Venous Disease
advertisement

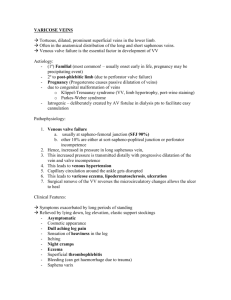
Venous Disease ANATOMY A clear understanding of the anatomy of the venous system in the legs is essential to understanding pathophysiology as well as treatment. Venous drainage of the legs is the function of two parallel and connected systems: the deep and the superficial systems connected by perforators . Superficial Venous System . The dorsal venous arch, into which empty the dorsal metatarsal veins, is continuous with the greater saphenous vein medially and the lesser saphenous vein laterally . The greater saphenous vein, in close proximity to the saphenous nerve, ascends anterior to the medial malleolus, crosses, and then ascends medial to the knee. It ascends in the superficial compartment and empties into the common femoral vein after entering the fossa ovalis. Before its entry into the common femoral vein, it receives medial and lateral accessory saphenous veins, as well as small tributaries from the inguinal region, pudendal region, and anterior abdominal wall. The posterior arch vein drains the area around the medial malleolus, and as it ascends up the posterior medial aspect of the calf, it receives medial perforating veins, termed Cockett’s perforators, before joining the greater saphenous vein at or below the knee. The lesser saphenous vein arises from the dorsal venous arch at the lateral aspect of the foot and ascends posterior to the lateral malleolus, and it empties into the popliteal vein after penetrating the fascia. The exact entry of the lesser saphenous vein into the popliteal vein is variable. Deep Venous System The plantar digital veins in the foot empty into a network of metatarsal veins that comprise the deep plantar venous arch. This continues into the medialand lateral plantar veins that then drain into the posterior tibial veins. The dorsalis pedis veins on the dorsum of the foot form the paired anterior tibial veins at the ankle.The paired posterior tibial veins, adjacent to and flanking the posterior tibial artery, run under the fascia of the deep posterior compartment. These veins enter the soleus and join the popliteal vein, after joining with the paired peroneal and anterior tibial veins. There are large venous sinuses within the soleus muscle—the soleal sinuses—that empty into the posterior tibial and peroneal veins. The popliteal vein enters a window in the adductor magnus, at which point it is termed the femoral vein. The femoral vein ascends and receives venous drainage from the profunda femoris vein, or the deep femoral vein, and after this confluence, it is called the common femoral vein. As the common femoral vein crosses the inguinal ligament, it is called the external iliac vein. Perforating veins Perforating veins connect the superficial venous system to the deep venous system at various points in the leg—the foot, the medial and lateral calf, the mid- and distal thigh . Venous Function The venules, the smallest veins ranging from 0.1 to 1 mm, contain mostly smooth muscle cells, whereas the larger extremity veins contain relatively few smooth muscle cells. These larger caliber veins have limited contractile capacity. The venous valves prevent retrograde flow, and it is the failure of the valves that leads to reflux and associated symptoms. Venous valves are most prevalent in the distal lower extremity, whereas as one proceeds proximally, the number of valves decreases to the point that in the superior and inferior vena cava, no valves are present. The return of the blood to the heart from the lower extremity is facilitated by the muscle pump function of the calf—a mechanism whereby the calf muscle, functioning as a bellows during exercise, compresses the gastrocnemius and soleal sinuses and propels the blood toward the heart. The normally functioning valves in the venous system prevent retrograde flow; it is when one or more of these valves become incompetent that symptoms of venous insufficiency can develop. During calf muscle contraction, the venous pressure of the foot and ankle drop dramatically. The pressures developing in the muscle compartments during exercise range from 150 to 200 mm Hg, and when there is failure of perforating veins, these high pressures are transmitted to the superficial system. Varicose Veins terms The term varicose veins is, in the common parlance, a term that encompasses a spectrum of venous dilation that ranges from minor telangiectasia to severe dilated, tortuous varicose veins. As stated earlier, for a proper categorization, as well as for appropriate treatment options to be considered, certain definitions must be agreed on. Varicose veins refer to any dilated, tortuous, elongated vein of any caliber. Telangiectasias are intradermal varicosities that are small and tend to be cosmetically unappealing but not symptomatic in and of themselves. Reticular veins are subcutaneous dilated veins that enter the tributaries of the main axial or trunk veins. Trunk veins are the named veins, such as the greater or lesser saphenous veins or their tributaries. The end result of CVI can range from aching, heaviness, pain, and swelling with prolonged standing or sitting in the case of symptomatic varicose veins, to severe lipodermatosclerosis with edema and ulceration in the patient with severe CVI. Risk Factors A combination of risk factors, rather than any one specific risk factor, is a better predictor of the likelihood of a given patient developing symptomatic varicose veins. Heredity undoubtedly plays a significant role in the development of varicose veins. Valvular dysfunction and insufficiency Female sex, gravitation hydrostatic force, and hydrodynamic forces due to muscular contraction. Hormonal Influence Venous function is undoubtedly influenced by hormonal changes. In particular, progesterone liberated by the corpus luteum stabilizes the uterus bycausing relaxation of smooth muscle fibers. This effect directly influences venous function. The result is passive venous dilation, which, in many instances, causes valvular dysfunction. Although progesterone is implicated in the first appearance of varicosities in pregnancy, estrogen also has profound effects. It produces the relaxation of smooth muscle and a softening of collagen fibers. Further, the estrogen-progesterone ratio influences venous distensibility. This ratio may explain the predominance of venous insufficiency symptoms on the first day of a menstrual period when a profound shift occurs from the progesterone phase of the menstrual cycle to the estrogen phase. Pathogenesis Defects in the strength and characteristics of the venous wall enter into the pathogenesis of varicose veins. Furthermore, communicating veins connecting the deep with the superficial compartment may have valve failure. Pressure studies show that two sources of venous hypertension exist. The first is gravitational and is a result of venous blood coursing in a distal direction down linear axial venous segments. This is referred to as hydrostatic pressure and is the weight of the blood column from the right atrium. The second source of venous hypertension is dynamic. It is the force of muscular contraction, usually contained within the compartments of the leg. If a perforating vein fails, high pressures (ranging from 150 to 200 mm Hg) developed within the muscular compartments during exercise are transmitted directly to the superficial venous system. Here, the sudden pressure transmitted causes dilation and lengthening of the superficial veins. Progressive distal valvular incompetence may occur. Pathogenesis : Changes occur at the cellular level. In the distal liposclerotic area, capillary proliferation is seen and extensive capillary permeability occurs as a result of the widening of interendothelial cell pores. Transcapillary leakage of osmotically active particles, the principal one being fibrinogen, occurs. The extravascular fibrin remains to prevent the normal exchange of oxygen and nutrients in the surrounding cells.However, little proof exists for an actual abnormality in the delivery of oxygen to the tissues. An other factor is the protolytic enzymes from the extravasated leukocytes VENOUS INSUFFICIENCY The C-E-A-P classification is a recent scoring system that stratifies venous disease based on clinical presentation, etiology, anatomy, and pathophysiology. C Clinical signs (grade 0–6 , supplemented by “A” for asymptomatic and “S” for symptomatic presentation E Etilogic classification (congential, primary, secondary) A Anatomic distribution (superficial, deep, or perforator, alone or in combination) P Pathophysiologic dysfunction (reflux or obstruction, alone or in combination) Clinical Classification of Chronic Lower Extremity Venous Disease Class 0 No visible or palpable signs of venous disease Class 1 Telangiectasia, reticular veins, malleolar flare Class 2 Varicose veins Class 3 Edema without skin changes Class 4 Skin changes ascribed to venous disease (e.g., pigmentation, venous eczema, lipodermatosclerosis) Class 5 Skin changes as defined above with healed ulceration Class 6 Skin changes as defined above with active ulceration Etiologic Classification of Chronic Lower Extremity Venous Disease Congenital (EC ) Cause of the chronic venous disease present since birth Primary (EP ) Chronic venous disease of undetermined cause Secondary (ES ) Chronic venous disease with an associated known cause (post-thrombotic, post-traumatic, other) ANATOMIC CLASSIFICATION (AS , AD , or AP ) The anatomic site(s) of the venous disease should be described as superficial (AS ), deep (AD ), or perforating (AP ) vein(s). One, two, or three systems may be involved in any combination. For reports requiring greater detail, the involvement of the superficial, deep, and perforating veins may be localized by use of the anatomic segments. PATHOPHYSIOLOGIC CLASSIFICATION (PR,O ) Clinical signs or symptoms of chronic venous disease result from reflux (PR ), obstruction (PO ), or both (PR,O ). Symptoms The patient with symptomatic varicose veins relates, most often, symptoms of aching, heaviness, discomfort, and sometimes pain in the calf of the affected limb. This is particularly worse at the end of the day, most likely due to prolonged sitting or standing that results in venous distention and associated pain. The symptoms are typically reduced or absent in the morning owing to the fact that the limb has not been in a dependent position through the night. In the case of women, the symptoms are often most troubling and exacerbated during the menstrual period, particularly during the first day or two. Primary varicose veins consist of elongated, tortuous, superficial veins that are protuberant and contain incompetent valves. Primary varicose veins merge imperceptibly into more severe CVI. Swelling ,edema is moderate to severe, an increased sensation of heaviness occurs with larger varicosities, and early skin changes of mild pigmentation and subcutaneous induration appear. When CVI becomes severe, marked swelling and calf pain occur after standing, sitting, or walking. Multiple dilated veins are seen associated with various clusters and heavy medial and lateral supramalleolar pigmentation. Many causes of leg pain are possible, and most may coexist. Therefore, defining the precise symptoms of venostasis is necessary. Discomfort usually occurs during warm temperatures and after prolonged standing. The pain is characteristically dull, does not occur during recumbency or early in the morning, and is exacerbated in the afternoon, especially after long standing. The discomforts of aching, heaviness, fatigue, or burning pain are relieved by recumbency, leg elevation, or elastic support. Cutaneous itching is also a sign of venostasis and is often the hallmark of inadequate external support. It is a manifestation of local congestion and may precede the onset of dermatitis. This, and nearly all the symptoms of stasis disease, can be explained by the irritation of superficial nerve fibers by local pressure or accumulation of metabolic end products with a consequent pH shift. External hemorrhage may occur as superficial veins press on overlying skin within this protective envelope. DIAGNOSTIC EVALUATION OF VENOUS DYSFUNCTION Clinical examination of the patient in good light provides nearly all the information necessary. It determines the nature of the venostasis disease and ascertains the presence of intercutaneous venous blemishes and subcutaneous protuberant varicosities, the location of principal points of control or perforating veins that feed clusters of varicosities, the presence and location of ankle pigmentation and its extent, and the presence and severity of subcutaneous induration. Visual examination can be supplemented by noting a downward-going impulse on coughing. Tapping the venous column of blood also demonstrates pressure transmission through the static column to incompetent distal veins. The modified Perthes test for deep venous occlusion . Brodie-Trendelenburg test ,and multible tornicheat test of axial reflux Those testes have been replaced by in-office use of the continuouswave, handheld Doppler instrument supplemented by duplex evaluation.The handheld Doppler instrument can confirm an impression of saphenous reflux, and this, in turn, dictates the operative procedure to be performed in a given patient. And it is used in specific locations to determine incompetent valves of perforators. Duplex technology more precisely defines which veins are refluxing by imaging the superficial and deep veins. Treatment Indications for treatment are pain, easy fatigability, heaviness, recurrent superficial thrombophlebitis, external bleeding, and appearance. Nonoperative Management The cornerstone of therapy for patients with CVI is external compression. A triple-layer compression dressing, with a zinc oxide paste gauze wrap in contact with the skin, is utilized most commonly from the base of the toes to the anterior tibial tubercle with snug, graded compression. In general, snug, graded-pressure triple-layer compression dressings effect more rapid ulcer healing than compression stockings alone. Venous Ablation: Sclerotherapy Cutaneous venectasia with vessels smaller than 1 mm in diameter do not lend themselves to surgical treatment. Dilute solutions of sclerosant (e.g., 0.2% sodium tetradecyl) can be injected directly into the vessels of the blemish. Care should be taken to ensure that no single injection dose exceeds 0.1 mL but that multiple injections completely fill all vessels contributing to the blemish. Venules larger than l mm and smaller than 3 mm in size can also be injected with sclerosant of slightly greater concentration (e.g., 0.5% sodium tetradecyl), but limiting the amount injected to less than 0.5 mL. If their cause is saphenous or tributary venous incompetence, these conditions can be treated surgically. Surgery is not indicated for the treatment of venous insufficiency in limbs with deep venous incompetence . Surgical Management Surgical treatment may be used to remove clusters with varicosities greater than 4 mm in diameter. Ambulatory phlebectomy may be performed using the stab avulsion technique with preservation of the greater and lesser saphenous veins, if they are unaffected by valvular incompetence When greater or lesser saphenous incompetence is present, the removal of clusters is preceded by limited removal of the saphenous vein (stripping). Stripping techniques are best done from above downward to avoid lymphatic and cutaneous nerve damage. Subfascial endoscopic perforator vein surgery perforating vein division using laparoscopic instrumentation. Initial data suggested that perforator interruption produced rapid ulcer healing and a low rate of recurrence. Direct Venous Reconstruction ?? DEEP VENOUS THROMBOSIS Acute deep venous thrombosis (DVT) is a major cause of morbidity and mortality in the hospitalized patient, particularly in the surgical patient. The triad of venous stasis, endothelial injury, and hypercoagulable state first posited by Virchow has held true a century and a half later. The thrombotic process initiating in a venous segment can, in the absence of anticoagulation or in the presence of inadequate anticoagulation, propagate to involve more proximal segments of the deep venous system, thus resulting in edema, pain, and immobility. The most dreaded sequel to an acute DVT is that of pulmonary embolism, a condition of potentially lethal consequence. The late consequence of DVT, particularly of the iliofemoral veins, can be CVI due to valvular dysfunction in the presence of luminal obstruction. For these reasons, understanding the pathophysiology, standardizing protocols to prevent or reduce DVT, and instituting optimal treatment promptly all are critical to reducing the incidence and morbidity of this unfortunately common condition. Etiology Stasis Soleal sinuses are the most common sites for initiation of venous thrombosis. The stasis may contribute to the endothelial cellular layer contacting activated platelets and procoagulant factors, thereby leading to DVT. The Hypercoagulable State Should any of these conditions be identified, a treatment regimen of anticoagulation is instituted for life, unless specific contraindications exist. Following major operations, large amounts of tissue factor may be released into the bloodstream from damaged tissues. Tissue factor is a potent procoagulant .Increases in platelet count, adhesiveness, changes in coagulation cascade, and endogenous fibrinolytic activity all result from physiologic stress such as major operation or trauma and have been associated with an increased risk of thrombosis. Venous Injury It has been clearly established that venous thrombosis occurs in veins that are distant from the site of operation; for instance, it is well known that patients undergoing total hip replacement frequently develop contralateral lower extremity DVT. There were multiple microtears noted within the valve cusps that resulted in the exposure of the subendothelial matrix. The exact mechanism by which this injury at a distant site occurs, and what mediators, whether cellular or humeral, are responsible is not clearly understood but that the injury occurs and occurs reliably is evident from these and other studies. Hypercoagulable States ■ Factor V Leiden mutation ■ Prothrombin gene mutation ■ Protein C deficiency ■ Protein S deficiency ■ Antithrombin III deficiency ■ Antiphospholipid syndrome Incidence Venous thromboembolism occurs for the first time in approximately 100 persons per 100,000 This incidence increases with increasing age with an incidence of 0.5% per 100,000 at 80 years of age. More than two thirds of these patients have DVT alone, and the rest have evidence of pulmonary embolism. The recurrence rate with anticoagulation has been noted to be 6% to 7% in the ensuing 6 months. Aside from pulmonary embolism, secondary CVI (that resulting from DVT) is significant in terms of cost, morbidity, and lifestyle limitation. If the consequence of DVT, in terms of pulmonary embolism and CVI, is to be prevented, the prevention, diagnosis, and treatment of DVT must be optimized. Clinical Diagnosis The diagnosis of DVT requires, to use an overused phrase, a high index of suspicion. Most are familiar with Homans’ sign, which refers to pain in the calf on dorsiflexion of the foot. It is certainly true that although the absence of this sign is not a reliable indicator of the absence of venous thrombus, the finding of a positive Homans’ sign should prompt one to attempt to confirm the diagnosis. Certainly, the extent of venous thrombosis in the lower extremity is an important factor in the manifestation of symptoms. For instance, most calf thrombi may be asymptomatic unless there is proximal propagation. Only 40% of patients with venous thrombosis have any clinical manifestations of the condition. Major venous thrombosis involving the iliofemoral venous system results in a massively swollen leg with pitting edema, pain, and blanching, a condition known as phlegmasia alba dolens. With further progression of disease, there may be such massive edema that arterial inflow can be compromised. This condition results in a painful blue leg, the condition called phlegmasia cerulea dolens. With this evolution of the condition, unless flow is restored, venous gangrene can develop. Investigation Duplex Ultrasound. The modern diagnostic test of choice for the diagnosis of DVT is the duplex ultrasound, a modality that combines. Real time B-mode ultrasonography with color-flow imaging has improved the sensitivity and specificity of ultrasound scanning. With color-flow duplex imaging, blood flow can be imaged in the presence of a partially occluding thrombus. The probe is also used to compress the vein: A normal vein should be easily compressed, whereas in the presence of a thrombus, there is resistance to compression. Magnetic Resonance Venography. With major advances in technology of imaging, magnetic resonance venography has come to the forefront of imaging for proximal venous disease. The cost and the issue of patient tolerance due to claustrophobia limit the widespread application, but this is changing. It is a useful test for imaging the iliac veins and the inferior vena cava, an area where duplex ultrasound is limited in its usefulness. Prophylaxis The patient who has undergone either major abdominal surgery, major orthopedic surgery, has sustained major trauma, or has prolonged immobility (>3 days) represents a patient who has an elevated risk for the development of venous thromboembolism. The methods of prophylaxis can be mechanical or pharmacologic. The simplest method is for the patient to be able to walk. Activation of the calf pump mechanism is an effective means of prophylaxis. A patient who is expected to be up and walking within 24 to 48 hours is at low risk of developing venous thrombosis. The practice of having a patient “out of bed into a chair” is one of the most thrombogenic positions that one could order a patient into. Sitting in a chair with the legs in a dependent position causes venous pooling, which in the postoperative milieu could be easily a predisposing factor in the development of thromboembolism. The most common method of prophylaxis in the surgical universe has traditionally revolved around sequential compression devices, which periodically compress the calves and essentially replicate the calf bellows mechanism. This has clearly reduced the incidence of venous thromboembolism in the surgical patient. Heparin “Minidose” heparin the dose traditionally used is 5000 units of unfractionated heparin every 12 hours. When subcutaneous heparin is used on an every-8-hour dosing, rather than every 12 hours, there is a reduction in the development of venous thromboembolism. More recently, fractionated low-molecular-weight heparin (LMWH) for prophylaxis and treatment of venous thromboembolism. LMWH inhibits factors Xa and IIA activity, with the ratio of antifactor Xa to antifactor IIA activity ranging from 1:1 to 4:1. LMWH has a longer plasma half-life and has significantly higher bioavailability. There is much more predictable anticoagulant response than heparin. No laboratory monitoring is necessary because the partial thromboplastin time (PTT) is unaffected. LMWH results less bleeding complications. In short, LMWH should be considered the optimal method of prophylaxis in moderate and high-risk patients. TREATMENT Traditionally, the treatment of DVT centers around heparin treatment to maintain the PTT at 60 to 80 seconds, followed by warfarin therapy to obtain an International Normalized Ratio (INR) of 2.5 to 3.0. A widely used regimen is 80 U/kg bolus of heparin, followed by a 15 U/kg infusion. The PTT should be checked 6 hours after any change in heparin dosing. Warfarin is started the same day. If warfarin is initiated without heparin, the risk of a transient hypercoagulable state exists, because proteins C and S levels fall before the other vitamin K– dependent factors are depleted. With the advent of LMWH, it is no longer necessary to admit the patient for intravenous heparin therapy. It is now accepted practice to administer LMWH to the patient as an outpatient, as a bridge to warfarin therapy. A minimum treatment time of 3 months is advocated in most cases. If, however, the patient has a known hypercoagulable state or has experienced episodes of venous thrombosis, then lifetime anticoagulation is required, in the absence of contraindications. The accepted INR range is 2.0 to 3.0. Oral anticoagulants are teratogenic and thus cannot be used during pregnancy. In the case of the pregnant woman with venous thrombosis, LMWH is the treatment of choice, and this is continued through delivery and can be continued postpartum if needed. Thrombolysis The advent of thrombolysis has resulted in increased interest in thrombolysis for DVT. The purported benefit is preservation of valve function with subsequently lesser chance of developing CVI. However, to date, little definitive, convincing data exist to support the use of thrombolytic therapy for DVT. One exception is the patient with phlegmasia in whom thrombolysis is advocated for relief of significant venous obstruction. In this condition, thrombolytic therapy probably results in better relief of symptoms and less long-term sequelae than heparin anticoagulation alone. The alternative for this condition is surgical venous thrombectomy. No matter which treatment is chosen, long-term anticoagulation is indicated. The incidence of major bleeding is higher with lytic therapy. Vena Caval Filter The most worrisome and potentially lethal complication of DVT is pulmonary embolism. The symptoms of pulmonary embolism, ranging from dyspnea, chest pain, and hypoxia to acute cor pulmonale are nonspecific and require a vigilant eye for the diagnosis to be made. The gold standard remains the pulmonary angiogram, but increasingly this is being displaced by the computed tomographic angiogram. Adequate anticoagulation is usually effective in stabilizing venous thrombosis, but if a patient should develop a pulmonary embolism in the presence of adequate anticoagulation, a vena cava filter is indicated. The modern filters are placed percutaneously over a guide wire. The Greenfield filter, with the most extensive use and data, has a 95% patency rate and a 4% recurrent embolism rate. This high patency rate allows for safe suprarenal placement if there is involvement of the inferior vena cava up to the renal veins or if it is placed in a woman of childbearing potential. The device-related complications are wound hematoma, migration of the device into the pulmonary artery, and caval occlusion due to trapping of a large embolus. In the latter situation, the dramatic hypotension that accompanies acute caval occlusion can be mistaken for a massive pulmonary embolism. The distinction between the hypovolemia of caval occlusion versus the right heart failure from pulmonary embolism can be arrived at by measuring filling pressures of the right side of the heart. The treatment of caval occlusion is volume resuscitation. Indications for a Vena Cava Filter ■ Recurrent thromboembolism despite “adequate” anticoagulation ■ Deep venous thrombosis in a patient with contraindications to anticoagulation ■ Chronic pulmonary embolism and resultant pulmonary hypertension ■ Complications of anticoagulation ■ Propagating iliofemoral venous thrombus in anticoagulation Pulmonary Thromboembolism • DVT is most common source of PE; <10% of PE cases cause pulmonary infarction • Symptoms and signs include dyspnea and chest pain (present in 75%); tachycardia, tachypnea, altered mental status; classic triad of dyspnea, chest pain, and hemoptysis in only 15%; pleural rub and S1Q3T3 rarely found • V˙ /Q˙ scan has sensitivity and specificity of 90%, but 67% of studies are inconclusive; spiral computed tomography is more accurate Differential Diagnosis • Other causes of chest pain and hypoxia, such as pneumonia Treatment • Stabilize initially with pressors and ventilatory support; start heparin or lowmolecular-weight heparin quickly • Surgery: consider IVC filter if risk of embolus is ongoing and anticoagulation is risky • Open surgical thrombectomy (Trendelenburg procedure): high mortality, rarely clinically useful for massive saddle embolus • Prevention: DVT prophylaxis in perioperative period Superficial Thrombophlebitis Can occur spontaneously in varicose veins, post traumatic, pregnant or postpartum women, thromboangiitis obliterans, Behçet disease; superficial migratory phlebitis (Trousseau) suggests abdominal carcinoma Symptoms and signs include local extremity pain, redness; indurated, erythematous, tender areas indicate thrombosed superficial veins; well localized over superficial vein Differential Diagnosis • Ascending lymphangitis • Cellulitis Treatment • Primary treatment includes nonsteroidal anti-inflammatory drugs, heat, elevation, support stockings, elastic wrap; ambulation is encouraged • Surgery: excise vein if condition persists >2 weeks or recurs; ligate and resect vein at saphenofemoral or cephalic-subclavian junction Prognosis: uncomplicated superficial thrombophlebitis responds well to conservative therapy; extension into DVT may be associated with PE Leg ulcer An ulcer is defined as an area of discontinuity of the surface epithelium. Venous ulcers • Venous hypertension secondary to DVT or varicose veins: ulceration on the medial side of the leg, above the ankle, any size, shallow with sloping edges, bleeds after minor trauma, weeps readily, surrounded by pigmentation associated dermatoliposclerosis. Arterial ulcers Occlusive arterial disease: painful ulcers, do not bleed, nonhealing, lateral ankle, heel, metatarsal heads, tips of the toes, associated features of ischaemia, e.g. claudication, absent pulses, pallor. Elderly patients may present with ‘blue toe’ syndrome. Diabetic ulcers • Ischaemic: same as arterial ulcers. • Neuropathic: deep, painless ulcers, plantar aspect of foot or toes, associated with cellulitis and deep tissue abscesses, warm foot, pulses may be present. Lymphatic Disorders Lymphedema Excessive and persistent accumulation of extravascular and extracellular fluid and proteins in tissue spaces Caused by a disturbance of the water and protein balance across the capillary membrane Increased concentration of proteins draws greater amount of water into interstitial spaces Exceeds transport capacity of the lymphatic system, leading to lymphedema Disorders of the Lymphatic System Leading to Lymphatic Insufficiency Primary Congenital Malformation(congenita, praecox &tarda) Secondary: Infection and Inflammation Obstruction or Fibrosis Trauma, Surgery, Neoplasms Radiation Therapy Surgical Dissection of Lymph Nodes Chronic Venous Insufficiency Clinical Signs and Symptoms of Lymphedema Edema of the dorsum of the foot or hand Decreased range of motion, flexibility and function Usually unilateral Worse after prolonged dependency No discomfort or a dull, heavy sensation; sense of fullness Clinical Manifestations of Lymphatic Disorders Lymphedema Increased girth and weight of the limb Sensory disturbances Stiffness and limited range of motion Decreased resistance to infection Lymphedema Location Severity of Lymphedema Mild lymphedema: One to two cm increase in girth measurements between the involved and non-involved limb Moderate lymphedema: Two to five cm increase in girth measurement Severe lymphedema: Greater than five cm increase Components of a Decongestive Lymphatic Therapy Program Elevation Manual lymphatic drainage Compression Exercise Skin care Daily living precautions Elevation Elevate the involved limb when using a sequential compression pump Elevate limb when sleeping, resting, and during sedentary activities Compressive bandages or garment should be worn during periods of elevation Manual Lymphatic Drainage Slow, very light, repetitive stroking and circular massage movements performed in a specific sequence, limb elevated whenever possible Proximal congestion in the trunk, groin, buttock, or axilla is cleared first Direction of massage is towards specific lymph nodes Usually involves distal to proximal stroking Manual Lymphatic Drainage Manual Lymphatic Drainage Exercise Active range of motion, stretching, and low-intensity resistance exercise is incorporated with manual drainage techniques Exercises should be performed with compressive bandages or garment Exercise Compression No-stretch, non-elastic or low-stretch elastic bandages are used Sports bandages, such as ACE wraps, are NOT recommended in the treatment of lymphedema Compressive garments are available Use of a sequential, pneumatic compression pump on a daily basis may be recommended Bandages Compressive Bandages Skin Care and Hygiene Lymphedema increases risk of skin breakdown, infection, and delayed wound healing Proper skin care Inspection Protection