How to deal with suspected
arrhythmia
CCG Educational Evening 17.7.14
Dr Sanjay Kumar
Lead Consultant Cardiologist
Dr Ravi Kamdar
Consultant Cardiologist in Devices and Arrhythmia
Croydon Health Services NHS Trust
© your company name. All rights
reserved.
Objectives
• Brief overview of new suspected arrhythmia
pathway
• Things to do before referral
• Case studies
• Questions
Suspected Arrhythmia –
diagnosis & management
Immediate transfer to
hospital for specialist
assessment/treatment
treatment
* In all adult age groups , use
traffic lights system to guide
further action ( slides 2 & 3)
Patient presents with symptoms, palpitations, chest pain,
dyspnoea, syncope/pre syncope, asymptomatic
Red Flag signs:
• Patient looks unwell e.g. signs of heart
failure
• Exercise – induced dizziness/syncope
• Syncope with injury
• Syncope with angina
• Syncope with known
structural/ischaemic heart disease
• 2nd or 3rd Degree Heart Block
• Other ECG abnormality – evidence of
previous MI,LV hypertrophy ,short PR
interval, long QT,LBBB, significant twave inversion
Assessment – history & examination. Onset of symptoms
(duration) – palpitations, dyspnoea, and impact of activities of
daily living or at night. Past medical history & family history.
Examination: General appearance, respiratory rate, pulse, BP,
chest auscultation. Full blood count, urea & electrolytes,
glucose, TFTs & LFTs and chest X ray if appropriate
Red flag signs
Steps that are based in primary care
Steps that are based in acute
Steps that are taken in community services
Decision making point
Shared decision making with patient
12 lead ECG with
accurate interpretation
and reporting. Consider
echocardiogram
Review of results to determine if single episode. Normal ECG and
no evidence of structural heart disease. Consider other diagnosis
and further investigation if appropriate. Management in primary
care. Consider virtual Cardiac advise Service
Normal results – changes required e.g. reduce caffeine intake
Abnormal results with recurrent symptoms
Incidental finding of
Atrial fibrillation e.g.
pulse check
Atrial fibrillation
Complete CHADS₂ - Vasc
risk score
Referral to Community Arrhythmia clinic if :
• Age <65yrs
• Adequate heart rate or rhythm control not achieved
• Symptomatic despite good rate/rhythm control
• Paroxysmal AF
• AF with other ECG abnormality, structural heart disease or
heart failure
• Lone AF e.g. no history or echo evidence of cardiovascular
disease
Initiate Anticoagulant therapy if appropriate with Primary care
management with annual review to monitor rate and rhythm in line
with Croydon guidelines.
http://nhscroydonintranet.croydonpct.nhs.uk/TeamsAndDepartmen
ts/primarycarecommissioning/prescribing/Pages/Documents.aspx
Recurrent palpitations, recurrent presyncope/syncope/symptomatic bradycardia
See slide 4
Family history of
inherited cardiac
condition
Community Arrhythmia clinic – Consultant –led
with Arrhythmia Nurse Specialist
Discharge to primary care
as appropriate
LIFESTYLE
Inherited Cardiac Condition
Clinic
Community Anti Coagulant Clinic
Impact of exercise and
advise regarding
management to maintain
an active lifestyle without
fear
Smoking cessation
course
Alcohol advice and guidance
on healthy eating
Work – driving or flying
issues. Sensitive issues
regarding sexual activity
Palpitations - What to do before referral (1)
Identify specific patients….high risk of adverse outcomes? Can intervention improve QoL?
What does the patient mean?
‘Abnormally perceived heartbeat’ – tachycardia, bradycardia, irregularity, pounding, ‘missed beats’, ‘extra beats’, ‘fluttering’
Do they mean chest discomfort?
Duration, frequency, Onset/offset, Precipitating factors – nocturnal? exertional? Emotional? Mode of termination – vagal?
What else happens? Pre-syncope or syncope, acute-onset sustained SOB, chest pain
What’s making it worse?
Mental health – anxiety, depression, somatisation disorders
Caffeine, alcohol
Recreational drugs – amphetamines, cocaine
Medications – β agonist, theophylline, T4, calcium antagonists, class I anti-arrhythmics (e.g. flecainide), drugs prolonging QTc
Family history?
Evidence of early-onset AF, heart failure or premature CAD in close relative?
Sudden cardiac or unexplained death <40yrs old? RTA? Drowning?
Potential misdiagnosis of epilepsy? Sudden death?
Palpitations - What to do before referral (2)
Examination & simple tests
Physical evidence of structural heart disease (HF, abnormal HS, murmurs)?
Thyrotoxicosis? Anaemia?
12 lead ECG – AF, high-grade heart block, old MI, LVH, LBBB, ischaemic ST/t-wave change, short PR, long QTc
Sources of advice for patients
CUH arrhythmia nurse / clinic
Charities: Arrhythmia Alliance: www.heartrhythmcharity.org.uk
Atrial Fibrillation Association: www.atrialfibrillation.org.uk
Sudden Adult Death Trust: www.sadsuk.org
Cardiac Risk in the Young: www.c-r-y.org.uk
Occupation / driving: DVLA rules
If arrhythmia identified that causes (or is likely to cause) incapacity, stop driving
Doctors’ responsibility to inform patient
If no diagnosis (or awaiting specialist assessment), but disabling symptoms, advise patient to stop driving
Working at height?
Control of potentially dangerous machinery?
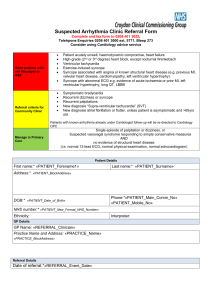
Suspected Arrhythmia Community Clinic Referral Form
Please complete form and fax to Clinic administrator on 020 8401 3022
Enquiries: Arrhythmia nurse specialist: 020 8401 3000, ext. 5771 or bleep 273
Cardiology GP Advice Service:
email mhn-tr.gpcardiologyadviceservice@nhs.net; http://www.croydonhealth.nhs.uk/GPadviceservice
Referrals without an ECG and incomplete forms will be returned
Refer patients with “red flag” signs to A&E:
·
·
·
·
·
·
Patient acutely unwell, haemodynamic compromise, heart failure
nd
rd
High-grade (2 or 3 degree) heart block, except nocturnal Wenkebach
Ventricular tachycardia
Exercise-induced syncope
Syncope associated with angina or known structural heart disease (e.g. previous MI, valvular
heart disease, cardiomyopathy, left ventricular hypertrophy)
Syncope with abnormal ECG e.g. evidence of acute ischaemia or prior MI, left ventricular
hypertrophy, long QT, LBBB
Referral criteria for Community Clinic (no “red flag” signs):
·
·
·
·
·
Symptomatic bradycardia
Recurrent dizziness or syncope
Recurrent palpitations
New diagnosis “Supra-ventricular tachycardia” (SVT)
New diagnosis atrial fibrillation or flutter, unless patient is asymptomatic and >65yrs old
Patients with known arrhythmia already under Cardiologist follow-up will be redirected to Cardiology OPC.
Manage in Primary Care (web link to traffic lights):
Single episode of palpitation or dizziness, or
Suspected vasovagal syndrome responding to simple conservative measures
AND
no evidence of structural heart disease
(i.e. normal 12-lead ECG, normal physical examination, normal echocardiogram)
Patient'details' !
!
'
Name! !
!
!
Sex!
d.o.b.! !
!
!
NHS!Number!
!
!
Hosp.!Number!
Address!
!
!
!
!
Telephone!
!
!
Ethnicity!!
Interpreter!needed?!!Y!/!N!
!
!
!
GP'details'
!
!
!
GP!name!
!
!
!
!
!
!
Practice!name!
Practice!address!
!
!
!
!
!
!
Postcode!
Telephone!!
!
Syncope?
!
Other:!
Clinical'history! !
Palpitations?
! !
!
Frequency:!
!
Shortness!of!breath?!! !!!!!!
Dizziness?
!!!
!
Asymptomatic!(incidental!finding)?! !
!
!
!
!
!
!
Fatigue?
!
!
Page 1/2
Reason'for'referral'
''
Syncope'/'dizziness'
'
'
AF/flutter''
Palpitations'''
Other'
'
Clinical'examination'&'investigation'(fax'all'results'B'*'denotes'data'without'which'referral'will'be'rejected):'
Medications'
·
·
Initial'primary'care'management'
·
·
Where'would'your'patient'prefer'to'be'seen?'
To be completed by clinic staff
Date referral received:
ECG included? Y/N
Provisional appointment date:
Tests required before clinic appointment:
If inappropriate referral, referrer informed? Y/N
How would you manage these patients?
Case Study 1
64yr old lady
Irregular pulse on recent pulse check
12-lead ECG: Atrial fibrillation, heart rate 120bpm, otherwise NAD
Many years’ minor (NYHA class 2) exertional breathlessness, otherwise no symptoms
Hypertension, type 2 diabetes, 30U alcohol/week
o/e Looks well, BP 150/90, RR 12, no cardiac murmurs
FBC, U&E, TFT normal
CXR – no parenchymal lung abnormality, borderline cardiomegaly
Action
Advice?
Reduce alcohol intake. Avoid vigorous effort until rate-controlled. Treat co-morbidity e.g. salt/BP
Drugs?
Rate control with β blocker (exercise-induced tachycardia) or rate-limiting CCB (BP); anti-coagulate with warfarin
Investigation?
Echo (LV function, LA size, valves, evidence of CAD); 24hr Holter after initiating rate-limiters (HR control)
Onward referral?
Suspected arrhythmia clinic – <65, rate or rhythm control? Diagnose underlying cause?
The CHADS2 index has been routinely used as an initial, rapid,
and easy-to-remember means of assessing stroke risk1–4
CHADS2 criteria
Congestive HF
CHADS2
Adjusted stroke rate*
(95% CI)
6
18.2
(10.5 to 27.4)
5
12.5
(8.2 to 17.5)
4
8.5
(6.3 to 11.1)
3
5.9
(4.6 to 7.3)
Score
1
Patients (%)
36.1%
Hypertension
1
Age ≥75 years
1
Diabetes
1
2
4.0
(3.1 to 5.1)
30.1%
Stroke or TIA
(previous history)
2
1
2.8
(2.0 to 3.8)
27%
0
1.9
(1.2 to 3.0)
6.9%
Sum
*Adjusted stroke rate = expected stroke rate per 100 patient-years
from exponential survival model, assuming ASA not taken
1. Gage et al. JAMA 2001;285:2864–2870
2. Gage et al. Circulation 2004;110:2287–2292
3. Camm et al. Eur Heart J 2010;31:2369–2429
4. Nieuwlaat et al. Eur Heart J 2006;27:3018–3026
33.6% with
CHADS2
0 or 1
The CHA2DS2-VASc scheme was adopted by the ESC
to complement the CHADS2 scoring system
CHADS2
Score
CHA2DS2-VASc
Score
Congestive
heart failure
1
Congestive heart failure/left ventricular dysfunction
1
Hypertension
1
Hypertension
1
Aged ≥75 years
1
Aged ≥75 years
2
Diabetes mellitus
1
Diabetes mellitus
1
Stroke/TIA/TE
2
Stroke/TIA/TE
2
Maximum score
6
Vascular disease (prior MI, PAD, or aortic plaque)
1
Aged 65–74 years
1
Sex category (i.e. female gender)
1
Maximum score
9
CHA2DS2-VASc:
In patients with a CHADS2 score of 0–1, or
When a more detailed stroke risk assessment is indicated
Camm et al. Eur Heart J 2010;31:2369–429.
The 2010/2012 ESC guidelines recommend use
of a simple bleeding risk score: HAS-BLED
Letter
Clinical characteristic
Points awarded
H
Hypertension
1
A
Abnormal renal and liver function
(1 point each)
S
Stroke
1
B
Bleeding
1
L
Labile INRs
1
E
Elderly (e.g. age >65 years)
1
D
Drugs or alcohol (1 point each)
1 or 2
1 or 2
Maximum 9 points
HAS-BLED ≥3:
Indicates ”high risk”, and
Some caution and regular review of the patient is needed following
the initiation of antithrombotic therapy, whether with OAC or aspirin
Camm et al. Eur Heart J 2010;31:2369–429.
Camm et al. Eur Heart J 2012;e-published August 2012, doi:10.1093/eurheartj/ehs253.
Pisters et al. Chest 2010;138:1093–100.
How would you manage these patients?
Case Study 2
27yr old female medico-legal solicitor
c/o 1 episode of severe dizziness while standing in a long post-office queue, nearly lost consciousness
No chest pain, SOB
No recurrent symptoms
PMH: 2 previous similar episodes aged 16 and 18, while studying for exams
No medication, no alcohol, occasional cannabis use
FH: mother died suddenly aged 35, cause unknown
o/e normal – no cardiac murmurs
FBC, U&E, TFT normal
12-lead ECG: sinus rhythm 70bpm, no heart block, normal QTc
Action
Advice? Identify & avoid triggers e.g. prolonged standing, pain/cough/laugh, review/minimise work stresses; keep
well-hydrated; curtail cannabis use
Drugs? Water
Investigation? Echocardiogram (subclinical cardiomyopathy, severe valvular heart disease)
Onward referral? One-stop arrhythmia clinic, GP advice service
What if no FHx? Re-assure likely vasovagal – advice, referral only if symptoms not controlled by conservative means
How would you manage these patients?
Case Study 3
79yr old man
c/o 4 episodes of self-terminating palpitation, over a period of 6 weeks
Each episode approximately 1-minute long, associated with minor SOB
Minor (NYHA class 2) exertional SOB, no angina pectoris, no syncope
MI 10 years ago, hypertension, hypercholesterolaemia, current smoker
Rx: Aspirin, lisinopril, simvastatin (beta blocker not tolerated – dizziness)
o/e normal – no cardiac murmurs
FBC, U&E, TFT normal
12-lead ECG: sinus rhythm 60bpm, first degree heart block, LBBB
Similar ECG appearances 3 years ago
Action
Advice? Stop smoking (IHD)
Drugs? Avoid rate-limiting medication
Investigation? CXR (HF), echo (LVSD, LVH, scar, substrate for AF/VT)
Onward referral? A&E (red flag)