Blood Flow
advertisement

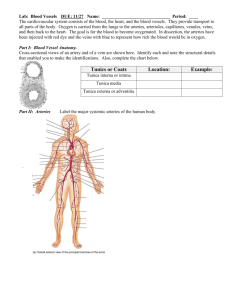
Lab Lecture #3 Circulatory system 1/20/10 Monitoring Circulatory Efficiency • Vital signs: pulse and blood pressure, along with respiratory rate and body temperature • Pulse: pressure wave caused by the expansion and recoil of arteries • Radial pulse (taken at the wrist) routinely used Measuring Blood Pressure • Systemic arterial BP • Measured indirectly by the auscultatory method using a sphygmomanometer • Pressure is increased in the cuff until it exceeds systolic pressure in the brachial artery Measuring Blood Pressure • Pressure is released slowly and the examiner listens for sounds of Korotkoff with a stethoscope • Sounds first occur as blood starts to spurt through the artery (systolic pressure, normally 110–140 mm Hg) • Sounds disappear when the artery is no longer constricted and blood is flowing freely (diastolic pressure, normally 70–80 mm Hg) Variations in Blood Pressure • Blood pressure cycles over a 24-hour period • BP peaks in the morning due to levels of hormones • Age, sex, weight, race, mood, and posture may vary BP Alterations in Blood Pressure • Hypotension: low blood pressure • Systolic pressure below 100 mm Hg • Often associated with long life and lack of cardiovascular illness Homeostatic Imbalance: Hypotension • Orthostatic hypotension: temporary low BP and dizziness when suddenly rising from a sitting or reclining position • Chronic hypotension: hint of poor nutrition and warning sign for Addison’s disease or hypothyroidism • Acute hypotension: important sign of circulatory shock Alterations in Blood Pressure • Hypertension: high blood pressure • Sustained elevated arterial pressure of 140/90 or higher • May be transient adaptations during fever, physical exertion, and emotional upset • Often persistent in obese people Homeostatic Imbalance: Hypertension • Prolonged hypertension is a major cause of heart failure, vascular disease, renal failure, and stroke • Primary or essential hypertension • 90% of hypertensive conditions • Due to several risk factors including heredity, diet, obesity, age, stress, diabetes mellitus, and smoking Homeostatic Imbalance: Hypertension • Secondary hypertension is less common • Due to identifiable disorders, including kidney disease, arteriosclerosis, and endocrine disorders such as hyperthyroidism and Cushing’s syndrome Blood Flow Through Body Tissues • Blood flow (tissue perfusion) is involved in • Delivery of O2 and nutrients to, and removal of wastes from, tissue cells • Gas exchange (lungs) • Absorption of nutrients (digestive tract) • Urine formation (kidneys) • Rate of flow is precisely the right amount to provide for proper function Brain Heart Skeletal muscles Skin Kidney Abdomen Other Total blood flow at rest 5800 ml/min Total blood flow during strenuous exercise 17,500 ml/min Figure 19.13 Velocity of Blood Flow • Changes as it travels through the systemic circulation • Is inversely related to the total cross-sectional area • Is fastest in the aorta, slowest in the capillaries, increases again in veins • Slow capillary flow allows adequate time for exchange between blood and tissues Relative crosssectional area of different vessels of the vascular bed Total area (cm2) of the vascular bed Velocity of blood flow (cm/s) Figure 19.14 Autoregulation • Automatic adjustment of blood flow to each tissue in proportion to its requirements at any given point in time • Is controlled intrinsically by modifying the diameter of local arterioles feeding the capillaries • Is independent of MAP, which is controlled as needed to maintain constant pressure Autoregulation • Two types of autoregulation 1. Metabolic 2. Myogenic Metabolic Controls • Vasodilation of arterioles and relaxation of precapillary sphincters occur in response to • Declining tissue O2 • Substances from metabolically active tissues (H+, K+, adenosine, and prostaglandins) and inflammatory chemicals Metabolic Controls • Effects • Relaxation of vascular smooth muscle • Release of NO from vascular endothelial cells • NO is the major factor causing vasodilation • Vasoconstriction is due to sympathetic stimulation and endothelins Myogenic Controls • Myogenic responses of vascular smooth muscle keep tissue perfusion constant despite most fluctuations in systemic pressure • Passive stretch (increased intravascular pressure) promotes increased tone and vasoconstriction • Reduced stretch promotes vasodilation and increases blood flow to the tissue Intrinsic mechanisms (autoregulation) • Distribute blood flow to individual organs and tissues as needed Extrinsic mechanisms • Maintain mean arterial pressure (MAP) • Redistribute blood during exercise and thermoregulation Amounts of: Sympathetic pH O2 Metabolic a Receptors b Receptors controls Amounts of: Nerves Epinephrine, norepinephrine CO2 K+ Angiotensin II Hormones Prostaglandins Adenosine Nitric oxide Endothelins Myogenic controls Stretch Antidiuretic hormone (ADH) Atrial natriuretic peptide (ANP) Dilates Constricts Figure 19.15 Long-Term Autoregulation • Angiogenesis • Occurs when short-term autoregulation cannot meet tissue nutrient requirements • The number of vessels to a region increases and existing vessels enlarge • Common in the heart when a coronary vessel is occluded, or throughout the body in people in high-altitude areas Blood Flow: Skeletal Muscles • At rest, myogenic and general neural mechanisms predominate • During muscle activity • Blood flow increases in direct proportion to the metabolic activity (active or exercise hyperemia) • Local controls override sympathetic vasoconstriction • Muscle blood flow can increase 10 or more during physical activity Blood Flow: Brain • Blood flow to the brain is constant, as neurons are intolerant of ischemia • Metabolic controls • Declines in pH, and increased carbon dioxide cause marked vasodilation • Myogenic controls • Decreases in MAP cause cerebral vessels to dilate • Increases in MAP cause cerebral vessels to constrict Blood Flow: Brain • The brain is vulnerable under extreme systemic pressure changes • MAP below 60 mm Hg can cause syncope (fainting) • MAP above 160 can result in cerebral edema Blood Flow: Skin • Blood flow through the skin • Supplies nutrients to cells (autoregulation in response to O2 need) • Helps maintain body temperature (neurally controlled) • Provides a blood reservoir (neurally controlled) Arteriole Venule Interstitial fluid Net HP—Net OP (35—0)—(26—1) Net HP 35 mm Capillary Net OP 25 mm NFP (net filtration pressure) is 10 mm Hg; fluid moves out Net HP—Net OP (17—0)—(26—1) Net HP 17 mm Net OP 25 mm NFP is ~8 mm Hg; fluid moves in HP = hydrostatic pressure • Due to fluid pressing against a wall • “Pushes” • In capillary (HPc) • Pushes fluid out of capillary • 35 mm Hg at arterial end and 17 mm Hg at venous end of capillary in this example • In interstitial fluid (HPif) • Pushes fluid into capillary • 0 mm Hg in this example OP = osmotic pressure • Due to presence of nondiffusible solutes (e.g., plasma proteins) • “Sucks” • In capillary (OPc) • Pulls fluid into capillary • 26 mm Hg in this example • In interstitial fluid (OPif) • Pulls fluid out of capillary • 1 mm Hg in this example Figure 19.17 Circulatory Shock • Hypovolemic shock: results from large-scale blood loss • Vascular shock: results from extreme vasodilation and decreased peripheral resistance • Cardiogenic shock results when an inefficient heart cannot sustain adequate circulation Acute bleeding (or other events that cause blood volume loss) leads to: 1. Inadequate tissue perfusion resulting in O2 and nutrients to cells 2. Anaerobic metabolism by cells, so lactic acid accumulates 3. Movement of interstitial fluid into blood, so tissues dehydrate Chemoreceptors activated (by in blood pH) Major effect Baroreceptor firing reduced (by blood volume and pressure) Initial stimulus Physiological response Signs and symptoms Result Hypothalamus activated (by pH and blood pressure) Brain Minor effect Activation of respiratory centers Cardioacceleratory and vasomotor centers activated Heart rate Sympathetic nervous system activated Neurons depressed by pH ADH released Intense vasoconstriction (only heart and brain spared) Central nervous system depressed Kidney Renal blood flow Adrenal cortex Renin released Angiotensin II produced in blood Aldosterone released Rate and depth of breathing CO2 blown off; blood pH rises Tachycardia, weak, thready pulse Skin becomes cold, clammy, and cyanotic Kidneys retain salt and water Water retention Urine output Thirst Restlessness (early sign) Coma (late sign) Blood pressure maintained; if fluid volume continues to decrease, BP ultimately drops. BP is a late sign. Figure 19.18 R. external carotid artery R. axillary R. internal carotid artery R. vertebral R. common carotid – right side of head and neck R. subclavian – neck and R. upper limb Brachiocephalic – head, neck, and R. upper limb Arteries of R. upper limb L. external carotid artery L. internal carotid artery L. common carotid – left side of head and neck L. vertebral L. subclavian – neck and L. upper limb Aortic arch L. axillary Arteries of L. upper limb Ascending aorta – L. ventricle to sternal angle Thoracic aorta T5 – T12 (diaphragm) L. and R. coronary arteries L. ventricle of heart Parietal branches Visceral branches Mediastinal – posterior mediastinum Esophageal – esophagus Bronchial – lungs and bronchi Pericardial – pericardium Posterior intercostals – intercostal muscles, spinal cord, vertebrae, pleurae, skin Superior phrenics – posterior and superior diaphragm Diaphragm Abdominal aorta T12 (diaphragm) – L4 Parietal branches Visceral branches Gonadal – testes or ovaries Suprarenal – adrenal glands and Renal – kidneys Superior and inferior mesenterics – small intestine – colon Celiac trunk – liver – gallbladder – spleen – stomach – esophagus – duodenum R. common iliac – pelvis and R. lower limb Arteries of R. lower limb Inferior phrenics – inferior diaphragm Lumbars – posterior abdominal wall Median sacral – sacrum – coccyx L. common iliac – pelvis and L. lower limb (a) Schematic flowchart Arteries of L. lower limb Figure 19.21a Arteries of the head and trunk Internal carotid artery External carotid artery Common carotid arteries Vertebral artery Subclavian artery Brachiocephalic trunk Aortic arch Ascending aorta Coronary artery Thoracic aorta (above diaphragm) Celiac trunk Abdominal aorta Superior mesenteric artery Renal artery Gonadal artery Common iliac artery Inferior mesenteric artery Internal iliac artery (b) Illustration, anterior view Arteries that supply the upper limb Subclavian artery Axillary artery Brachial artery Radial artery Ulnar artery Deep palmar arch Superficial palmar arch Digital arteries Arteries that supply the lower limb External iliac artery Femoral artery Popliteal artery Anterior tibial artery Posterior tibial artery Arcuate artery Figure 19.21b Ophthalmic artery Basilar artery Vertebral artery Internal carotid artery External carotid artery Common carotid artery Thyrocervical trunk Costocervical trunk Subclavian artery Axillary artery Branches of the external carotid artery • Superficial temporal artery • Maxillary artery • Occipital artery • Facial artery • Lingual artery • Superior thyroid artery Larynx Thyroid gland (overlying trachea) Clavicle (cut) Brachiocephalic trunk Internal thoracic artery (b) Arteries of the head and neck, right aspect Figure 19.22b Anterior Frontal lobe Optic chiasma Cerebral arterial circle (circle of Willis) • Anterior communicating artery • Anterior cerebral artery • Posterior communicating artery • Posterior cerebral artery Basilar artery Middle cerebral artery Internal carotid artery Mammillary body Temporal lobe Pons Occipital lobe Vertebral artery Cerebellum Posterior (d) Major arteries serving the brain (inferior view, right side of cerebellum and part of right temporal lobe removed) Figure 19.22d Vertebral artery Thyrocervical trunk Suprascapular artery Costocervical trunk Thoracoacromial artery Axillary artery Posterior circumflex humeral artery Anterior circumflex humeral artery Subscapular artery Brachial artery Deep artery of arm Common interosseous artery Common carotid arteries Left subclavian artery Right subclavian artery Brachiocephalic trunk Posterior intercostal arteries Anterior intercostal artery Internal thoracic artery Descending aorta Lateral thoracic artery Radial artery Ulnar artery Deep palmar arch Superficial palmar arch Digital arteries (b) Illustration, anterior view Figure 19.23b Liver (cut) Inferior vena cava Diaphragm Esophagus Celiac trunk Common hepatic artery Hepatic artery proper Gastroduodenal artery Right gastric artery Gallbladder Left gastric artery Stomach Splenic artery Pancreas (major portion lies posterior to stomach) Right gastroepiploic artery Superior mesenteric mesenteric Duodenum Abdominal aorta Left gastroepiploic artery Spleen (b) The celiac trunk and its major branches. The left half of the liver has been removed. Figure 19.24b Hiatus (opening) for inferior vena cava Hiatus (opening) for esophagus Adrenal (suprarenal) gland Kidney Celiac trunk Abdominal aorta Lumbar arteries Ureter Median sacral artery Diaphragm Inferior phrenic artery Middle suprarenal artery Renal artery Superior mesenteric artery Gonadal (testicular or ovarian) artery Inferior mesenteric artery Common iliac artery (c) Major branches of the abdominal aorta. Figure 19.24c Popliteal artery Anterior tibial artery Posterior tibial artery Lateral plantar artery Medial plantar artery Fibular artery Dorsalis pedis artery (from top of foot) Plantar arch (c) Posterior view Figure 19.25c Common iliac artery Internal iliac artery Superior gluteal artery External iliac artery Deep artery of thigh Lateral circumflex femoral artery Medial circumflex femoral artery Obturator artery Femoral artery Adductor hiatus Popliteal artery Anterior tibial artery Posterior tibial artery Fibular artery Dorsalis pedis artery Arcuate artery Dorsal metatarsal arteries (b) Anterior view Figure 19.25b Veins of the head and trunk Dural venous sinuses External jugular vein Vertebral vein Internal jugular vein Right and left brachiocephalic veins Superior vena cava Great cardiac vein Hepatic veins Splenic vein Hepatic portal vein Renal vein Veins that drain the upper limb Subclavian vein Axillary vein Cephalic vein Brachial vein Basilic vein Median cubital vein Ulnar vein Radial vein Digital veins Veins that drain the lower limb Superior mesenteric vein Inferior vena cava Inferior mesenteric vein External iliac vein Common iliac vein Popliteal vein Internal iliac vein Posterior tibial vein Femoral vein Great saphenous vein Anterior tibial vein (b) Illustration, anterior view. The vessels of the pulmonary circulation are not shown. Small saphenous vein Dorsal venous arch Dorsal metatarsal veins Figure 19.26b Brachiocephalic veins Right subclavian vein Axillary vein Brachial vein Cephalic vein Basilic vein Median cubital vein Internal jugular vein External jugular vein Left subclavian vein Superior vena cava Azygos vein Accessory hemiazygos vein Hemiazygos vein Posterior intercostals Inferior vena cava Ascending lumbar vein Median antebrachial vein Cephalic vein Basilic vein Radial vein Ulnar vein Deep palmar venous arch Superficial palmar venous arch Digital veins (b) Anterior view Figure 19.28b Hepatic veins Inferior vena cava Right suprarenal vein Right gonadal vein Inferior phrenic vein Left suprarenal vein Renal veins Left ascending lumbar vein Lumbar veins Left gonadal vein Common iliac vein Internal iliac vein External iliac vein (b) Tributaries of the inferior vena cava. Venous drainage of abdominal organs not drained by the hepatic portal vein. Figure 19.29b Inferior vena cava (not part of hepatic portal system) Hepatic veins Liver Hepatic portal vein Small intestine Gastric veins Spleen Inferior vena cava Splenic vein Right gastroepiploic vein Inferior mesenteric vein Superior mesenteric vein Large intestine Rectum (c) The hepatic portal circulation. Figure 19.29c Common iliac vein Internal iliac vein External iliac vein Inguinal ligament Femoral vein Great saphenous vein (superficial) Popliteal vein Small saphenous vein Fibular vein Anterior tibial vein Dorsalis pedis vein Dorsal venous arch Dorsal metatarsal veins (b) Anterior view Figure 19.30b Superficial temporal vein Occipital vein Posterior auricular vein External jugular vein Ophthalmic vein Facial vein Vertebral vein Internal jugular vein Superior and middle thyroid veins Brachiocephalic vein Subclavian vein Superior vena cava (b) Veins of the head and neck, right superficial aspect Figure 19.27b Superior sagittal sinus Falx cerebri Inferior sagittal sinus Cavernous sinus Straight sinus Confluence of sinuses Transverse sinuses Sigmoid sinus Jugular foramen Right internal jugular vein (c) Dural venous sinuses of the brain Figure 19.27c