Glaucoma and Ocular Surface Disease
advertisement

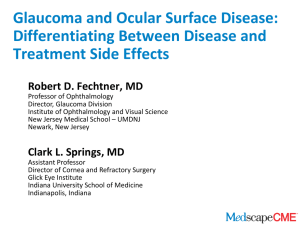
Glaucoma and Ocular Surface Disease: Differentiating Between Disease and Treatment Side Effects Robert D. Fechtner, MD Professor of Ophthalmology Director, Glaucoma Division Institute of Ophthalmology and Visual Science New Jersey Medical School – UMDNJ Newark, New Jersey Clark L. Springs, MD Assistant Professor Director of Cornea and Refractory Surgery Glick Eye Institute Indiana University School of Medicine Indianapolis, Indiana Overall Program Goal The goal of the program is to examine the incidence of and issues involved in accurately identifying and managing ocular surface disease in patients who have glaucoma. Prevalence of Dry Eye and Ocular Surface Disease Study results showing prevalence of dry eye (overall, in women, in men, and in older individuals): • Schaumberg DA, et al. Am J Ophthalmol. 2003;136:318-326. • Schaumberg DA, et al. Arch Ophthalmol. 2009;127:763-768. • Schein OD, et al. Am J Ophthalmol. 1997:124:723-728. Prevalence of Dry Eye Among Women: Study Population • 39,876 health professionals • Ages 45-84 years • Enrolled in the Women’s Health Study, a randomized trial designed to assess the benefits of and risks for aspirin and vitamin E in the primary prevention of cardiovascular disease and cancer in healthy women • Participants received mailed questionnaires every year • At year 4, included 3 questions about dry eye Schaumberg DA, et al. Am J Ophthalmol. 2003;136:318-326. Prevalence of Dry Eye Among Women: Methods • Have you ever been diagnosed by a clinician as having dry eye syndrome? • How often do your eyes feel dry (not wet enough)? • How often do your eyes feel irritated? • Possible answers: – – – – constantly often sometimes never Schaumberg DA, et al. Am J Ophthalmol. 2003;136:318-326. Prevalence of Dry Eye Among Women: Results • The prevalence of dry eye syndrome increased with age, from 5.7% among women < 50 years old to 9.8% among women aged ≥ 75 years old. The age-adjusted prevalence of dry eye syndrome was 7.8%, or 3.23 million women aged ≥ 50 in the United States. • Compared with whites, Hispanic (OR 1.81, CI 1.182.80) and Asian (OR 1.77, CI 1.17-2.69) women were more likely to report severe symptoms, but not be clinically diagnosed with dry eye syndrome. • Women from the South had the highest prevalence of dry eye syndrome, although the magnitude of geographic differences was modest. Schaumberg DA, et al. Am J Ophthalmol. 2003;136:318-326. Prevalence of Dry Eye Among Women 9.8% among women aged ≥ 75 years old Schaumberg DA, et al. Am J Ophthalmol. 2003;136:318-326. Prevalence of Dry Eye Among Men: Study Population • Physicians Health Study (PHS) • Randomized period of PHS I and PHS II ended in 1999 • 25,444 men, including 18,596 original participants in PHS I and 6848 men who did not participate in PHS I but were randomly assigned to PHS II Schaumberg DA, et al. Arch Ophthalmol. 2009;127:763-768. Prevalence of Dry Eye Among Men: Methods • Have you ever been diagnosed by a clinician as having dry eye syndrome? • How often do your eyes feel dry (not wet enough)? • How often do your eyes feel irritated? • Possible answers: – – – – constantly often sometimes never Schaumberg DA, et al. Arch Ophthalmol. 2009;127:763-768. Prevalence of Dry Eye Among Men: Results • The prevalence of dry eye disease increased with age, from 3.90% among men aged 50-54 years to 7.67% among men 80 years and older (P for trend ≤ .001). • High blood pressure and benign prostatic hyperplasia were associated with a higher risk for dry eye disease. • Use of antidepressants, antihypertensives, and medications to treat benign prostatic hyperplasia were also associated with increased risk for dry eye disease. Schaumberg DA, et al. Arch Ophthalmol. 2009;127:763-768. Prevalence of Dry Eye Among Men 7.67% among men 80 years and older Schaumberg DA, et al. Arch Ophthalmol. 2009;127:763-768. Prevalence of Dry Eye Among the Elderly: Study Population • 2520 residents of Salisbury, Maryland • 65 years or older as of 1993 • Standardized questionnaire (6 questions) • Examination – Schirmer’s test – Rose Bengal stain – Assessment of meibomian glands Schein OD, et al. Am J Ophthalmol. 1997:124:723-728. Prevalence of Dry Eye Among the Elderly: Results Age Group (yr) Percent Who Have 1 or More Symptoms Often or All the Time 65-69 14.2% (774) 70-74 14.9% (824) 75-79 13.7% (540) 80+ 16.3% (344) Gender Male 13.3% (1052) Female 15.6% (1430) Schein OD, et al. Am J Ophthalmol. 1997:124:723-728. Prevalence of Dry Eye Among the Elderly: Results 14.6% reported 1 or more dry eye symptom “often” or “all the time” Schein OD, et al. Am J Ophthalmol. 1997:124:723-728. Interactive Poll Question Approximately what percentage of your patients treated for glaucoma would you estimate also have ocular surface disease symptoms? Fewer than 1% Approximately 15% Approximately 25% Approximately 50% More than half Prevalence of Ocular Surface Disease in Patients With Glaucoma Studies have sought to determine how common ocular surface disease (OSD) is in patients with glaucoma: • Leung EW, et al. J Glaucoma. 2008; 17:350-355. • Fechtner RD, et al. Cornea. 2010;29:618-621. Prevalence of OSD in Patients With Glaucoma: Study Design • 101 patients with glaucoma or ocular hypertension • Exclusions: receiving cyclosporine, steroids, topical ocular nonsteroidal anti-inflammatory drugs, or punctal plugs within previous 3 months • Testing – – – – Ocular Surface Disease Index (OSDI) Schirmer’s test Staining (fluorescein and lissamine green) Tear break-up time (TBUT) Leung EW, et al. J Glaucoma. 2008;17:350-355. Number (%) of Patients With Each Result Test Results Lissamine Green OSDI Schirmer’s Test TBUT Normal 79 41 39 22 Mild to Moderate 22 33 27 13 Severe 0 27 35 66 Leung EW, et al. J Glaucoma. 2008;17:350-355. Patients With Symptoms (%) Symptoms vs Signs of OSD Clinical Tests Leung EW, et al. J Glaucoma. 2008;17:350-355. Prevalence of OSD in Patients With Glaucoma: Results OSDI Scores in Glaucoma Patients Ranking Normal Mild to Moderate Patients 41 33 27 41% 33% 27% Percentage 59% Leung EW, et al. J Glaucoma. 2008;17:350-355. Severe Prevalence of OSD in Patients With Glaucoma Treated With Topical Medications: Study Methods • Conducted from May 2006 to March 2007 • 10 sites - geographically distributed • 630 glaucoma patients: – > 18 years of age – Primary open-angle, exfoliation, or pigment dispersion glaucoma, or ocular hypertension in both eyes – Treated with 1 or more topical intraocular pressurelowering medication(s) • Patients completed OSDI survey while in the office Fechtner RD, et al. Cornea. 2010;29:618-621. OSDI Severity Grading Normal Mild Moderate (0-12) (13-22) (23-32) 0 10 20 30 Severe (33-100) 40 50 60 70 80 Total OSDI Score = (Sum of Score for All Questions Answered) X (25) (Total # of Questions Answered) Miller KL, et al. 13th Annual Conference of the International Society for Quality of Life Research. 2006. Abstract 1540. 90 100 Prevalence of OSD in Patients With Glaucoma Treated With Topical Medications: Study Results OSDI Scores in Glaucoma Patients Ranking Normal Mild Moderate Severe Patients 325 134 84 87 51.6% 21.3% 13.3% 13.8% Percentage 48.4% Fechtner RD, et al. Cornea. 2010;29:618-621. Ocular Surface Disease and Topical Medications for Glaucoma Studies suggest there may be a relationship between the presence of OSD in patients with glaucoma and topical medications for glaucoma: • Leung EW, et al. J Glaucoma. 2008;17:350-355. • Rossi GC, et al. Eur J Ophthalmol. 2009;19:572-579. Patients (Percentage) OSDI and Number of BAK-Containing Eyedrops Number of BAK-Containing Eyedrops BAK = benzalkonium chloride Leung EW, et al. J Glaucoma. 2008;17:350-355. Dry Eye Syndrome–Related Quality of Life in Glaucoma Patients: Study Methods • 61 treated subjects (G1 = 1 drop/day, G2 = 2 drops/day, G3 = 3 drops/day) • 20 untreated controls (G0 = no drops) • Questionnaires – National Eye Institute Visual Function Questionnaire (NEI-VFQ) – Glaucoma Symptom Scale (GSS) – OSDI • Dry eye syndrome was defined as presence of punctate keratitis and decreased TBUT Rossi GC, et al. Eur J Ophthalmol. 2009;19:572-579. Quality of Life: Impact of Multiple Medications Number of Medications Percent With Dry Eye Syndrome 0 medications 5 1 medication 11 2 medications 39 3 medications 40 Rossi GC, et al. Eur J Ophthalmol. 2009;19:572-579. Discussion of Answers to Poll Question Case #1: A 55-Year-Old Man • 55-year-old psychiatrist Medical History • Panic attacks (started 1 month ago) Ocular History • Primary open-angle glaucoma (diagnosed 15 years ago) • Posterior chamber intraocular lens OU • Trabeculectomy OU • Presumed ocular histoplasmosis syndrome OU, with central macular scars OU OU = each eye Case #1: Medications Ocular Medications • Bimatoprost OU every evening Other Medications • Escitalopram (for panic attacks) Chief Complaint “I am uncomfortable driving and I have difficulty reading at work.” Case #1: Examination • BCVa 20/400 OD • OS vision decreased from 20/50 to 20/100 • IOP in mid-teens • Moderate rosacea with meibomian gland dysfunction • Severe central PEE • Normal Schirmer’s test • Has to wear SCL to make bioptics work • Torn SCL BCVa = best corrected visual acuity; OD = right eye; OS = left eye; IOP = intraocular pressure; PEE = punctate epithelial erosions; SCL = soft contact lens Interactive Poll Question How would you proceed in this patient? Change to preservative-free artificial tears Decrease BAK load Anti-inflammatory therapy Punctal plugs All of the above Case #1: Treatment Plan • Reduce BAK Load – Travoprost BAK-free substituted for bimatoprost[a-c] • Anti-inflammatory therapy – Loteprednol etabonate[d] – 4 times a day for 1 week, thrice daily for 1 week, twice daily for 1 week, once daily for 1 week – Cyclosporine OU twice daily[e] – Doxycycline 20 mg orally twice daily[f] a. Baudouin C, et al. Br J Ophthalmol. 1998;82:39-42. b. Pisella PJ, et al. Br J Ophthalmol. 2002;86:418-423. c. Jaenen N, et al. Eur J Ophthalmol. 2007;17:341-351. d. Pavesio CE, Decory HH. Br J Ophthalmol. 2008;92:455-459. e. Perry HD, et al. Cornea. 2006;25:171-175. f. Stone DU, Chodosh J. Cornea. 2004;23:106-109. Case #1: Follow-up • 4-week follow-up: BCVa improved to 20/60 left eye • 1-year follow-up: BCVa improved to baseline Discussion of Answers to Poll Question Discussion: Approach to Patient Case #2: An 86-Year-Old Man • 86-year-old white man • Medical history – Hypertension – Cerebrovascular disease – Heart disease • Ocular history – Primary open-angle glaucoma since 1998 – Cataract extraction with intraocular lens OU 2000 – Branch retinal vein occlusion (BRVO) OD with poor vision 2002 – Steroid responder • Family history: sisters with glaucoma Case #2: Medications • Medications: verapamil, lisinopril, propafenone, simvastatin, dronedarone , aspirin • Ocular medications: bimatoprost at bedtime OU, brimonidine/timolol twice daily OU, cyclosporine ophthalmic twice daily OU, methazolamide 50 mg thrice daily, artificial tears as needed • Allergies: “All glaucoma drops” Chief Complaint “When I use my glaucoma medications and my IOP is controlled, my vision is poor. When I stop my drops, I see much better but my IOP is in the 30s.” Case #2. Ocular Examination • Visual acuity: distance OD 20/150, (+0.50-4.00 X 005), OS 20/50 (+1.0-3.50 X 90) ph 20/30-2 • External examination – – – – – Lids: erythema and meibomian gland dysfunction Conjunctiva: 2+ injection OU Cornea: punctate staining Anterior chamber: quiet Lens: IOL • Extraocular movement: unremarkable • Pupils: afferent defect OD Case #2. Slit Lamp Examination • Lids: meibomian gland dysfunction • Conjunctiva: 2+ injection • Cornea: punctate staining OU • Anterior chamber: OU, deep, quiet • Iris: OU normal • IOP: OD, 14 mm Hg, OS 19 mm Hg • Pachymetry: 560 OD, 552 OS • Gonioscopy: OU, open, ciliary body showing (d-40-q) Interactive Poll Question What are possible contributors to the external signs and symptoms? Drug allergy Drug toxicity Dry eye Meibomian gland disease Preservative toxicity Case #2. Dilated Examination and Diagnostic Testing • Lens: OU, IOL • Disc: OD, CDR 0.9 OS, CDR 0.5- (V&H) • Retina: OD old BRVO Visual Field: HVF 24-2 Discussion of Answers to Poll Question Case #2: Treatment Plan • Reduce BAK load[a-c] – Discontinue bimatoprost and brimonidine/timolol – Begin travoprost with sofZia™ preservative and preservative-free timolol – Continue methazolamide • Treat meibomian gland disease and ocular surface – Lid hygiene – Add azithromycin ophthalmic[d] – Continue cyclosporine ophthalmic a. Baudouin C, et al. Br J Ophthalmol. 1998;82:39-42. b. Pisella PJ, et al. Br J Ophthalmol. 2002;86:418-423. c. Jaenen N, et al. Eur J Ophthalmol. 2007;17:341-9.15. d. Luchs J. Adv Ther. 2008;25:858-870. Case #2: Follow-up • Two weeks later, by telephone call: “I feel a little better” • One week after that: – – – – Seen by comprehensive ophthalmologist Felt fine, felt vision was better IOP 30s OU Treated with brimonidine and brimonidine/timolol in the office – Placed on brimonidine 0.15% with Polyquad® Medications • Travoprost OU at bedtime • Preservative-free timolol OU twice daily • Brimonidine 0.15% OU thrice daily • Azithromycin ophthalmic OU twice daily • Cyclosporine ophthalmic OU twice daily • Methazolamide 50 mg orally thrice daily Case #2: Follow-up Examination • Visual acuity 20/150 OD, 20/50 OS • Lids and eyes red • Conjunctiva 2+ injection with follicles • Cornea mild punctate staining Case #2: Suspected Brimonidine Allergy • Discontinue brimonidine, cyclosporine ophthalmic, azithromycin ophthalmic • Continue travoprost, preservative-free timolol, methazolamide • Add pilocarpine 1% thrice daily OU, olopatadine once daily OU, doxycyline 20 mg orally once daily Blondeau P, Rousseau JA. Can J Ophthalmol. 2002;37:21-26. Case #2: Follow-up • Three weeks later, by telephone call with ophthalmologist: – – – – Seen by comprehensive ophthalmologist IOP in mid teens OU Eyes comfortable, felt vision was better Continue travoprost, preservative-free timolol, methazolamide, pilocarpine 1% thrice-daily OU, olopatadine once-daily OU, doxycyline 20 mg orally once daily Discussion: Approach to Patient Question-and-Answer Session With the Audience Thank you for participating in this activity. To proceed to the online CME test, click on the Earn CME Credit link on this page.