Public Health - California Directors of Public Health Nursing

1
PUBLIC HEALTH:
IMPROVING HEALTH FOR
ALL DISCUSSION SERIES
An overview of an innovative workforce development training
Aaron T. Gardner, MA
Wendy Hetherington, MPH
Directors of Public Health Nursing in California
2015 Fall Conference
San Diego, California
Learning Objectives
Participants will be able to:
Describe the key components of the Riverside County
Department of Public Health’s health equity staff training program.
Design a health equity and social justice training series, adapted to meet the needs of your organization.
Identify important logistical items to address successful training implementation.
Identify two ways to evaluate a staff-driven training series
Riverside County: Who We Are
2.2 Million residents
Population expected to increase by 1 million over the next decade
55% of residents identify as non-white
Home to Palm Springs,
California
San Francisco
Riverside County
Los
Angeles
San Diego
County of Riverside Department of Public Health
Health Equity Committee
5
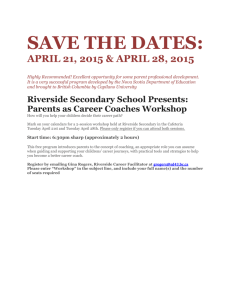
Improving Health for All Discussion Series
• Shift the Currents of
Departmental Culture
• All staff on the same page
• Why reinvent the wheel?
The Intervention:
Improving Health for All (IHA)
• A six-module discussion series designed to build a public health workforce that is able to address health disparities and inequities
• Each module is 4-hours in length
• Department requirement
6
Improving Health for All facilitators, Riverside County
Department of Public Health, December 2012
7
Public Health 101
Alameda County, CA
Module I
An Overview of Public Health
Module II
Cultural Competency &
Cultural Humility
Module III
Undoing Racism
Module IV
Social and Health Equity
Module V
Community Capacity Building
Riverside County, CA
Module I
• An Overview of Public Health
Module II
Cultural Competency &
Acceptance
Module III
• Deconstructing Racism
Module IV
• Social Determinants of Health
Module V
• Discrimination & Stigma
Module VI
• Community Engagement &
Capacity Building
Alameda County Department of Public Health (2013). PH 101 Dialogue Series. Social and Health Equity. http://www.acphd.org/social-and-health-equity/organizational-transformation/trainings-and-dialogues/ph101.aspx
Public Health: Improving Health for All
Module I
•
• Public Health History & System
Core Functions and of Public Health
Essential Services
Module II
• Cultural Competency & Acceptance
Module III
• Deconstructing Racism
Module IV
• Social Determinants of Health
Module V
• Discrimination & Stigma
Module VI
• Community Engagement &
Building
Capacity
8
9
Module 1: Overview of Public Health
Public health history and connections to social justice
3 main organizational levels of the public health system
3 core functions and 10 essential services of public health and linked it to what we do each day
Module 2: Cultural Competency &
Acceptance
Difference between health inequities and health disparities
Importance of cultural competency and cultural acceptance
Application of lessons learned from this training to improve services provided to our community
10
Module 3: Deconstructing Racism
11
Social, economic, and political conditions that disproportionately privilege some groups while disadvantaging others
How institutional racism impacts Riverside
County residents
Ideas for addressing institutional racism and its impact
12
Module 4: Social Determinants of Health
• Describe and identify social determinants of health and how they lead to social and health inequities.
• Learn how DOPH is addressing social determinants of health.
13
Module 5: Discrimination & Stigma
The discussion focuses on three groups : o LGBT o Aging o People with Disabilities
• To recognize and address the perceived discrimination and stigma among these three groups.
• Discuss ways we can avoid and undo discrimination among the groups discussed.
Module 6: Community Engagement &
Capacity Building
Discussion on:
14
The Department’s role in community engagement and capacity building
Discuss the benefits and challenges of community engagement and capacity building
Describe DOPH efforts to improve
CE and CCB.
Articulate their role in CE and
CCB
How to Begin
Getting department buy-in
How did DOPH do this?
Educating and motivating
Lots of meetings
Use data to illustrate the need
How to Begin
Getting department buy-in, continued
Frequent communication
Enlist support
Get the information out…spread the word
How to Begin
Recommendations:
Involve the chief
Susan Harrington, MS, RD
Director, Public Health
Chief administrators need an active role in goal setting, prioritizing, and launching of this effort
Additionally…
Diverse development teams
Constant communication with a feedback loop
Adapting the PH 101 Dialogue Series
Form a curriculum development team
A diverse group
Need to spread the work
Adapting the PH 101 Dialogue Series
Develop a vision
Consult with the experts
Other jurisdictions, EAS, etc.
Training coordination
Know your staff
Awareness Survey Response Comparison
Self-reported: “No knowledge of the topic”.
Relationship between
Institutional Racism and Health
Inequities
Definition and Measurement of
Health
Social Determinants of Health
Community Capacity Building
How Community Capacity
Building Supplements
Traditional Program & Service
Delivery
County of Riverside
DOPH
19.1%
18.4%
17.0%
36.8%
39.3%
Alameda County
PHD
11.8%
11.8%
9.9%
17.5%
20.3%
Adapting a PH 101 Dialogue Series
Recommendations:
Have a development team
Assess and alert your staff
Create deadlines
Allow evolution
Training and Recruitment of Facilitators
Who are the facilitators?
Optimal pairing
Support from Public
Health Director
Have staff development team
Training and Recruitment of Facilitators
Employee Assistance
Services
Rehearse
Facilitators’ Meetings
Alameda County (ACDPH)
Site Visit
Dr. Jamie Rotnofsky, PhD
Director, Employee Assistance Services
Training and Recruitment
Recommendations:
Administrator Recognition
Have a Staff Development
Team
Mandatory Rehearsals
Implementation and Logistics
Training is mandatory
Diverse facilitation
Use Dry-runs and pilots
Implementation and Logistics
Plan for challenges
Constant feedback
Use the skills of a PIO
Developing a toolkit
Jose Arballo
Public Information Specialist
Implementation and Logistics
Recommendations:
Mandate training participation
Have diverse facilitation teams
Use rehearsals
Have a staff development team…ring a bell?
Sakeena Al-Amin
Staff Development Team Member
How Ready Are You?
What’s your organization’s need?
Is your organization ready for a change in culture?
Time, resources, and personnel…do you have enough?
Can your organization sustain the effort?
Let’s take a minute to assess your organization’s readiness!
Evaluation
Be sure to develop an evaluation plan
Don’t back into evaluation
A must have in order to determine your program’s effectiveness
Can help you figure out what is or is not working
Can be an integral part of your planning
Designating
Evaluation
Plans
Designing
Data
Collection
Tools
Collecting
Data
Analyzing
Results
Reporting
Findings
Planning
Program
Changes
Evaluation
Process evaluation
“Hot Wash”
Feedback
Participant census
Outcome evaluation
Knowledge, self-efficacy, attitudinal, and behavioral intentions scale
Impact evaluation
Long-term and may be hard to measure
Organizational assessment
31
Evaluation
• Two levels of evaluation
• Class level
• Outcome Evaluation – Improving Health for All
Research Study
32
The Improving Health for All
Research Study
• To examine the effects of the Improving Health for
All program on staff of County of Riverside’s
Department of Public Health
• Received IRB Approval on March 27, 2013
• Study period: April 22, 2013 - Sept. 26, 2013
Penny, M., Modeste, N., Herring, P., Marshak, H., & Gardner, A. (2014). Examining the role of knowledge and perceptions in predicting the intention to address health disparities among public health staff. Manuscript submitted for publication.
Penny, M., Modeste, N., Herring, P., Marshak, H., & Gardner, A. (2014). Effects of Public Health Workforce
Development on Knowledge, Perceptions and Intention to Develop Strategies to Reduce Health Disparities.
Manuscript submitted for publication.
33
Theoretical Framework
Attitude towards behavior
Improving
Health for all
Intervention
Knowledge
Subjective Norm to perform behavior
Behavioral
Intention
Perceived
Behavioral
Control to engage in behavior
The hypothesized relationships using the theory of planned behavior
(TPB) to illustrate the influence of knowledge, attitude, subjective norm, and perceived behavioral control on behavioral intention.
34
Study Research Questions
1.
Are there differences in knowledge , attitudes , subjective norm , perceived behavioral control , and behavioral intention to address health disparities and inequities after participating in the intervention, compared to perceptions of those variables prior to the intervention?
2.
After controlling for pretest values, are there differences in posttest knowledge and TPB variables among those who have formal public health training (FPHT) compared to those who do not have formal public health training
(FPHT)?
3.
After controlling for pretest values, do staff posttest reports of knowledge , and TPB variables predict their posttest reports of behavioral intention ?
35
Results - Effect of IHA Intervention
• Results indicate a positive effect of IHA on knowledge and perceptions as they relate to issues of health disparities
• Knowledge and all TPB variable scores were statistically significantly higher at posttest compared to retrospective pretest.
• Posttest knowledge and PBC scores were statistically significantly higher among those with FPHT compared to those without.
•
Pretest scores of attitude and Posttest scores of attitude , PBC , and SN were significant predictors of behavioral intention
[R 2 =.66, F(17, 138) = 16.018, p<.001].
36
Why has this been so successful?
• Time!
• Priority
• Listening to all members and facilitators
• Must have successes: How are these defined?
Evaluation Recommendation
Do one!
Start it early
Be sure to have a clear program goal and objectives
Keep records
Meeting agendas and minutes
Old versions of material
Focus group notes
Biggest Challenges and Successes
Challenges
Administrative changes
Fear of the unknown
Logistics
Maintaining a facilitator pool
Communication
Successes
Supportive administrators
High level of interest
Staff Development
Strong facilitator support and dedication
Work in progress
39
Summary/Q&A
• What are your thoughts?
• What are your suggestions?
• Any questions?
Improving Health for All facilitators, Riverside County Department of Public Health,
June 2013