MMR immunity Patients wear masks Caution with soiled linen 163 Rubella (German measles) Causative agent - rubella virus Mild, febrile, highly communicable disease Systems affected; Integumentary, Musculoskeletal, Lymph nodes 164 Mode of transmission Maternal transmission gravest risk: Congenital heart diseases, eye inflammations, retardation, Deafness (90% of neonates born to mothers infected in first trimester develop congenital rubella syndrome). 165 Congenital anomalies; death from heart disease, sepsis in first 6 month Mental retardation Deafness Person-person contact via mucous secretions 166 S/S: Generally mild; fever, flue sx, red rash that spreads from forehead to face to torso to extremities and lasts 3 days. Serious complications do not occur in Rubella. 167 Patient management: BSI including mask. All EMS workers, especially females should be screened for immunity. No specific treatment. Immunizations: known to be 98-99% effective 168 Measles (rubeola, hard measles) Causative organism - measles virus Highly communicable Systems affected: respiratory, CNS, pharynx, eyes, systemic Mode of transmission - air droplets, direct contact. 169 170 S/S: Prodrome - conjunctivitis, swelling of eyelids, photophobia, high fevers to 105 degrees, hacking cough, malaise 171 A day or two before rash, patients develop small, red-based lesions with blue-white centers in the mouth (Koplik’s spots) sometimes disappearing with generalized skin rash. Rash is red, slightly bumpy and spreads from forehead to face, neck, torso, to feet by 3rd day. 172 Rash usually lasts for 6 days, initially appears thicker over head and shoulders, clears up and follows that pattern toward feet. Pneumonia, eye damage and myocarditis are all possible but most life-threatening is subacute sclerosing panencephalitis Progressive deterioration of mental capacity, muscle coordination 173 Patient management: BSI, including mask EMS workers should be immunized No specific treatment. 174 Pertussis (Whooping Cough) The 100-day cough Causitive organism - Bordetella pertussis Mainly affects infants and young children Affects oropharynx Mode of transmission; direct contact with airborne droplets. 175 S/S: Insidious onset of cough which becomes paroxysmal in 1-2 weeks, lasts 1-2 months. Paroxysms are violent, inspiratory whoop. Whoop often not present in infants < 6 mo., adults Before pertussis vaccine in 1950’s, disease killed more children in U.S. than all other infectious diseases combined 176 Patient management: EMS workers be cautious about handling linens, supplies etc. on all patients with hx of recent onset of paroxysmal cough Transport patient with mask. Communicable period thought to be greatest before onset of coughing. Incubation period 6-20 days. Erythromycin decreases period of communicability, but only reduces sx if given during incubation period. 177 Influenza – the flu Causative organisms; influenza viruses types A, B, C Affects respiratory system primarily Mode of transmission: airborne, direct contact Virus can persist for hours, especially in low humidity and cold temp. Incubation period 1-3 days. 178 S/S: URI- type symptoms which last 2-7 days. Chills Fever Headache Muscle aches Anorexia Fatigue Cough often severe, protracted. 179 Patient management: Supportive Immunizations: Health care workers should be immunized by mid-Sept. (flu season Nov.-Mar. in US). 180 Avian Flu Lots of media coverage In most bird populations More of an issue when in domestic birds Chickens Turkeys Ducks Rarely transmitted to humans Not known to transmit human to human 50% death rate when acquired 181 27 February 2009 Cumulative Number of Confirmed Human Cases of Avian Influenza A/(H5N1) Reported to WHO 2003 Country C 2004 D C 2005 D C 2006 D C 2007 D C 2008 D C 2009 D C Total D C D Azerbaijan 0 0 0 0 0 0 8 5 0 0 0 0 0 0 8 5 Bangladesh 0 0 0 0 0 0 0 0 0 0 1 0 0 0 1 0 Cambodia 0 0 0 0 4 4 2 2 1 1 1 0 0 0 8 7 China 1 1 0 0 8 5 13 8 5 3 4 4 7 4 38 25 Djibouti 0 0 0 0 0 0 1 0 0 0 0 0 0 0 1 0 Egypt 0 0 0 0 0 0 18 10 25 9 8 4 4 0 55 23 Indonesia 0 0 0 0 20 13 55 45 42 37 24 20 0 0 141 115 Iraq 0 0 0 0 0 0 3 2 0 0 0 0 0 0 3 2 Lao People's Democratic Republic 0 0 0 0 0 0 0 0 2 2 0 0 0 0 2 2 Myanmar 0 0 0 0 0 0 0 0 1 0 0 0 0 0 1 0 Nigeria 0 0 0 0 0 0 0 0 1 1 0 0 0 0 1 1 Pakistan 0 0 0 0 0 0 0 0 3 1 0 0 0 0 3 1 Thailand 0 0 17 12 5 2 3 3 0 0 0 0 0 0 25 17 Turkey 0 0 0 0 0 0 12 4 0 0 0 0 0 0 12 4 Viet Nam 3 3 29 20 61 19 0 0 8 5 6 5 2 2 109 54 Total 4 4 46 32 98 43 115 79 88 59 44 33 13 6 408 256 C = Cases D = Deaths West Nile Virus Symptoms Usually mild or no symptoms May have fever Headache Body aches Skin rash Swollen lymph glands May cause encephalitis 183 2005 2008 West Nile Virus Treatment Prevention • Insect repellent Supportive Most return to normal status within 1 year 186 Mononucleosis Causative organism Epstein-Barr virus or cytomegalovirus (both herpes virus family) Body regions affected: oropharynx, tonsils 187 Modes of transmission Person-to-person spread by saliva Kissing Care providers to young children is common 188 S/S: Appear gradually Fever Sore throat Oropharyngeal discharges Lymphadenopathy Splenomegaly Recovery usually in a few weeks, but may take months 189 Patient management No specific treatment No immunization available. 190 Herpes simplex virus type 1 Causative organism: HSV 1 Affects: oropharynx, face, lips, skin, fingers, toes, CNS in infants Mode of transmission: Saliva Skin – skin contact 191 S/S: Cold sores, fever blisters Tx with acyclovir (Zovirax) helpful. 192 Patient management: BSI, including mask Lesions are highly contagious 193 Herpes simplex virus type 2 Causative organism HSV 2 Mode of transmission sexual activity S/S - Males: Lesions of penis, anus, rectum, and/or mouth 194 S/S - Females: Sometimes asymptomatic; lesions of cervix, vulva, anus, rectum and mouth; recurrent disease generally affects vulva, buttocks, legs, perineal skin. 195 Syphilis Causative organism; Treponema pallidum, a spirochete Affects: Skin, CNS, Eyes, Joints, Skeletal system, Kidneys, Cardiovascular 196 Mode of transmission: Direct contact with exudates from moist, early, obvious or concealed lesions of skin and mucous membranes Semen, Blood, Saliva, Vaginal discharges, Blood transfusions, Needle sticks Congenital transmission 197 S/S: Occurs in 4 stages Primary stage - painless lesion develops at point of entry called a chancre, 1090 days after initial contact. Lesion heals spontaneously within 1-5 weeks Highly communicable at this stage 198 Secondary stage - bacteremia stage begins 2-10 weeks after appearance of primary lesion H/A Malaise Anorexia Fever Sore throat Lymphadenopathy Rash, (small, red, flat lesions) on palms and soles of feet, lasts about 6 weeks. 199 Condyloma latum - painless wart-like lesion found on moist, warm sites like inguinal area. Extremely infectious, lasts @ 6 weeks. Skin infection in areas of hair growth results in bald spots and/or loss of eyebrows. CNS - eyes, bone and joints or kidneys may become involved. 201 Third stage - latent syphilis 1 – 40 years 25% may relapse and develop secondary stage symptoms again. After 4 years, there are generally no more relapses 33% of patients will progress to tertiary syphilis; the rest will remain asymptomatic. 202 Tertiary (Late) Syphilis Granulomatous lesions (gummas) found on skin and bones; skin gummas are painless with sharp borders; bone lesions cause a deep, growing pain. Cardiovascular syphilis; occurs 10 years after primary infection; generally results in dissecting aneurysm of ascending aorta or aortic arch. Antibiotics don’t reverse this disease process. 203 Neurosyphilis; asymptomatic, develop menengitis, Spinal cord disease that results in loss of reflexes and loss of pain and temperature sensation. Tabes dorsalis; spinal column degeneration; wide gait and ataxia Spirochetes attack cerebral blood vessels and cause CVA. Psychosis, Insanity 204 Late Stage Syphilis 205 Syphilis can do a number on your genitalia: Secondary syphilis w/gross disfiguration Patient management: BSI Causative agent extremely fragile and is easily killed by heat, drying, or soap and water. Treatment is effective with penicillin, erythromycin, doxycycline. 207 US Syphilis Rates by State, 2004 2.4 0.4 0.2 0.0 0.8 0.5 1.8 0.5 0.0 0.6 3.8 0.2 1.0 0.4 1.8 0.6 3.8 3.1 1.4 2.8 0.9 0.7 4.4 1.0 2.1 0.2 1.6 1.6 1.1 1.7 2.8 2.0 3.7 0.2 0.4 1.8 2.4 1.3 1.7 1.1 6.9 2.3 2.2 Guam 0.0 6.3 Rate per 100,000 population 3.7 7.4 1.2 VT NH MA RI CT NJ DE MD 1.9 4.3 <=0.2 0.21-4.0 >4.0 0.6 Puerto Rico 4.7 Virgin Is. 4.6 (n= 7) (n= 39) (n= 7) Statistics Oregon: 2005 – 57 cases reported • 2004 – 58 cases reported 115% increase over 2001 209 Gonorrhea AKA “The Clap” Causative agent; Neisseria gonorrheae Affect genital organs and associated structures Mode of transmission: direct contact with exudates of mucous membranes; unprotected sex. 210 S/S - Males: Initial inflammation of urethra with dysuria and purulent urinary discharge . Left untreated, can progress to epididymitis, prostitis, and strictures of urethra. 211 Typical Gonorrheal penile discharge 212 S/S - Females: Dysuria and purulent vaginal discharge may occur. Most females have no pain and minimal urethral discharge. 213 Infection of uterus can progress to PID; fever, lower abdominal pain, abnormal menstrual bleeding, cervical motion tenderness. Menstruation allows bacterial spread from cervix to upper genital tract 50% of PID occurs within 1 week of onset of menstruation. 214 Females at increased risk for sterility, ectopic pregnancy, abscesses of fallopian tubes, ovaries, peritoneum, and peritonitis. 215 Males and females: In rare cases, systemic bacteremia Septic arthritis with fever, pain, swelling of 1 or 2 joints can occur. Patient management: BSI Antibiotics 216 Statistics Oregon: 1980 – 11,162 1995 – 854 2001 – 1,039 2005 – 1,562 217 Gonorrhea Rates by State, 2004 45.8 9.6 16.1 17.4 36.6 58.4 7.5 92.3 39.8 11.8 97.6 172.4 42.4 90.9 65.9 137.3 85.0 67.1 72.8 179.0 162.8 110.6 25.6 69.7 93.3 126.8 49.3 116.0 161.6 67.0 151.8 221.1 Guam 69.7 182.3 181.7 Rate per 100,000 population 110.2 234.4 87.4 13.9 10.3 47.5 75.8 82.2 77.5 109.4 150.6 180.7 145.1 248.6 VT NH MA RI CT NJ DE MD 109.2 <=19.0 19.1-100.0 >100.0 94.9 Puerto Rico 6.9 Virgin Is. 68.9 (n= 8) (n= 25) (n= 20) Chlamydia Causative organism; Chlamydia trachomatis Affects; eyes, genital area and associated organs, respiratory system 219 Mode of transmission sexual activity, sharing contaminated clothing or towels. S/S: similar to gonorrhea Conjunctivitis may occur; leading cause of preventable blindness in the world. Infant pneumonia known to occur. Healthy Cervix Chlamydia Statistics Most common reported STD in Oregon 2005 – 9,018 222 US Chlamydia Rates by State, 2004 287.6 284.2 161.8 285.6 244.1 229.3 203.8 351.2 331.3 215.9 308.0 409.2 236.3 307.5 301.2 298.5 372.9 297.6 164.0 344.4 311.0 300.8 482.0 275.1 295.2 344.3 152.3 292.9 373.7 157.1 288.5 444.2 Guam 457.2 295.8 394.7 Rate per 100,000 population 317.5 485.7 609.4 183.6 134.8 205.8 319.8 274.2 202.0 361.3 362.2 344.5 385.4 654.7 VT NH MA RI CT NJ DE MD 250.0 (n= 2) <=150.0 150.1-300.0 (n= 25) (n= 26) >300.0 422.0 Puerto Rico 92.5 Virgin Is. 278.5 Scabies Scabies; a mite; a parasite Female burrows into epidermis to lay eggs; remains in burrow for 1 month. Affects skin Modes of transmission; skin-skin contact Bedding only if within 24 hours. Mite can burrow into skin in 2.5 minutes. 224 S/S: Intense itching, esp. at night with vesicles, papules, linear burrows. Males; lesions prominent around finger webs, anterior surfaces of wrists and elbows, armpits, belt line, thighs, external genitalia Females; lesions prominent on nipples, abdomen, lower portion of buttocks. Infants; head, neck, palms, soles. 225 Patient management: BSI Personal - launder everything used in last 48 hours in hot water. Treatment with Kwell 226 Lice Infesting agents: Head louse, body louse Responsible for outbreaks of epidemic typhus & trench fever in WWI Modes of transmission: Head lice and body lice - direct contact Body lice - indirect contact, esp. shared clothing Crab lice - sexual contact 227 Head Louse infestation 228 3 stage life cycle; eggs, nymphs, adults Eggs hatch in 7-10 days Nymph stage lasts @ 7-13 days Egg-egg cycle lasts 3 weeks. 229 S/S: Itching Infestation of Head lice is of hair, eyebrows, eyelashes, mustache, beards. Infestation of body lice is of clothing, especially along seams of inner surfaces. 230 Patient management: Personal treatment - Kwell, etc. repeat in 7-10 days. Wash all bedding, clothing, etc. in hot water, or place in dryer on hot cycle. EMS workers - clean patient area well. 231 Lyme Disease Causative organisms; Borrelia burgdorferi Affects skin, CNS, cardiovascular system, joints Mode of transmission; tick borne with reservoirs in mice and deer Western Black-legged Tick 232 Statistics Oregon – 2005 - 24 Cases Tillamook: 5 Hood River: 7 May - August 233 S/S: Early, localized stage with painless skin lesion at site of bite (starts out as red, flat, round rash which spreads out. 234 Border remains bright red, center becomes clear, blue or necrose and black, flu-like syndrome with malaise, myalgia, stiff neck. 235 236 Early disseminated stage; invades skin, nervous system, heart, joints Skin - multiple lesions Nervous system - meningitis, Bell’s palsy, peripheral neuropathy Cardiac; AV block, Myocarditis 237 Joint and muscle pain - can occur 6 months after bite Late stage: ~10% develop chronic arthritis Encephalopathy can develop; cognitive deficits, depression, sleep disorders. 238 Almost time to go…. 239 Body fluids to which universal precautions apply Blood, other body fluids containing blood Semen, vaginal secretions Human tissue Human fluids CSF Synovial Pleural Peritoneal Pericardial Amniotic 240 Body fluids to which universal precautions do not apply In the absence of blood Feces Nasal secretions Sputum Sweat Tears Urine Vomitus 241 Precautions for other body fluids in special settings Human breast milk if mother HIV positive Saliva if person HBV or HIV positive 242 Remember! Prepare food and eat in appropriate areas Maintain general and psychological health Dispose of needles and sharps appropriately Don’t wipe face and/or rub eyes, nose, mouth etc. 243 Bye Bye now... 244