Optimal intakes of alpha-linolenic acid for heart health
advertisement

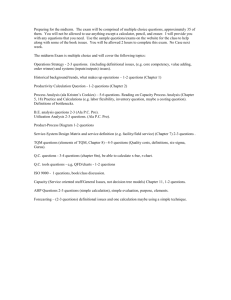
Unilever Health & Wellbeing Series Optimal intakes of alpha-linolenic acid for heart health There is convincing evidence and scientific consensus that replacing saturated fatty acids (SAFA) with polyunsaturated fatty acids (PUFA) in the diet decreases the risk of coronary heart disease (CHD). Although omega-6 (linoleic acid (LA) is the major dietary PUFA, it is acknowledged that both omega-6 and omega-3 PUFA are important for heart health. The two types of omega-3 fatty acids in the diet, ‘vegetable’ omega-3 fatty acid (alpha-linolenic acid (ALA) and ‘marine’ omega-3 fatty acids (eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are both reported to have beneficial effects on heart health. Although ALA is the most abundant omega-3 fatty acid in the diet, most research has focused on the heart health benefits of EPA&DHA. Although the evidence is less strong and extensive than for EPA & DHA, the available evidence supports a beneficial effect of ALA on heart health. Authors: Ans Eilander and Peter Zock (Unilever R&D) Scientific review ALA is the most abundant omega-3 fatty acid in the diet Polyunsaturated fatty acids (PUFA) can be classified into two groups: omega-3 and omega-6 fatty acids. There is convincing evidence and consensus that replacing saturated fatty acids (SAFA) with PUFA in the diet decreases the risk of CHD, with an estimated 10% reduction in CHD for each increase of 5% of energy in PUFA at the expense of SAFA (1-4). It has been suggested that this beneficial effect of PUFA as observed in randomized controlled trials (RCTs) should mainly be attributed to the omega-3 fatty acids and that increasing omega-6 fatty acid intake alone is not effective and would be even harmful (5). However, the available evidence is too limited to disentangle the effect of omega-6 and omega-3 PUFA, The vegetable oils and diets investigated in the RCTs contained all mainly omega-6 PUFA, which make them a likely candidate for the beneficial effect of vegetable PUFA. Moreover, several health authorities recognise that both omega-6 and omega-3 fatty acids are important for maintenance of healthy cholesterol levels, thereby decreasing the risk of CHD (2;6;7). ALA (C18:3n-3), an essential fatty acid, is the predominant omega-3 PUFA in the diet. As it cannot be synthesised in the body it is considered an essential nutrient and must be obtained from the diet. ALA is mainly found in a variety of vegetable oils (in particular rapeseed (canola), flaxseed and soybean), seeds and nuts. The other type of major omega-3 fatty acids in the diet are called long chain (LC) PUFA or marine omega-3 fatty acids (e.g. mainly present in seafood and fish oils), which are for the largest part eicosapentaenoic acid (EPA, C20:5n-3) and docosahexaenoic acid (DHA, C22:6n-3). However, EPA+DHA can also be obtained by conversion (elongation and desaturation) from ALA in the human body. These fatty acids are important structural constituents of membranes and tissues and play a vital role in many physiological and molecular processes. Higher intakes of EPA+DHA have been linked to many health outcomes, including brain development and function, cardiovascular health and inflammatory response. The evidence for a protective effect of intake of fish and its omega-3 fatty acids (EPA+DHA) on cardiovascular disease (CVD) and in Optimal intakes of alpha-linolenic acid for heart health (2011) particular (fatal) heart disease is well documented and considered strong for primary prevention in the general population. ALA is a precursor for EPA and DHA, but conversion is limited It is unclear, whether the essentiality of ALA is due to the action of ALA itself or to ALA being a precursor for EPA+DHA. In a critical review of human studies, the conversion of ALA to EPA was estimated to be a modest 8%; while the extent of conversion to DHA was much smaller at 0.05% (8). Furthermore, the conversion of ALA to EPA+DHA varies between people and is likely to be influenced by gender and the absolute amounts of ALA and LA in the diet (9;10). The consensus is that conversion of ALA to EPA+DHA in humans is limited with an average overall conversion rate of about 4-5% (11). For optimal heart health an omega-3 fatty acid intake up to 2% of dietary energy (en%) is recommended, of which at least 250 mg should come from EPA+DHA. It is important to consider that ALA intake recommendations are set both in the context of adequate intakes needed to prevent deficiencies and more recently as optimal intakes needed to prevent chronic diseases, in particular cardiovascular disease (CVD). To prevent deficiency symptoms, a minimum intake of >0.5 en% ALA is recommended for adults ((2). This intake level is easily achieved in a balanced diet and in the general population ALA deficiency is rarely observed. FAO (2) recommends that diets should provide between 0.5 and 2.0 en% of total omega-3 fatty acids, of which the higher value includes the recommendation for ALA and that for EPA+DHA of 0.25-2.0 g/d as part of a healthy diet. ALA intakes are often lower than recommended for optimal heart health A concern is that average ALA intake levels of adults and children are generally below levels recommended for optimal heart health. Available intake data from National Dietary Surveys indicate that average ALA intakes in different populations range from 0.5-1 en%, so ALA intake should be increased to reach the level recommended for optimal heart health (Harika et al, submitted). Possible adverse effects are unlikely Adverse effects of ALA intake have hardly been reported (12). A link between ALA concentrations and increased prostate cancer risk has been suggested, but a causal relation is not considered likely (13). A recent meta-analysis of 8 case-control and 8 prospective studies with inconsistent findings showed a borderline statistically significant higher risk of prostate cancer with high ALA intakes. However, these associations disappeared after adjustment for heterogeneity and publication bias (14). Clinical and prospective studies suggest that ALA intake reduces the incidence of CHD Most studies on effects of omega-3 on heart health have focused on the long-chain omegas EPA+DHA. This is evident from a systematic review that identified far more studies examining the effects of EPA+DHA or fish consumption on CVD outcomes than studies on effects of ALA (12). The potential of ALA to affect CVD risk, in particular coronary heart disease (CHD), has been studied in only a few clinical endpoints trials and in about 10 high quality, epidemiologic studies. One early primary trial did not find and effect on CHD incidence, possibly because duration of the study (1 year) was too short (15). The results of the Lyon Heart Study, a secondary prevention trial, indicate that a Mediterranean diet enriched with ALA can significantly lower the risk of cardiovascular death (16;17). The intake of ALA in the intervention diet was over 0.6 en%, which was about 1.8g/d ALA, compared with 0.7g ALA in the control diet. However, a major limitation of this trial is that multiple changes were made in the diet, which makes it impossible to quantify the contribution of ALA to the observed lower risk of CHD. Two other secondary prevention trials have reported on the effects of ALA supplements (18) and an ALA-enriched “Indo-Mediterranean diet” (19) on the risk of CHD. However, the reliability of results reported by this research group have been seriously questioned (20), and can therefore not be taken as credible evidence for an effect of ALA on CHD. More recently, the Alpha-Omega Trial showed no statistically significant effect of a low dose of 1.9 g/d ALA provided during 40 months on major cardiovascular events, including death from CHD in patients who had myocardial infarction. However, a borderline significant lower rate of cardiovascular events on ALA treatment was observed Page 2 of 7 Optimal intakes of alpha-linolenic acid for heart health (2011) in female patients (21). The authors indicate that the drug therapy used by the patients in their trial may have obscured possible beneficial effects of ALA. A meta-analysis (22) of five prospective cohort studies observed an inverse association between the intake of ALA and risk of CHD in most (23-26) but not all studies (27). The meta-analysis showed that a high ALA intake compared to a low ALA intake was associated with a lower borderline statistically significant risk of CHD mortality (RR=0.79, 95% CI 0.60, 1.04). Another prospective study (nested case-control in the Cardiovascular Heath study) observed significantly lower fatal ischemic heart disease with higher ALA concentrations (28). Updated analyses from the Health Professional FollowUp study (14 years follow-up) and the Nurses’ Health Study (18 years follow-up) confirmed the significant reductions in risk of CHD with increased ALA intakes (29;30) that were earlier reported (24;26). Two case-control studies suggest that ALA intake is associated with a lower risk of CHD (31;32); while one study observed an increased CHD risk with higher ALA intake (33). A large crosssectional study in men and women observed a significantly lower prevalence of CHD with higher intakes of ALA (34). A review on ALA and clinical cardiovascular outcomes concluded that, there is evidence from only one observational study that supports a protective effect against nonfatal myocardial infarction. However, no significant protective associations were observed between ALA status and risk of heart failure, atrial fibrillation, and sudden death (35). Moreover, in a large cohort study, ALA intake was also not associated with risk of CHD events (36). Although benefits have not been observed consistently and the number of high quality clinical and prospective cohort studies is small, the available evidence supports that higher ALA intakes may reduce the risk of CHD. ALA may affect several cardiovascular risk markers and cardiovascular end points Specific biological mechanisms by which ALA could reduce CVD risk are still largely unknown and needs to be addressed in further studies. The conversion of ALA to LCPUFA has been suggested as a way via which ALA could confer heart health benefits (37;38). However, as discussed above, the conversion of ALA to LCPUFA is limited and it is well possible that ALA has favorable cardiovascular effects by itself. Beneficial effects on multiple cardiovascular risk markers including cholesterol, blood pressure, glucose, inflammation, thrombosis, and arrhythmias have been reported (39-42). A review concluded that ALA intake did not significantly modify several cardiovascular risk factors (including total cholesterol, triglycerides, weight, body mass index, LDL, diastolic blood pressure, systolic blood pressure, VLDL, and apolipoprotein B) (43). A review of studies on ALA intake and CVD published between 2008 and 2010 showed that the evidence for protective effects of ALA is inconsistent for CVD risk markers, including blood lipids, low-density lipoprotein oxidation, lipoprotein(a), and apolipoproteins A-I and B (35). Conflicting results were found for studies of ALA in relation to inflammatory markers and glucose metabolism in the same review (35). Furthermore, it has been reported that low ALA intake may increase the risk of incident stroke in western countries (36;44), but results were not confirmed in a study in Japan (45). In summary, evidence is currently inconclusive for a beneficial role of ALA on cardiovascular end points other than CHD and biologic mechanisms of possible beneficial effects are unclear. The effect of ALA on blood lipids and lipoproteins is about similar to that of LA The potential beneficial effects of ALA on the risk of CHD can only for a small part be explained by its effect on blood lipids. While total vegetable PUFA have a favourable effect on the blood lipoprotein profile (46); the evidence is much more established for LA than ALA, mainly because the majority of total PUFA in the diet consists of LA. Very few studies have examined the specific effect of ALA on blood lipids. When ALA is examined by comparing the effects of exchanging oils (e.g. exchanging linseed oil and sunflower seed oil to compare directly with LA), generally no differences in effect on cholesterol and triglyceride levels have been observed (47-52). This suggests that ALA has an almost similar beneficial effect on the blood lipoprotein profile as LA. Because ALA is only a minor part of total PUFA (ALA+LA) in the diet, the potential impact on blood lipids would be small. Furthermore, ALA does not share the powerful triglyceride lowering effects of EPA+DHA (48;53;54). Assuming ALA is as effective as LA (the major unsaturated fatty acid in the diet), the predicted effects on blood Page 3 of 7 Optimal intakes of alpha-linolenic acid for heart health (2011) lipids of ALA in amounts as recommended or studied are too small to explain a relation between higher ALA intakes and lower risk of CHD. Conclusions For optimal heart health, a total omega-3 fatty acid intake of up to 2 en% is recommended, of which at least 1 en% should be ALA and at least 250 mg should be EPA+DHA Available evidence supports a beneficial effect of ALA on heart health, although this evidence is less strong and extensive than for marine omega-3 fatty acids Replacing dietary SAFA with PUFA (in practice mainly LA plus some ALA) lowers CHD risk The omega-3 to omega-6 ratio is not a useful concept The effect of ALA is small compared to LA because ALA makes up only a minor part of total vegetable PUFA in the diet Although ALA contributes to maintenance of LDL cholesterol concentrations, this effect is too small to explain the inverse relation between ALA intake and CHD The mechanisms by which ALA can contribute to heart health are not clear There is not enough evidence to assess if the contribution of dietary ALA to heart health is a direct effect of ALA or a indirect effect, via (limited) conversion in the body to EPA+DHA References 1. Mozaffarian D, Micha R, Wallace S. Effects on coronary heart disease of increasing polyunsaturated fat in place of saturated fat: a systematic review and meta-analysis of randomized controlled trials. PLoS Med 2010;7:e1000252. 2. FAO. Fats and fatty acids in human nutrition. Report of an expert consultation. 2010. Rome, FAO. 3. Astrup A, Dyerberg J, Elwood P et al. The role of reducing intakes of saturated fat in the prevention of cardiovascular disease: where does the evidence stand in 2010? Am J Clin Nutr 2011;93:684-8. 4. Kromhout D, Geleijnse JM, Menotti A, Jacobs DR. The confusion about dietary fatty acids recommendations for CHD prevention. Br J Nutr 2011;doi:10.1017/S0007114511002236. 5. Ramsden CE, Hibbeln JR, Majchrzak SF, Davis JM. n-6 fatty acid-specific and mixed polyunsaturate dietary interventions have different effects on CHD risk: a meta-analysis of randomised controlled trials. Br J Nutr 2010;104:1586-600. 6. Harris WS, Mozaffarian D, Rimm E et al. Omega-6 fatty acids and risk for cardiovascular disease: a science advisory from the American Heart Association Nutrition Subcommittee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Cardiovascular Nursing; and Council on Epidemiology and Prevention. Circulation 2009;119:902-7. 7. EFSA. Scientific Opinion on the substantiation of a health claim related to "low fat and low trans spreadable fat rich in unsaturated and omega-3 fatty acids" and reduction of LDL-cholesterol concentrations pursuant to Article 14 of Regulation (EC) No 1924/2006. EFSA Journal 2011;9:2168-81. 8. Burdge G. Alpha-linolenic acid metabolism in men and women: nutritional and biological implications. Curr Opin Clin Nutr Metab Care 2004;7:137-44. Page 4 of 7 Optimal intakes of alpha-linolenic acid for heart health (2011) 9. Burdge GC. Metabolism of alpha-linolenic acid in humans. Prostaglandins Leukot Essent Fatty Acids 2006;75:161-8. 10. Goyens PL, Spilker ME, Zock PL, Katan MB, Mensink RP. Conversion of alpha-linolenic acid in humans is influenced by the absolute amounts of alpha-linolenic acid and linoleic acid in the diet and not by their ratio. Am J Clin Nutr 2006;84:44-53. 11. Brenna JT. Efficiency of conversion of alpha-linolenic acid to long chain n-3 fatty acids in man. Curr Opin Clin Nutr Metab Care 2002;5:127-32. 12. Wang C, Harris WS, Chung M et al. n-3 Fatty acids from fish or fish-oil supplements, but not alpha-linolenic acid, benefit cardiovascular disease outcomes in primary- and secondaryprevention studies: a systematic review. Am J Clin Nutr 2006;84:5-17. 13. Brouwer IA. Omega-3 PUFA: Good or bad for prostate cancer? Prostaglandins Leukot Essent Fatty Acids 2008. 14. Simon JA, Chen YH, Bent S. The relation of alpha-linolenic acid to the risk of prostate cancer: a systematic review and meta-analysis. Am J Clin Nutr 2009;89:1558S-64S. 15. Natvig H, Borchgrevink CF, Dedichen J, Owren PA, Schiotz EH, Westlund K. A controlled trial of the effect of linolenic acid on incidence of coronary heart disease. The Norwegian vegetable oil experiment of 1965-66. Scand J Clin Lab Invest Suppl 1968;105:1-20. 16. de Lorgeril M, Renaud S, Mamelle N et al. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 1994;343:1454-9. 17. de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation 1999;99:779-85. 18. Singh RB, Niaz MA, Sharma JP, Kumar R, Rastogi V, Moshiri M. Randomized, double-blind, placebo-controlled trial of fish oil and mustard oil in patients with suspected acute myocardial infarction: the Indian experiment of infarct survival--4. Cardiovasc Drugs Ther 1997;11:485-91. 19. Singh RB, Dubnov G, Niaz MA et al. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet 2002;360:1455-61. 20. White C. Suspected research fraud: difficulties of getting at the truth. BMJ 2005;331:281-8. 21. Kromhout D, Giltay EJ, Geleijnse JM. n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med 2010;363:2015-26. 22. Brouwer IA, Katan MB, Zock PL. Dietary alpha-linolenic acid is associated with reduced risk of fatal coronary heart disease, but increased prostate cancer risk: a meta-analysis. J Nutr 2004;134:919-22. 23. Dolecek TA. Epidemiological evidence of relationships between dietary polyunsaturated fatty acids and mortality in the multiple risk factor intervention trial. Proc Soc Exp Biol Med 1992;200:177-82. 24. Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ 1996;313:84-90. Page 5 of 7 Optimal intakes of alpha-linolenic acid for heart health (2011) 25. Pietinen P, Ascherio A, Korhonen P et al. Intake of fatty acids and risk of coronary heart disease in a cohort of Finnish men. The Alpha-Tocopherol, Beta-Carotene Cancer Prevention Study. Am J Epidemiol 1997;145:876-87. 26. Hu FB, Stampfer MJ, Manson JE et al. Dietary intake of alpha-linolenic acid and risk of fatal ischemic heart disease among women. Am J Clin Nutr 1999;69:890-7. 27. Oomen CM, Ocke MC, Feskens EJ, Kok FJ, Kromhout D. alpha-Linolenic acid intake is not beneficially associated with 10-y risk of coronary artery disease incidence: the Zutphen Elderly Study. Am J Clin Nutr 2001;74:457-63. 28. Lemaitre RN, King IB, Mozaffarian D, Kuller LH, Tracy RP, Siscovick DS. n-3 Polyunsaturated fatty acids, fatal ischemic heart disease, and nonfatal myocardial infarction in older adults: the Cardiovascular Health Study. Am J Clin Nutr 2003;77:319-25. 29. Mozaffarian D, Ascherio A, Hu FB et al. Interplay between different polyunsaturated fatty acids and risk of coronary heart disease in men. Circulation 2005;111:157-64. 30. Albert CM, Oh K, Whang W et al. Dietary alpha-linolenic acid intake and risk of sudden cardiac death and coronary heart disease. Circulation 2005;112:3232-8. 31. Campos H, Baylin A, Willett WC. Alpha-linolenic acid and risk of nonfatal acute myocardial infarction. Circulation 2008;118:339-45. 32. Guallar E, Aro A, Jimenez FJ et al. Omega-3 fatty acids in adipose tissue and risk of myocardial infarction: the EURAMIC study. Arterioscler Thromb Vasc Biol 1999;19:1111-8. 33. Pedersen JI, Ringstad J, Almendingen K, Haugen TS, Stensvold I, Thelle DS. Adipose tissue fatty acids and risk of myocardial infarction--a case-control study. Eur J Clin Nutr 2000;54:61825. 34. Djousse L, Pankow JS, Eckfeldt JH et al. Relation between dietary linolenic acid and coronary artery disease in the National Heart, Lung, and Blood Institute Family Heart Study. Am J Clin Nutr 2001;74:612-9. 35. Geleijnse JM, de GJ, Brouwer IA. Alpha-linolenic acid: is it essential to cardiovascular health? Curr Atheroscler Rep 2010;12:359-67. 36. de GJ, Verschuren WM, Boer JM, Kromhout D, Geleijnse JM. Alpha-linolenic acid intake and 10-year incidence of coronary heart disease and stroke in 20,000 middle-aged men and women in the Netherlands. PLoS One 2011;6:e17967. 37. Barcelo-Coblijn G, Murphy EJ, Othman R, Moghadasian MH, Kashour T, Friel JK. Flaxseed oil and fish-oil capsule consumption alters human red blood cell n-3 fatty acid composition: a multiple-dosing trial comparing 2 sources of n-3 fatty acid. Am J Clin Nutr 2008;88:801-9. 38. Harper CR, Edwards MJ, DeFilippis AP, Jacobson TA. Flaxseed oil increases the plasma concentrations of cardioprotective (n-3) fatty acids in humans. J Nutr 2006;136:83-7. 39. Stark AH, Crawford MA, Reifen R. Update on alpha-linolenic acid. Nutr Rev 2008;66:326-32. 40. Harris WS. Alpha-linolenic acid: a gift from the land? Circulation 2005;111:2872-4. 41. Mozaffarian D. Does alpha-linolenic acid intake reduce the risk of coronary heart disease? A review of the evidence. Altern Ther Health Med 2005;11:24-30. Page 6 of 7 Optimal intakes of alpha-linolenic acid for heart health (2011) 42. de Deckere EA, Korver O, Verschuren PM, Katan MB. Health aspects of fish and n-3 polyunsaturated fatty acids from plant and marine origin. Eur J Clin Nutr 1998;52:749-53. 43. Wendland E, Farmer A, Glasziou P, Neil A. Effect of alpha linolenic acid on cardiovascular risk markers: a systematic review. Heart 2006;92:166-9. 44. Simon JA, Fong J, Bernert JT, Jr., Browner WS. Serum fatty acids and the risk of stroke. Stroke 1995;26:778-82. 45. Iso H, Sato S, Umemura U et al. Linoleic acid, other fatty acids, and the risk of stroke. Stroke 2002;33:2086-93. 46. Mensink RP, Zock PL, Kester AD, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a metaanalysis of 60 controlled trials. Am J Clin Nutr 2003;77:1146-55. 47. Bemelmans WJ, Broer J, Feskens EJ et al. Effect of an increased intake of alpha-linolenic acid and group nutritional education on cardiovascular risk factors: the Mediterranean Alpha-linolenic Enriched Groningen Dietary Intervention (MARGARIN) study. Am J Clin Nutr 2002;75:221-7. 48. Harris WS. n-3 fatty acids and serum lipoproteins: human studies. Am J Clin Nutr 1997;65:1645S-54S. 49. Nydahl M, Gustafsson IB, Ohrvall M, Vessby B. Similar serum lipoprotein cholesterol concentrations in healthy subjects on diets enriched with rapeseed and with sunflower oil. Eur J Clin Nutr 1994;48:128-37. 50. Lichtenstein AH, Ausman LM, Carrasco W et al. Effects of canola, corn, and olive oils on fasting and postprandial plasma lipoproteins in humans as part of a National Cholesterol Education Program Step 2 diet. Arterioscler Thromb 1993;13:1533-42. 51. Seppanen-Laakso T, Vanhanen H, Laakso I, Kohtamaki H, Viikari J. Replacement of margarine on bread by rapeseed and olive oils: effects on plasma fatty acid composition and serum cholesterol. Ann Nutr Metab 1993;37:161-74. 52. Chan JK, Bruce VM, McDonald BE. Dietary alpha-linolenic acid is as effective as oleic acid and linoleic acid in lowering blood cholesterol in normolipidemic men. Am J Clin Nutr 1991;53:12304. 53. Goyens PL, Mensink RP. Effects of alpha-linolenic acid versus those of EPA/DHA on cardiovascular risk markers in healthy elderly subjects. Eur J Clin Nutr 2006;60:978-84. 54. Layne KS, Goh YK, Jumpsen JA, Ryan EA, Chow P, Clandinin MT. Normal subjects consuming physiological levels of 18:3(n-3) and 20:5(n-3) from flaxseed or fish oils have characteristic differences in plasma lipid and lipoprotein fatty acid levels. J Nutr 1996;126:2130-40. Page 7 of 7