Clinical Pharmacology Spring Course 2006
advertisement

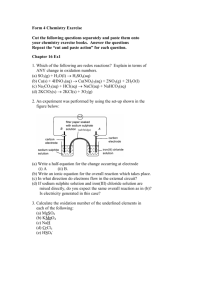
Drug Metabolism Clinical Pharmacology Spring Course 2006 M. E. Blair Holbein, Ph.D. Clinical Pharmacologist Presbyterian Hospital 1 Drug Metabolism - History “Xenobiotic metabolism” established by Richard Tecwyn Williams First paper with an identified “metabolite” in Nature 1931 Wrote first book on the Detoxification Mechanisms” 1959 Focus on elimination of foreign compounds Proposed a delineation of: Phase I (oxidation, reduction, hydrolysis) biotransformations as primary covalent chemical modifications to administered compound Phase II (conjugation) with an endogenous polar species To either parent drug Phase I product(s) 2 Biotransformations Phase I Oxidation Cytochrome P450 monooxygenase system Flavin-containing monooxygenase system Alcohol dehydrogenase and aldehyde dehydrogenase Monoamine oxidase (Co-oxidation by peroxidases) Reduction NADPH-cytochrome P450 reductase Reduced (ferrous) cytochrome P450 Hydroloysis Esterases and amidases Epoxide hydrolase Phase II Glutathione S-transferases Mercapturic acid biosynthesis UDP-Glucoron(os)yltranasferases N-Acetyltransferases Amino acid N-acyl transferases Sulfotransferases 3 Biotransformations Phase I Oxidation Cytochrome P450 monooxygenase system Flavin-containing monooxygenase system Alcohol dehydrogenase and aldehyde dehydrogenase Monoamine oxidase (Co-oxidation by peroxidases) Reduction NADPH-cytochrome P450 reductase Reduced (ferrous) cytochrome P450 Hydroloysis Esterases and amidases Epoxide hydrolase Phase II Glutathione S-transferases Mercapturic acid biosynthesis UDP-Glucoron(os)yltranasferases N-Acetyltransferases Amino acid N-acyl transferases Sulfotransferases 4 Biotransformations Phase I Oxidation Cytochrome P450 monooxygenase system Flavin-containing monooxygenase system Alcohol dehydrogenase and aldehyde dehydrogenase Monoamine oxidase (Co-oxidation by peroxidases) Reduction NADPH-cytochrome P450 reductase Reduced (ferrous) cytochrome P450 Hydroloysis Esterases and amidases Epoxide hydrolase Phase II Glutathione S-transferases Mercapturic acid biosynthesis UDP-Glucoron(os)yltranasferases N-Acetyltransferases Amino acid N-acyl transferases Sulfotransferases 5 Drug Metabolism - Determinants of Activity Inhibition of enzyme activity Patterns Competitive Noncompetitive Uncompetitive Effects not mediated by enzyme activity, e.g. free fraction, membrane effects, etc. Inducibility Rate-limitations Substrates First-pass metabolism, high-extraction drugs Co-factors Turnover Polymorphism Predictability of in vivo effects based on in vitro data is highly variable 6 Kinetic equations for inhibition of metabolizing enzymes 7 Drug Metabolism - Determinants of Activity Inhibition of enzyme activity Patterns Competitive Noncompetitive Uncompetitive Effects not mediated by enzyme activity, e.g. free fraction, membrane effects, etc. Inducibility Rate-limitations Substrates First-pass metabolism, high-extraction drugs Co-factors Turnover Polymorphism Predictability of in vivo effects based on in vitro data is highly variable 8 Biotransformations Phase I Oxidation Cytochrome P450 monooxygenase system Flavin-containing monooxygenase system Alcohol dehydrogenase and aldehyde dehydrogenase Monoamine oxidase (Co-oxidation by peroxidases) Reduction NADPH-cytochrome P450 reductase Reduced (ferrous) cytochrome P450 Hydroloysis Esterases and amidases Epoxide hydrolase Phase II Glutathione S-transferases Mercapturic acid biosynthesis UDP-Glucoron(os)yltranasferases N-Acetyltransferases Amino acid N-acyl transferases Sulfotransferases 9 Phase I Oxidation: Cytochrome P450 Isoenzymes Background: Huge superfamily of highly versatile enzymes (over 3800 sequences identified) Found in the genomes of virtually all organisms Heme-containing proteins named for the absorption band at 450 nm when combined with carbon monoxide NADP(H) used with molecular oxygen to produce oxidation of a variety of compounds: Xenobiotics Endobiotics In prokaryotes, P450s are soluble proteins. In eukaryotes, they are usually bound to the endoplasmic reticulum or inner mitochondrial membranes. Human drug metabolism primarily in the endoplasmic reticulum of hepatocytes. Also in the small intestine, kidney, lung and brain. More than thirty (30) CYP human isoenzymes have been identified. 10 Catalytic reaction cycle CYP450 and the oxidation of xenobiotics OH e- NADP+ NADP DRUG CYP Reductase Fe3+ CYP DRUG CYP Fe3+ CYP Fe2+ OH DRUG DRUG e- O2 O2 CYP Fe2+ DRUG H2O 2H+ 11 Catalytic reaction cycle involving cytochrome P450 in the oxidation of xenobiotics Drug + NADPH + H+ + O2 Oxidized Drug + NADP+ + H2O 12 CYP450 Mediated Chemical Transformation Hydroxylation Aliphatic Aromatic N-Dealkylation, O-Dealkylation, S-Dealkylation Oxidative Deamination Dehalogenation N-Oxidation S-Oxidation 13 CYP Mediated Oxidation Aliphatic Hydroxylation RCH2CH3 OH RCHCH3 Ex: Hydroxylation of ibuprofen 14 CYP Mediated Oxidation Aromatic Hydroxylation Ex: Hydroxylation of acetanilide to 4-hydroxyacetanilide 15 CYP Mediated Oxidation Aromatic Hydroxylation Directly through asymmetric oxygen transfer Through an unstable arene oxide intermediate Predictability Influence of environment Ex:Hydroxylation of aromatic carbon atoms 16 CYP Mediated Oxidation Aromatic Results Hydroxylation in several oxidized metabolites Ex:Metabolism of phenytoin 17 CYP Mediated Oxidation Dealkation (N-, O-, S-) Ex: N-demethylation of ethylmorphine 18 CYP Mediated Oxidation N-demethylation generates formaldehyde as a by-product 19 CYP Mediated Oxidation Dealkation (N-, O-, S-) Ex: N-demethylation and hydroxylation of propranolol 20 CYP Mediated Oxidation Oxidative Deamination Ex: General mechanism for oxidative deamination 21 CYP Mediated Oxidation Oxidative Deamination Ex: Deamination of amphetamine to inactive ketone 22 CYP Mediated Oxidation Dehalogenation Ex: Dehalogenation generates reactive free radicals. Metabolism of carbon tetrachloride generates oxidized lipids 23 CYP Mediated Oxidation N-Oxidation may produce toxic by-products 24 CYP Mediated Oxidation N-Oxidation Ex: N-oxidation of Dapsone 25 CYP Mediated Oxidation S-Oxidation Ex: General scheme Ex: CYP3A and Flavin monooxygenase produce same metabolite 26 CYP Mediated Oxidation S-Oxidation Ex: A-oxidation of tazofelone 27 Drug Metabolism CYP450 Cytochrome P450 system responsible for the majority of oxidative reactions Significant polymorphism in many. Drugs may be metabolized by a single isoenzyme CYP2C9, CYP2C19, and CYP2D6—can be even be genetically absent! Desipramine/CYP2D6; indinavir/CYP3A4; midazolam/CYP3A; caffeine/CYP1A2; omeprazole/CYP2C19 Drugs may be metabolized by multiple isoenzymes Most drugs metabolized by more than one isozyme Imipramine: CYP2D6, CYP1A2, CYP3A4, CYP2C19 If co-administered with CYP450 inhibitor, some isozymes may “pick up slack” for inhibited isozyme. Drugs may be metabolized by several different enzyme systems; e.g. CYP450 and MFO. This enzyme system notably susceptible to induction. Inherent turnover; highly variable response 28 Cytochrome P450 (CYP) Isoenzymes All CYP isoenzymes in the same family have at least 40% structural similarity, and those in the same subfamily have at least 60% structural similarity. Nomenclature ex: CYP2D6 Root: cytochrome P450 CYP Genetic Family: CYP2 Genetic Subfamily: CYP2D Specific Gene: CYP2D6 NOTE that this nomenclature is genetically based; it has NO functional implication Phase I Oxidation: Cytochrome P450 (CYP) Isoenzymes 29 Proportion of Drugs Metabolized by CYP450 Enzymes in Humans CYP2D6 20% CYP3A4 38% CYP2C19 8% CYP1A2 11% CYP2C9 16% CYP2E1 4% CYP2A6 3% 30 Cytochrome P450 3A4,5,7 Largest number of drugs metabolized Present in the largest amount in the liver. Present Not in GI tract polymorphic Inherent activity varies widely Activity has been shown to predominate in the gut. Substrates: Most calcium channel blockers: nifedipine, amlodipine; HMG Co A Most benzodiazepines: diazepam, midazolam Most HIV protease inhibitors: indinavir, ritonavir Most HMG-CoA-reductase inhibitors: atorvastatin, lovastatin Cyclosporine, tacrolimus Most non-sedating antihistamines Cisapride Macrolide antibiotics: clarithromycin, erythromycin Chlorpheniramine; Also: haloperidol, buspirone; sildenafil, tamoxifen, trazodone, vincristine 31 Mechanism of Induction of CYP3A4-Mediated Metabolism of Drug Substrates (Panel A) Wilkinson, G. R. N Engl J Med 2005;352:2211-2221 The Resulting Reduced Plasma Drug Concentration (Panel B) Cytochrome P450 2D6 Second largest number of substrates. Polymorphic distribution Majority of the population is characterized as an extensive or even ultra-extensive metabolizer. Approximately 7% of the U.S. Caucasian population and 1-2% of African or Asian inheritance have a genetic defect in CYP2D6 that results in a poor metabolizer phenotype. include: many beta-blockers – metoprolol, timolol, amitriptylline, imipramine, paroxetine, haloperidol, risperidone, thioridazine, codeine, dextromethorphan, ondansetron, tamoxifen, tramadol Inhibited by: amiodarone, chlorpheniramine, cimetidine, fluoxetine, ritonavir Substrates 33 Common Drug Substrates and Clinically Important Inhibitors of CYP2D6 Wilkinson, G. R. N Engl J Med 2005;352:2211-2221 Cytochrome P450 2C9 Note: Absent in 1% of Caucasian and African- Americans. Substrates include: many NSAIDs – ibuprofen, tolbutamide, glipizide, irbesartan, losartan, celecoxib, fluvastatin, phenytoin, sulfamethoxazole, tamoxifen, tolbutamide, warfarin Inhibited by: fluconazole, isoniazid, ticlopidine Induced by: rifampin 35 Cytochrome P450 1A2 Substrates include: theophylline, caffeine, imipramine, clozapine Inhibited by: many fluoroquinolone antibiotics, fluvoxamine, cimetidine Induced by: smoking tobacco 36 37 Coffee Intake and Relative Risk of Myocardial Infarction by CYP1A2 Genotype Cornelis, M. C. et al. JAMA 2006;295:1135-1141. Copyright restrictions may apply. 38 Cytochrome P450 2C19 Note: Absent in 20-30% of Asians, 3-5% of Caucasians Substrates include: omeprazole, diazepam, phenytoin, phenobarbitone, amitriptylline, clomipramine, cyclophosphamide, progesterone Inhibited by: fluoxetine, fluvoxamine, ketoconazole, lansoprazole, omeprazole, ticlopidine 39 Cytochrome P450 2B6 Substrates include: bupropion, cyclophosphamide, efavirenz, methadone Inhibited by: thiotepa Induced by: phenobarbital, rifampin 40 Cytochrome P450 2E1 Substrates include: acetaminophen 41 Cytochrome P450 2C8 Substrates; paclitaxel, torsemide, amodiaquine, cerivastatin, repaglinide Inhibited by: trimethoprim, quercetin, glitazones, gemfibrozil, montelukast Induced by: rifampin 42 Biotransformations Phase I Oxidation Cytochrome P450 monooxygenase system Flavin-containing monooxygenase system Alcohol dehydrogenase and aldehyde dehydrogenase Monoamine oxidase (Co-oxidation by peroxidases) Reduction NADPH-cytochrome P450 reductase Reduced (ferrous) cytochrome P450 Hydroloysis Esterases and amidases Epoxide hydrolase Phase II Glutathione S-transferases Mercapturic acid biosynthesis UDP-Glucoron(os)yltranasferases N-Acetyltransferases Amino acid N-acyl transferases Sulfotransferases 43 Non-CYP Mediated Chemical Transformation Hydrolysis Reduction Oxidations Flavine monooxygenases Monoamine and diamine oxidases Alcohol and aldehyde dehydrogenase 44 Non-CYP Mediated Biotransformation Hydrolysis Esterases, amidases and proteases Non-microsomal (cytosolic) Widely distributed in most tissues 45 Non-CYP Mediated Biotransformation Reduction Ex: Reduction of side-chain of digoxin produces inactive metabolite 46 Non-CYP Mediated Chemical Transformation Hydrolysis Reduction Oxidations Flavine monooxygenases Monoamine and diamine oxidases Alcohol and aldehyde dehydrogenase 47 Flavine Monooxygenases Wide variety of substrates First isolated from pig liver Originally termed N-oxidase (or Ziegler’s enzyme) Products are generally polar, non-toxic compounds Some generation of reactive intermediates, esp. S-oxides 48 Flavine Monooxygenases Isoenzymes Six genes in mammals Nomenclature based on sequence homology FMO1: major human fetal liver; adult kidney FMO2: lung (most species) FMO3: major adult liver form; major form in brain Interindividual variability FMO4: atypical FMO5: trace FMO6: reported Question of inducibility (vs. P450) Genetic polymorphism 49 Flavine Monooxygenases Reactions S-Oxygenation Spironolactone Cimetidine Stereoselective: FMO3 forms the (+) enantiomer and FMO1 forms () enantiomer N-Oxygenation Imipramine Nicotine 50 Flavine Monooxygenases Mechanism Requires O2 and NADPH Unlike P450 which forms oxidizing intermediate AFTER binding substrate, FMO exists in “preloaded” state and will oxygenate any lipophilic substrate that binds with it. Individual FMOs have broader substrate range than individual CYP 51 Flavine Monooxygenase Cycle NADP+ + H 2O Enz | Flox NADPH FMO Cycle Enz | FlH2 + NADP+ Enz | FlHOH O2 Enz | FlOOH DRUG - O DRUG 52 Catalytic reaction cycle CYP450 and the oxidation of xenobiotics OH e- NADP+ NADP DRUG CYP Reductase Fe3+ CYP DRUG CYP Fe3+ CYP Fe2+ OH DRUG DRUG e- O2 O2 CYP Fe2+ DRUG H2O 2H+ 53 Flavine Monooxygenase Cycle NADP+ + H 2O Enz | Flox NADPH FMO Cycle Enz | FlH2 + NADP+ Enz | FlHOH O2 Enz | FlOOH DRUG - O DRUG 54 Non-CYP Mediated Oxidation Oxidation: Flavine Monooxygenases Ex: N-Oxidation of nicotine, catalyzed by FMO3 55 Non-CYP Mediated Oxidation Oxidation: Flavine Monooxygenases Ex: S-Oxidation of cimetidine, catalyzed by FMO3 56 Non-CYP Mediated Chemical Transformation Hydrolysis Reduction Oxidations Flavine monooxygenases Monoamine and diamine oxidases Alcohol and aldehyde dehydrogenase 57 Non-CYP Mediated Oxidation Oxidation: Monoamine Oxidases Mitochondrial enzymes Deaminate endogenous neurotransmitters Dopamine Serotonin Norepinephrine Epinephrine Same type of products as other oxidizing enzymes Distinguish Found source enzyme of metabolites by other means in liver, kidney, intestine, brain 58 Non-CYP Mediated Oxidation Oxidation: Diamine Oxidases Endogenous amines Histamine Polyamines Putrescine Cadaverine Amines converted to aldehydes (in presence of O2) Contribute to oxidation of some drugs Found in liver, intestine, placenta 59 Non-CYP Mediated Chemical Transformation Hydrolysis Reduction Oxidations Flavine monooxygenases Monoamine and diamine oxidases Alcohol and aldehyde dehydrogenase 60 Non-CYP Mediated Oxidation Alcohol and Aldehyde Dehydrogenases Ex: Products of alcohol dehydrogenase are substrates for aldehyde dehydrogenase. 61 Non-CYP Mediated Oxidation Alcohol and Aldehyde Dehydrogenases Ex: Products of alcohol dehydrogenase are substrates for aldehyde dehydrogenase. 62 Relative Contribution to Drug Metabolism - Phase I Evans & Relling Science 1999 Phase II Biotransformation: Conjugation: Glucuronidation, Sulfation, Acetylation Addition of hydrophilic groups (glucuronic acid, sulfate, glycine, or acetyl) onto the drug or drug metabolite Catalyzed by a group of enzymes called transferases. Located in cytosol Microsomal enzyme: Uridine diphosphate glucuronosyltransferase (UGTs) 64 Biotransformations Phase I Oxidation Cytochrome P450 monooxygenase system Flavin-containing monooxygenase system Alcohol dehydrogenase and aldehyde dehydrogenase Monoamine oxidase (Co-oxidation by peroxidases) Reduction NADPH-cytochrome P450 reductase Reduced (ferrous) cytochrome P450 Hydroloysis Esterases and amidases Epoxide hydrolase Phase II Glutathione S-transferases UDP-Glucoron(os)yltranasferases N-Acetyltransferases Amino acid N-acyl transferases Sulfotransferases 65 Phase II Biotransformations (Conjugations) Glutathione Catalyzed by glutathione-S-transferases Cytosolic and microsomal Detoxification of electrophilic (and potentially carcinogenic) molecules 66 UDP-Glucuronosyltransferase (UGT) Catalyses conjugation of glucuronic acid with a substrate with a suitable functional group The most important (quantitatively) conjugation step Substrates Xenobiotics (drugs, dietary chemicals, carcinogens, environmental pollutants) Endobiotics (steroid hormones, bilirubin, bile acids, fatty acids) Altered activity important (toxicology, pharmacologically) Microsomal location in endoplasmic reticulum on opposite side of membrane from CYP Transporter functions for cofactors Polymorphic (at least two families) Rare disorders associated with genetic abnormalities Criglar-Najjar Syndromes (types1,2) Absence of bilirubin conjugation enzyme and marked unconjugated hyperbilirubinemia & jaundice Gilbert Syndrome Partial block in bilirubin conjugation; benign elevation in total and unconjugated bilirubin 67 Phase II Biotransformations (Conjugations) Glucuronidation Ex: N- and O- linked glucuronide formation markedly enhances the polarity and water solubility. 68 Phase II Biotransformations (Conjugations) Glucuronides can be generated from a variety of substrates 69 Phase II Biotransformations (Conjugations) Sulfation General pathway for enzymatic sulfation 70 Phase II Biotransformations (Conjugations) Sulfation Ex: Minoxidil 71 Phase II Biotransformations (Conjugations) Acetylation Ex: Acetyl transferase donates the acyl group from Coenzyme A to drug substrates 72 Phase II Biotransformations (Conjugations) Acetylation Ex: Isoniazid inactivation by acetylation 73 Phase II Biotransformations (Conjugations) Hydroxylation and acetylation Ex: Reactive nitrenium ions may be produced in the metabolism of aromatic amines through hydroxylation and acetylation 74 Biotransformations Phase I Oxidation Cytochrome P450 monooxygenase system Flavin-containing monooxygenase system Alcohol dehydrogenase and aldehyde dehydrogenase Monoamine oxidase (Co-oxidation by peroxidases) Reduction NADPH-cytochrome P450 reductase Reduced (ferrous) cytochrome P450 Hydroloysis Esterases and amidases Epoxide hydrolase Phase II Glutathione S-transferases UDP-Glucoron(os)yltranasferases N-Acetyltransferases Amino acid N-acyl transferases Sulfotransferases 75 Questions? Blair Holbein, Ph.D., BCAP Presbyterian Hospital of Dallas Email: bholbein@hcin.net Website: http://phdres.caregate.net Annotated bibliography 76 References Wright JM. Drug Interactions. Carruthers SG, Hoffman BB, et al.s, ed. Melmon and Morrelli’s Clinical Pharmacology: Basic Principles in Therapeutics, 4th ed. New York 2000 :McGraw-Hill. In: Markey SM.Pathways of Drug Metabolism In: Atkinson AJ, Daniels CE, Dedrick RL, et al., ed. Principles of Clinical Pharmacology, New York 2001: Academic Press. 77