Case Study 1
advertisement

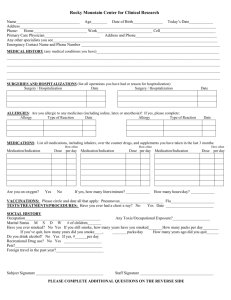
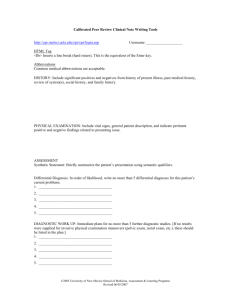
Gill Heart Institute Strive to Revive Case Study 1 Case Objectives • Discuss critical aspects of initial resuscitation that affected outcomes • Discuss important aspects of postresuscitation care: – ECMO – Management of VT CASE DETAILS • CC: unconscious during MVA • HPI: 58 yo female w/ PMHx notable for obesity s/p gastric bypass surgery, DM, HTN, hypothyroidism who presented as a trauma alert after a MVA. Patient reportedly had swerved off the road and slowed to a stop with minimal trauma. Bystanders noted that patient was unconscious, and called EMS. Pre-Hospitalization OSH Course ED Course Early Hospitalization and Workup Rest of Hospitalization • EMS called – found patient to be pulseless. CPR initiated. Primary rhythm was PEA, and was given epinephrine and chest compression – Regained Pulse in the field and was found to be tachycardic • Patient was transferred to OSH PreHospitalization OSH Course ED Course Early Hospitalization and Workup Rest of Hospitalization •CPR initiated •Regained pulse • At OSH, patient was intubated for airway protection and hypoxic respiratory failure • Found to be in Atrial Fibrillation with Rapid ventricular response – Loaded on Amiodarone at OSH • Transferred to UK as a Trauma Alert HISTORY • PMHx: – – – – – HTN Hypothyroidism DM OA Obesity • PSurgHx: – s/p Gastric Bypass Surgery >10 years ago – Hernia repair – Total Knee replacement • FamHx: – No history of SCD or ICD placement. Detailed family history unavailable • SocHx: – Significant EtOH abuse per family that was present. – No known illicit drug use. – Significant social stressors – Recent death of husband and premature birth of grandchildren – • ROS: – Not obtainable HISTORY • Medications: – Levothyroxine 200 mcg daily – Lisinopril 10 mg daily – Metformin 500 mg twice daily – Metoprolol Succinate 25 mg daily • Allergies: No known drug or food allergies PHYSICAL EXAM • Vitals: HR: 169, BP: 97/63, RR: 39, SpO2 of 99% on 100% FiO2 • Gen: Obese, mechanically ventilated, cool to touch • Head: Atraumatic, plethoric and cool • Eyes: Left pupil is 5 mm and right is 3 mm, reactive • Nose: Nares patent, no discharge • Mouth: Endotracheal tube in place • Neck: Trachea midline • Respiratory: Distant breath sounds • CV: Irregularly irregular, tachycardic, 1+ central pulses • Abdomen: Soft nontender distended • Extremities: Cool, absent distal pulses • Neuro: She is intermittently flexing upper extremities with no purposeful movement, no response to pain • Psych: Unable to assess Initial ECG PreHospitalization •CPR initiated •Regained pulse OSH Course ED Course Early Hospitalization and Workup Rest of Hospitalization •Intubated •Started on Amiodarone • Afib with RVR to the 170s • Concern that patient had inadequate perfusion with SBP<100 • DCCV at 200 J x 1 with conversion to sinus rhythm transiently then return to Afib with RVR • Trauma called – no significant trauma noted PreHospitalization •CPR initiated •Regained pulse OSH Course ED Course Early Hospitalization and Workup Rest of Hospitalization •Intubated •Started on Amiodarone • Work-up – CT PE – negative – CT head and spine – no significant acute findings other than rib fractures • Thought to be related to CPR • Cardiology consulted for evaluation PreHospitalization •CPR initiated •Regained pulse OSH Course •Intubated •Started on Amiodarone ED Course Early Hospitalization and Workup Rest of Hospitalization •Given Diltiazem 10 mg x 1 •Followed by DCCV • Patient went emergently to cardiac cath lab given cardiovascular arrest and subsequent arrhythmia – RHC • • • • RA: 26 mmHg PA: 52/24, mean of 38 mmHg PCWP: 30 mmHg PA saturation: 24% – CO , CI: 3.8 L/min , 1.9 L/min/m2 – Selective coronary angiography • Non-obstructive CAD – Left ventriculography • Global Hypokinesis w/ EF<30% – Left Heart catheterization • LVEDP: 30 mmHg PreHospitalization •CPR initiated •Regained pulse OSH Course •Intubated •Started on Amiodarone ED Course Early Hospitalization and Workup Rest of Hospitalization •Given Diltiazem 10 mg x 1 •Followed by DCCV • Given inotropes in the cath lab, with minimal improvement • Placed emergently on VA ECMO • Transferred to the CVICU under the care of the CCU team Telemetry strips in CCU Telemetry strips in CCU PreHospitalization •CPR initiated •Regained pulse OSH Course •Intubated •Started on Amiodarone ED Course Early Hospitalization and Workup Rest of Hospitalization •DCCV • Polymorphic ventricular tachycardia noted soon after arrival to the CCU • Defibrillated X 1 with return of sinus rhythm First ECG after Defibrillation PreHospitalization •CPR initiated •Regained pulse OSH Course •Intubated •Started on Amiodarone ED Course •Given Diltiazem 10 mg x 1 •Followed by DCCV • Initial Labs: – CBC unremarkable – – – – – – – – Early Hospitalization and Workup Na: 138 K: 6.3 Cl: 106 CO2: 11 BUN/Cr: 14/1.14 Mag: 1.3 Ca: 7.9 Phos: 6.1 • ABG: – – – – – – – pH: 7.32 PaCO2: 22 PaO2: 291 Base Deficit: 13 Albumin 2.3 AG: 21 TnI: 0.29 Rest of Hospitalization PreHospitalization •CPR initiated •Regained pulse OSH Course •Intubated •Started on Amiodarone ED Course Rest of Hospitalization •Given Diltiazem 10 mg x 1 •Followed by DCCV • Initial Labs: – CBC unremarkable – – – – – – – – Early Hospitalization and Workup Na: 138 K: 6.3 Cl: 106 CO2: 11 BUN/Cr: 14/1.14 Mag: 1.3 Ca: 7.9 Phos: 6.1 • ABG: – – – – – – – pH: 7.32 PaCO2: 22 PaO2: 291 Base Deficit: 13 Albumin:2.3 AG: 21 TnI: 0.29 Initial assessment • Cardiogenic shock with new global LV dysfunction – Etiology non-ischemic • EtOH vs other non-ischemic etiology • Stunning from either CPR or initial arrest – Afib w/ RVR secondary to this? • AG metabolic acidosis w/ respiratory compensation • Profound hyperkalemia and hypomagnesemia • QT prolongation – Mg and QT prolonging agents Pre-Hospitalization • CPR initiated • Regained pulse OSH Course • Intubated • Started on Amiodarone ED Course • Given Diltiazem 10 mg x1 • Followed by DCCV Early Hospitalization and Workup Rest of Hospitalization • Cardiac catheterization • PA sat: 27% • ECMO • Workup – QT prolonged •Mg of 1.3 • Was initially on dopamine, but went into polymorphic VT – Magnesium aggressively repleted – Amiodarone and other QT prolonging agents had been stopped – Started on isoproterenol to increase basal heart rate and decrease opportunity for myocytes to spontaneously depolarize Pre-Hospitalization • CPR initiated • Regained pulse OSH Course • Intubated • Started on Amiodarone ED Course • Given Diltiazem 10 mg x1 • Followed by DCCV Early Hospitalization and Workup Rest of Hospitalization • Cardiac catheterization • PA sat: 27% • ECMO • Workup – QT prolonged •Mg of 1.3 • Did not require vasopressors • Was cautiously diuresed – Close monitoring of electrolytes • Added afterload reduction as a part of a CHF regimen – Lisinopril – Spironolactone – Metoprolol switched to Carvedilol Pre-Hospitalization • CPR initiated • Regained pulse OSH Course • Intubated • Started on Amiodarone ED Course • Given Diltiazem 10 mg x1 • Followed by DCCV Early Hospitalization and Workup Rest of Hospitalization • Cardiac catheterization • PA sat: 27% • ECMO • Workup – QT prolonged •Mg of 1.3 • Repeat ECG showed QTc of 530. • Had an episode of Afib while on isoproterenol requiring DCCV • No more VT after improvement in QTc and correction of Mg • Weaned off ECMO with stable HD • Extubated and transferred to the floor • Neurologically intact Pre-Hospitalization • CPR initiated • Regained pulse OSH Course • Intubated • Started on Amiodarone ED Course • Given Diltiazem 10 mg x1 • Followed by DCCV Early Hospitalization and Workup Rest of Hospitalization • Cardiac catheterization • PA sat: 27% • ECMO • Workup – QT prolonged •Mg of 1.3 • Final Assessment: – Cardiogenic shock 2/2 non-ischemic CM – resolved – LV dysfunction – not resolved – Polymorphic VT – resolved – Prolonged QTc – improved, but not resolved – Respiratory failure after arrest – resolved Summary of Hospital Course • Timeline PreHospitalization • CPR initiated • Regained pulse OSH Course • Intubated • Started on Amiodarone ED Course • Given Diltiazem 10 mg x 1 • Followed by DCCV Early Hospitalization and Workup • Cardiac catheterization • PA sat: 27% • ECMO • Workup – QT prolonged • Mg of 1.3 Rest of Hospitalization • Polymorphic VT • Stopped QT prolonging agents • Corrected Mg • Isoproterenol • Extubated • Neurologically intact Resuscitative Measures • CPR delayed until EMS arrived – Fortunately, no evidence of anoxic brain injury • Role of ECMO – Needs clearly defined end point – In this case, to allow time and interventions for resolution of cardiogenic shock and VT • Management of VT – Reversible causes – Important to understand etiology of VT DM • Questions