Providing Trans-Specific Health
Care to Transgender Students in
the College Health Setting
Michelle Famula MD, UC Davis
Nick Gorton MD, Lyon-Martin Health Services
Alexandra Hall MD, Cornell
Seth Pardo MA, Cornell
Overview
Brief discussion of gender identity
Discussion of Transsexuality
Explain the WPATH Standards of Care, and how
they can be used to provide needed care
Discuss the provision of hormonal and other
therapies, as well as primary care
Identify resources and strategies for providing
and maintaining quality care for transgender
students on our campuses
Defining the need…A Vignette
Rick, 21 yo undergraduate
Presented to CAPS for counseling and
medication in Summer ’05
Struggled with gender dysphoria, felt he was a
male born into a female body
Saw CAPS regularly for a year, decided that the
appropriate thing for him was to transition
Also saw a community therapist with experience
in gender dysphoria, who wrote a letter
affirming his readiness for hormonal therapy
Diagram of Sex and Gender
Biological Sex (anatomy, chromosomes, hormones)
male
intersex
female
Gender Identity (Sense of Self)
man
Twospirit/third gender
woman
Gender Expression (Communication of Gender)
masculine
androgynous
feminine
Sexual Orientation (Erotic Response)
attracted to women
Bisexual/asexual/pansexual
attracted to men
Biological Sex
anatomy, chromosomes, hormones
Biological Sex
anatomy, chromosomes, hormones
Fetal genital differentiation
Spectrum in-between
18% of all “congenital anomalies” are differences in genito-urinary tract.
1 in 100 live births are individuals who are not strictly “normal” male or
female, and 1 in 1000 will undergo some type of genital surgery.
Gender Identity
Internal sense of self,
may or may not be expressed
Only the individual can say for
themselves, cannot be “measured”
Gender Expression
Sexual Orientation / Attraction
Diagram of Sex and Gender
Biological Sex (anatomy, chromosomes, hormones)
male
intersex
female
Gender Identity (Sense of Self)
man
Twospirit/third gender
woman
Gender Expression (Communication of Gender)
masculine
androgynous
feminine
Sexual Orientation (Erotic Response)
attracted to women
Bisexual/asexual/pansexual
attracted to men
“Trans” or Transgender
An umbrella term / a spectrum
Other terms: Gender Non-Conforming, Gender-Queer
Gender identity and/or gender expression differ from
the conventional gender expectations for biological
males and females
OR
A gender identity not adequately defined by
conventional ideas of male and female.
NOTE: Sexual orientation is not in any way a part of this description!
How do our trans students define
themselves? What is their
experience of gender?
When “She” graduates as “He”:
Trans identity development
and navigating sexual boundaries in college
Seth T. Pardo, M.A.
Department of Human Development
Cornell University
Ithaca, NY 14853
Study design
Questionnaire
Recruited individuals who were “gender non-conforming”
299 surveys: 204 were natal females: 170 respondents
Mean age 28.6 +/- 9.4
Asked open-ended, “in your own words, how do you describe…”
GLBT Centers
List-serves
Conferences and Meetings
Public Events
Your gender identity
Your daily behavior, dress style, and appearance
Asked partner preference (sexual orientation)
Asked “at what age, if any, did you first…”
Wish to have been born a boy
Pass as the other sex
Feel a need for surgery/hormones
Who is Transgender?
Conceptualizations & Expressions
Major Identity
Domain
Domain Description &
Sub-domains
Sub-Domains
Gender Identity
Sex- or gender-qualified self.
“female,” “woman,” “male,” “man,”
“fluid,” “both,” or “neither.”
Gender Role &
Presentation
Qualitative daily behavior, dress style,
appearance, and personality
terms that reflect traditionally gendered
"feminine," "masculine;" or new/other
terms like “fluid” or “gender queer”.
Sexual Orientation &
Partner Preference
The self-described erotic attractions or
partner preferences
“asexual,” “gay,” “bisexual,” “straight,”
“lesbian,” “pansexual,” “transgender,”
“males,” “men,” “females,” “women,”
“queer,” “little or no preference,” some
combo*, or new other.**
Transitional Status
The hormonal or surgical body
modifications planned or completed.
“pre-op” (i.e. pre-operation), “noho” (i.e.
no hormones), “top-surgery,” “bottom
surgery,” and “post-op”
Gender Identity
“Naming” Transgender
Gender Identity
Androgynist
Boi
Butch
Chameleon
Cross-Dresser or Transvestite
Diesel Dyke or Dyke
Drag King
Drag Queen
Fem
Impersonator
Fem Male or Sissy Male
Female
Female-to-male (FTM)
Gender Blender
Gender Fuck
Hermaphrodite or Intersex
Male
Queer or Gender Queer
Sex Radical
Tranny Boy
Transgender
Transsexual
I prefer no label
T otal Selections
N
23
33
19
6
8
23
13
2
11
2
17
28
88
21
30
6
73
150
10
49
41
55
19
727
(88% of all respondents)
That’s about 4
terms per person!
In your own words, how do you describe your
gender identity?
Range of Responses: More Fixed
“I identify as female.”
“Just male. I feel that we have chosen the most obvious variable
(genital appearance) to distinguish between the sexes, but it is not the
most accurate. I feel that I am (and always have been) male, just a
male of the XX variety (rather than XY).”
How do you describe your gender identity?
Range of Responses: More Fluid
“Fluid. I'm definitely queer and find myself going through different
phases in my gender identity. Sometimes I feel very male, sometimes
I just want to be in a drag, sometimes I feel like a tomboy and
sometimes I feel like a girl - not a girly girl, but female. So - if i had to
give it one term, Genderqueer.”
“I identify as trans, I suppose. There are days when I feel like a boy or
like a guy, but there are days when I just don't know what I am,
although I'm sure that I'm NOT a girl.”
Who is Transgender?
Conceptualizations & Expressions
Identity Group
Facets
Gender
Identity
Gender
Presentation
Sexual
Orientation
Transitional
Status
Total
(170; 100%)
Female/
Woman
female/woman
Gender
Fluid
Gender
Transitional
anti-binary
"transmasculine"
(e.g androgynous)
spectrum
Male/
Man
male/man
female typed
alternating or
simultaneous
trending
masculine
male typed
"lesbian" or
"bisexual"
unrestricted
unrestricted
unrestricted
non-op
non-op*
active
consideration
active
transition
27 (16%)
27 (16%)
27 (16%)
89 (52%)
Developmental Milestones
Milestone
Age Range
(years)
1st recognized difference
5 to 7
Earliest transgressions
5 to 7
1st wish to be born male
8 to 11
1st confusion
12 to 15
1st disclosure
16 to 19
1st passing
16 to 19
1st thoughts of transition
20 to 26
Need for hormones / surgery
20 to 26
Pride
27 to 30
Proportion of Respondents by Time & Group
Reporting a “Need for Surgery/Hormones”
100
90
Proportion of Respondents (%)
80
70
60
50
40
30
20
10
0
<5
5 to 7
8 to 11
12 to 15
16 to 19
20 to 26
27 to 30
Age Range (years)
Female/Woman
Male/ Man
Gender fluid
Gender transitional
31+
Transsexual
A subset of transgender, representing one end
of the continuum, who are “born into the wrong
body”; gender identity is highly discordant with
biologic sex, resulting in gender dysphoria and
the desire/need to modify the body to reflect
the gender identity.
Transsexuality
Prevalence
Etiology
Morbidity & Mortality
Implications for College Health
Diagnosis
Treatment
Meeting the need in College Health
Prevalence of Transsexuality
Old statistics based on surgeries:
Newer estimate of MtF, based on number of male-tofemale surgeries performed per male US population:
1 in 30,000 for MtF
1 in 100,000 for FtM
1 in 2500
These are individuals who can afford surgery
Many individuals never undergo surgery
FtM surgery is far less commonly performed
At Cornell
19,800 students in Ithaca
Dr. Hall currently has 5 trans patients
Historically 5-12 students in trans support group
19,800 / 8 = 1 in 2475
This is a young population – many have not yet “come out” or
transitioned
Prevalence of Transsexuality
160
135
140
120
100
80
60
40
40
32.9
20
9.3
8.2
16
0
Transsexuality
Accidental
Death
Homicide
Suicide
IDDM
Hypothyroidism
Prevalence/Incidence rates per 100,000 Adolescents, age 15-19
CDC national Vital Statistics Reports, Vol 56, No 5, Nov 20, 2007
Transsexuality - Etiology
Socialization or mental illness - NO
? Part of nature’s variety
? Dissonance in development
Gonadal differentiation begins 7th week of
gestation
External genitalia develop 9th-14th weeks
Sexually dimorphic areas of the brain develop
and mature from early gestation, beyond
birth, into childhood and post-puberty
Brain anatomy of gender identity
Volume of BST
Heterosexual
male
(bed nucleus of stria terminalis)
Heterosexual
female
Homosexual
male
in hypothalamus
TransWoman
(male to female)
Zhou et al., A sex difference in the human brain and its relation to transsexuality. Nature. Vol. 378, 2 Nov. 1995
Transsexuality – Morbidity & Mortality
- Extrinsic
We live in a very strictly gender binary society
When a a baby is born…
Pink vs blue clothing, décor, bike, backpacks, etc.
Identifying documents
Medical forms
Bathrooms
Dorms
Little tolerance for any gender variance
Homosexuality can be seen as a form of deviance
from expected gender role, and is still severely
punished by some segments of society
Transsexuality – Morbidity & Mortality
- Extrinsic
5-fold increased risk of murder
1 in 800 in Netherlands study
www.rememberingourdead.org
Brandon Teena, Gwen Araujo
Harassment
Discrimination
Home / Family
Public
Work – still no gender-inclusive ENDA
Transsexuality – Morbidity & Mortality
- Extrinsic
Substandard health/medical care
Discrimination by providers (32%*)
Tyra Hunter – died after MVA due to EMS discontinuing
care and then substandard ER care in Wash DC
Fear of discrimination – may not seek care (32%*)
Fear of disclosure
Due to SES factors, high number of uninsured (47%*)
Inadequately trained health personnel
*Washington Transgender Needs Assessment Survey, Xavier, 2000
Transsexuality – Morbidity & Mortality
- Intrinsic
Mental Health Implications
Internalized transphobia
Gender Dysphoria
Suppression of feelings of gender identity
Shame, guilt
Social isolation
Depression
Anxiety
Social isolation
Stress of a highly persecuted minority
Transsexuality – Morbidity & Mortality
Study
n
Lundstrom 1984
Kuiper and
Cohen-Kettenis
1988
Clements-Nolle
2006
Xavier 2000
Suicidality Suicide attempt
20%
141
19% FTMs
24% MTFs
515
32%
263
35%
16%
Transsexuality – Treatment Efficacy
Study
Pre-treatment
Lundstrom Suicidality
1984
20%
Kuiper
1988
Post-treatment
1-2%
Suicide attempts
19% FTM
0% FTM
24% MTF
6% MTF
Defining the need…Vignette cont.
Rick began to live as a male – clothing,
hairstyle, pronoun, name
Legally changed his name to reflect male
gender identity
Changed name with the registrar
Changed drivers license
Defining the need…Vignette cont.
Made an appointment with one of our
physicians to ask for testosterone rx
Researched the topic thoroughly
Sent copious reference materials to the
physician in advance of the appt for the
MD to review
Also sent letter from therapist certifying
readiness/eligibility
Defining the need…Vignette cont.
At the appt, patient was told by the physician that s/he
could not help him at that time:
Had no training in treatment of transsexuality
No previous experience, had never done it before
No one else was doing it
Didn’t have a good understanding of transsexualism / gender
dysphoria, therefore couldn’t be confident in assigning him that
diagnosis
Didn’t have a good understanding of the risks involved
Local endocrinologist also couldn’t help, didn’t know any other
resources for information, support, or consultation
Physician didn’t know where else the patient could go
Why the college health provider is the
perfect person to prescribe hormones
Good understanding of biopsychosocial model
We know about identity development
Familiarity with hormones
Comfortable discussing sexual health, anatomy,
sexuality
The majority of trans people who will need
hormones will need them starting ages 16-26
It’s not technically difficult to do
Resources and training are available (here’s some!)
Many other college health centers are doing it
Strong sense of social justice
Our Students Need Us
Need for hormones and surgery arises at the
same time they are on our campuses
Need holistic care, not just endocrinology
Trans-specific care is not available in many
areas – they have no other local options
Economics – student health center may be only
place they can afford care
Providing trans-specific care illustrates our
commitment to diversity, inclusiveness, and
social justice
Diagnosis
Diagnosing
Gender Identity Disorder
and Transsexualism
Listen to the patient
Obtain consult of trained mental health provider
Exclude other causes
Intersex
Psychosis
Major depressive disorder
Dissociative identity disorder
Other trans spectrum
DSM IV Diagnostic Criteria
Gender Identity Disorder
A strong and persistent cross-gender
identification manifest by a stated desire to
be the other sex or to live or be treated as
the other sex.
A persistent discomfort with his or her sex
or sense of inappropriateness in the
gender role of that sex manifest by a
strong desire to change their physical
primary and secondary sex characteristics .
DSM IV Diagnostic Criteria
Gender Identity Disorder
The disturbance is not concurrent with a
physical intersex condition.
The disturbance causes clinically
significant distress or impairment in social,
occupational, or other important areas of
functioning.
ICD-9 Coding for Diagnosis
TRANSSEXUALISM (F64.0)
Desire to live/be accepted as a member of the opposite
sex with a desire to make body congruent with that
gender.
Identity persistent at least 2 years
No mental health or chromosomal/anatomic abnormality
DUAL-ROLE TRANSVESTISM (F64.1)
GENDER IDENTITY DISORDER OF CHILDHOOD
(64.2)
Importance of Establishing
Diagnostic Criteria for
Gender Identity Disorder
and Transsexualism
Establishing medical standards of care
Securing insurance benefit coverage
Setting legal rights and responsibilities
Supporting research opportunities for
medical care improvements
Diagnosis – Take Home
Listen to the patient – avoid assumptions
Important to distinguish gender
“nonconformity” from gender “dysphoria”
If it’s not clear, if you’re not sure, or if the
patient isn’t sure, refer to a provider with
more expertise
The Care TEAM: Mental Health and
Medical Providers
MENTAL HEALTH PRACTITIONER ROLE
Assess for accurate GID and co-occurring conditions
Counsel on medical/mental health care options
Assess for and document transition readiness
Provide mental health consultation to treatment team
Provide mental health care for patient /family
PHYSICIAN ROLE
Understanding of standards of care, eligibility criteria,
readiness requirements and treatment needs
Assess for health status and co-occurring conditions
Prescribe, monitor and manage trans-care treatment
as well as provide routine health and wellness care
Provide Medical/Legal documentation as needed
Transsexual Treatment Goals
To bring physical body more into alignment with
person’s sense of self / gender identity in order
to relieve gender dysphoria
Ability to live in the world in congruence with
gender identity, hopefully without harassment
For different people, this means differing levels
of treatment, spanning behavioral, medical, and
surgical options
Ideally, something that looks good, feels good,
and “works good”
Priority Treatment Goal
Person is able to live their life in
congruence with their gender
identity
Transition
The process of changing one’s appearance
and/or body to reflect the true internal
gender identity.
It can include behavioral, legal, medical,
and surgical interventions.
Treatment
Mental Health
Behavioral / Non-Medical
Hormonal
Surgical
Treatment – Mental Health
Psychotherapy usually an integral part of tx
Enormous stressor of being transsexual
Counseling about medical interventions
Support for coming-out process
Gathering support for transition
Deciding what degree of transition is needed
for that individual
Letters of support for medical and surgical tx
Non-Medical Treatment Options
Male to Female (MTF)
Hair removal
Clothing
Hairstyle
Breast prosthesis
Voice training
Cosmetics
Female to male (FTM)
Theatrical facial hair
Clothing
Hairstyle
Breast binding
Weight-lifting
Padding underwear or
penile prosthesis
Medical Treatment Background
Dr. Harry Benjamin
1885-1986
Pioneer in the field
Principles of Dr. Benjamin’s Approach,
later codified into “Standards of Care”
HBIGDA - WPATH – World Professional Association for
Transgender Health www.wpath.org
“Triadic Therapy”
Real-life Experience / Behavioral treatment
Hormonal / Medical treatment
Surgery
Gradual process from fully reversible, to partially
reversible, then irreversible interventions
Eligibility requirements often seen as a barrier by
patients – meant to be a guideline
Readiness Criteria proposed to optimize successful
transition and satisfaction goals
Can also serve as validation
WPATH Standards of Care
The Real-Life Experience
To maintain full- or part-time employment
To function as a student
To function in some community-based volunteer
activity
To undertake some combination of 1-3
To acquire a legal gender-identity appropriate first
name
To provide documentation that persons other than
the therapist know that the patient functions in the
desired gender role
Adult Transition Sequence:
“Triadic Therapy”
Psychotherapy or Real Life Experience (RLE) – 3 months
Assess and understand underlying ideas and establish diagnosis
NOT “treat/cure” the GID
RLE: adopting new gender role/presentation in everyday life.
RLE assesses transition resolve/readiness NOT diagnosis
Documentation: Letter of support for Medical Therapy
Medical: Hormone Therapy
Continuing Therapy and Real Life Experience – 12 to 24
months
Documentation: Letter of support for Surgical Therapy
Surgery: Genital Reconstruction/ Surgical Reassignment
Medical / Hormonal Treatment
WPATH Standards of Care
Eligibility Criteria:
Age 18
Demonstrable knowledge of the risks and benefits
Either
A documented real-life experience of at least 3 months
A period of psychotherapy, duration specified by counselor,
usually a minimum of 3 months
Readiness criteria:
Further consolidation of gender identity during the Real Life
Experience or psychotherapy
Progress in mastering other co-morbidities (suicidality,
substance abuse)
Likely to take hormones in a responsible manner
Typical Narrative (following
Standards Of Care)
Accept your trans identity and seek help
Internet, local groups, organizations
Find a therapist and get a dx (and letter)
3 month 'Real Life Experience' OR
Psychotherapy (duration usually 3+months)
Find a physician
Start hormone therapy
FTM chest surgery can start with HRT
>1 year successful – genital surgery
Initiating Medical
Treatment
Getting Started…..
Health Maintenance and
Screening
Health Maintenance and
Screening
The Two Commandments
The Two Commandments
Medical Treatments:
Fundamentals
Set realistic goals
What will, might, and won't happen
Emphasize primary and preventative care
Use the simplest hormonal program that
will achieve goals
Every option doesn't work for every
patient
Cost, ease of use, safety
Medical Treatments:
Fundamentals
Patience is a virtue
Side effects are in the eye of the beholder
Puberty comparison
Take a long term outlook – safety and efficacy
Baldness
Screening:
Medical Treatments:
Fundamentals
Patience is a virtue
Side effects are in the eye of the beholder
Puberty comparison
Take a long term outlook – safety and efficacy
Baldness
Screening:
Medical Treatments:
Fundamentals
Hormone treatments are one of the
easiest parts
FTM – Testosterone to normal male dose
Dose that masculinizes and stops menses is
enough
MTF – More difficult because must
suppress testosterone production to get
best results
Anti-androgen(s) – Spironolactone most common
in US
Estrogens titrated to higher than normal
replacement doses for women
Medical Treatments: MTF
Estrogens at high dose
Anti-Androgen
3-5x normal female replacement doses
Partially to feminize
Partially to better suppress testosterone
Spironolactone and others
Orchiectomy
Results variable
Age at starting is important
Genetics plays a big part
Hormones: MTF - Estrogens
Oral - $
IM – Delestrogen $$
Premarin 1.25 – 10mg/d (usual 5-6.25)
Estradiol 1-5mg/d (usual 2-4)
Ethinyl Estradiol (OCPs) – drug interactions (PIs, P-450)
10-40mg q2weeks
Can't easily 'stop' in an emergency when patient
immobilized
Strohecker's Compounding Pharmacy www.stroheckersrx.com
Transdermal – Estradiol patch $$$
0.1-0.3mg/day (1-3 patches/week – overlapped)
Probably the safest for transwomen predisposed to
thrombo-embolic dz (age>40, smoking, FH, etc.)
Patient's often wary of starting but some prefer after
trying it
Hormones: MTF - Estrogens
Estrogens - “Mixing E formulations”
Some patients prefer –
?psychological effect?
Keep track of total dose
Lyon-Martin protocol
Tom Waddell protocol:
www.dph.sf.ca.us/chn/HlthCtrs/HlthCtrDoc
s/TransGendprotocols.pdf
Tendency for some to increase dose
Hormones: MTF - Estrogens
Hormones: MTF - Estrogens
Hormones: MTF - Estrogens
Beneficial effects
Breast growth
Suppress androgen production
Change of body habitus (muscle and fat)
Softening of skin
Contraindications/Precautions
Same as in cis-gender women
Individual risk/benefits (MTF get greater
benefits r/t mental health than menopausal
cis-gender women.)
In MTF with absolute CI – at least suppress
testosterone
Hormones: Estrogens Adverse
Effects
THROMBOEMBOLIC DISEASE
Hepatotoxicity (especially ORAL) – incr TA,
adenomas
Prolactinoma (if dose is too high)
Decreased glucose tolerance
Lipid profile
Gallbladder Disease
Worsening migraine/seizure control
Acne
Breast Cancer
Mood
Decreased libido
Hormones: MTF –
Anti-Androgens
Antiandrogens - All
Spironolactone 50-200 mg/d divided bid
Decrease T production or activity
Slow/stop MPB, decreases facial/body hair growth
Decrease erections/libido
Improve BPH
Cheap, reasonably safe
Hyper-K+, diuresis, changes in BP, 'just don't like it'
Decreased H/H (T erythropoetin)
Cyproterone
Hormones: MTF –
Anti-Androgens
5-α-reductase inhibitors
Finasteride, dutasteride, saw palmetto
Finasteride (Proscar/Propecia)
Stops conversion of T
DHT
5mg tabs = $70 for 30 on Drugstore.com
(~$40 at online Canadian pharmacies)
1mg tabs = $60 for 30 on Drugstore.com
(~$30 at online Canadian pharmacies)
Hormones: MTF - Progestins
Usually requested for breast growth
based on anecdotal evidence of efficacy
Decrease total estrogen dose if using
progestins
No medical need to cycle – emotional
needs?
Hormones: MTF - Surgery?
Stop E two weeks before any
immobilizing event (incl SRS) resume a
week after ambulating regularly
ASA for those with increased
risk of TE-dz (and maybe for
those without)
ASA stopped before surgery!
Hormones: MTF - Efficacy
What is adequate treatment?
Pt outcomes – breast growth (peak 2-3 yrs),
changes in skin, hair, fat/muscle, libido
The floor – testosterone levels (female range)
The roof – prolactin level
Hormones: MTF - Monitoring
Every Visit
BP, Weight, BMI
Safety
Mental health
General screening based on age, organ,
gender, and sex appropriate norms
Patient education
S/Sx of TEDz
Healthy Habits
Vision changes or lactation
Hormones: MTF - Monitoring
Clinical monitoring most important
Same adverse events in cis-gender pts
w/ same meds (use what you know!)
Labs
0, 2, & 6 mo initially then (semi)annual or
after dose changes
CBC, CMP, Lipids
Glucose
+
K
Cr
Prolactin and T
AST/ALT
Prolactin
Hormones: MTF - Monitoring
1st Pass Metabolism
AST/AST
Pituitary
Adenoma
Prolactin
Hormones: MTF – Adverse
effects
Prolactin levels
>20 possibly too much (? 'extra' E or other
meds)
>25 probably too much
>30 definitely too much
Elevated Prolactin: Stop Estrogens
(not anti-androgen)
If levels normalize, resume E at lower dose
If levels remain high MRI r/o Prolactinoma
Hormones: MTF – Adverse
effects
Elevated LFTs
Look for other cause!
If due to E, lower dose or stop until LFT
normal
Medical Treatments: FTM
Hormones: FTM
Testosterone Injected Esters (cheapest)
Cypionate
Enanthate
Biggest vial is 5ml
Slightly more expensive
Other forms (not easily obtained in US)
200mg/ml: 1-10ml vials
Cheapest - $125 for 10ml (~4mos supply)
Intramuscular testosterone undecanoate
(Nebido)
Higher levels from injected maybe better
for earlier transition
Hormones: FTM
Therapeutic
Range
200 mg
2 weeks
100 mg
week
Steady State
Usually achieved after 3-5 T½
T ½ of esters = 8-10 days
Therapeutic
Range
Hormones: FTM
Transdermal
Expensive: $7 day retail, $1/day
compounded
Less variable levels
Daily administration
Risk of inadvertent transfer to others
1%, 5g QD
5%, 1g QD
Hormones: FTM - Monitoring
Every Visit
BP, Weight, BMI
Safety
Mental health
General screening based on age, organ,
gender, and sex appropriate norms
Patient education
Vaginal bleeding
Healthy habits
Tx available for acne, MPB
Medical Treatments:
Fundamentals
Clinical monitoring most important
Same adverse events in cis-gender pts
w/ same meds (use what you know!)
Labs
0, 2, & 6 mo initially then (semi)annual or p
changes
Glucose
CBC, CMP, Lipids
Cr
Hgb
T (trough) in FTM
ALT
T
Hct
Treatment Effects (any
delivery...)
Nearly immediate
Increased sebum and resultant acne
Increased sex drive
Sometimes – amenorrhea
Metabolic changes start
Emotional effects of 'finally starting T'
Treatment Effects
1-6 months
Voice change starts – parallels adolescence
Hair growth (and loss) begins: parallels
adolescence*
Clitoromegaly starts
Most amenorrhea (but E only decreases
modestly)*
Fat and muscle distribution changes
Metabolic changes
* Gooren, et al. 2008. “Review of studies of androgen treatment of FTM
transsexuals: Effects and risks of administration of androgens to
females”.
Treatment Effects
1-5 Years
Voice settles
Final fat and muscle redistribution
Clitoromegaly maxes
Length average 4-5cm (3-7 cm range)1
Volume increases 4-8x2
Greater change in younger patients2
Breast involution?
1 Meyer W, et al. 1986 “Physical and hormonal evaluation of transsexual
patients: a longitudinal study.”
2 Gooren, et al. 2008. “Review of studies of androgen treatment of FTM
transsexuals: Effects and risks of administration of androgens to
females”.
Do they really shrink?
Breast involution?
Yes: 23 pts Slagter, et al. 2006. “Effects of Longterm Androgen Administration on Breast Tissue of
Female-to-Male Transsexuals.”
No: 29 pts Burgess & Shousha. 1993. “An
immunohistochemical study of the long-term
effects of androgen administration on female-tomale transsexual breast: a comparison with normal
female breast and male breast showing
gynaecomastia.”
Some do, some don't: 2 other studies (14 total)
At a minimum the fat decreases with
metabolic changes
Treatment Effects
5-10 years
Final hair growth
Androgenic alopecia can happen at any age
– and does in 50% of FTMs by 13 years*
* Gooren, et al. 2008. “Review of studies of androgen treatment of FTM
transsexuals: Effects and risks of administration of androgens to
females”.
Hormones: FTM – Adverse
effects
Acne – MC side effect (chest/back)
CV - worsening of surrogate endpoints lipids, glucose metabolism, BP
Polycythemia (normals for males)
Unmask or worsen OSA
Enhanced Libido
Androgenic alopecia
'Other' hair growth
Androgenic Alopecia
T
5-α-reductase
DHT
Finasteride
aromatase
E
aromatase
not very
active stuff
Hormonal Treatments: Is this
safe?
Van Kesteren P, et al. “Mortality and
morbidity in TS subjects treated with
cross-sex hormones.” Clin Endo (Oxf).
47(3):337-42.1997.
DESIGN: Retrospective, descriptive study @
university teaching hospital that is the national
referral center for the Netherlands (serving 16
million people)
SUBJECTS: 816 MTF & 293 FTM on HRT for total
of 10,152 pt-years
OUTCOMES: Mortality and morbidity incidence
ratios calculated from the general Dutch
population (age and gender-adjusted)
Hormonal Treatments: Is this
safe?
Van Kesteren P, et al. “Mortality and
morbidity in TS subjects treated with
cross-sex hormones.” Clin Endo (Oxf).
47(3):337-42.1997.
293 FTMs
c/w ♀
????
10,152
pt years
816 MTFs
c/w ♂
????
Hormonal Treatments: Is this
safe?
Van Kesteren P, et al. “Mortality and morbidity
in TS subjects treated with cross-sex
hormones.” Clin Endo (Oxf). 47(3):337-42.1997.
MTF/FTM total mortality no higher than general popl'n
Largely, observed mortality not r/t hormone treatment
VTE was the major complication in MTFs.
Fewer cases after the introduction of
transdermal E in MTFs over 40.
VTE
In MTFs increased morbidity from VTE
and HIV and increased proportion of
mortality due to HIV
HIV
Hormonal Treatments: Is this
safe?
Van Kesteren P, et al. “Mortality and
morbidity in TS subjects treated with
cross-sex hormones.” Clin Endo (Oxf).
47(3):337-42.1997.
293 FTMs
c/w ♀
No Increase Morbidity
or Mortality
10,152
pt years
816 MTFs
c/w ♂
No Increase Mortality
Increase morbidity r/t HIV/VTE
Hormonal Treatments: Is this
safe?
Van Kesteren P, et al. “Mortality and
morbidity in TS subjects treated with
cross-sex hormones.” Clin Endo (Oxf).
The absence of
47(3):337-42.1997.
evidence is not
evidence of absence
Hormonal Treatments: Is this
safe?
Gooren L, et al. “Long term treatment of
TSs with hormones: Extensive personal
experience.” J Clin Endo & Metab.
93(1):19-25. 2008.
Same clinic group as 1997 paper – now 2236
MTF, 876 FTM (1975-2006)
Outcome M&M Data, data assessing risks of
osteoporosis and cardiovascular disease, cases of
hormone sensitive tumors and potential risks
Hormonal Treatments: Is this
safe?
Gooren L, et al. Cardiovascular Risks
Analyzed studies of surrogate markers for CVDz
in MTF/FTM: Body composition, lipids, insulin
sensitivity, vasc function, hemostasis/fibrinolysis,
others (HC CRP)
Some worsen, some improve, some are
unchanged – much of the worsening seem
likely due to weight
MTF do worse than FTM
Hard clinical endpoints show no
difference
Cardiovascular Disease
What really killed the dinosaurs
Cardiovascular Disease
Screen and treat for modifiable risk
factors in all patients
Try to get modifiable risk factors under
control before starting hormone
replacement therapy
Be respectful of patient autonomy and
the difficulty of modifying certain risk
factors
Cardiovascular Disease - MTF
Estrogen use increases risk for CVDz in
cis-gender women
Estrogen use in transgender women
worsens
surrogate
markers
for
CVDz
(Gooren et al.)
Its a pretty good bet that Estrogen use in
transgender women increases risk of
CVDz
Transdermal
estrogen
is
the
least
risky
(Gooren et al.)
Aspirin use may ameliorate some of the
increased risk
Cardiovascular Disease - MTF
Consider treadmill stress in patients with
multiple significant risk factors for CVDz
prior to starting hormones*
Patient education and clinical monitoring
for signs and symptoms of vascular
events
Be especially cautious in first two years of
hormone treatments (Gooren et al.)
*if reasonable given patient's situation
Cardiovascular Disease - FTM
Testoeterone use in transgender men
worsens surrogate markers for CVDz, but
not as bad as estrogen in MTFs (Gooren et al.)
It is possible that testosterone use in
transgender men increases risk of CVDz
Motivate patients to take care of
modifiable risk factors
Cardiovascular Disease - FTM
Consider treadmill stress in patients with
significant risk factors for CVDz prior to
starting hormones*
Patient education and clinical monitoring
for signs and symptoms of vascular
events
*if reasonable given patient's situation
CVDz Risks: Hypertension
Blood pressure at every visit for FTM and
MTF
Both exogenous estrogen and testosterone
can cause increases in blood pressure
In MTF patients with hypertension,
spironolactone should be part of
treatment if tolerated
CVDz Risks: Dyslipidemia
Annual fasting lipids in FTM and MTF
Target LDL < 130 if no other risk factors
Higher peak serum levels worsen lipids in
both
If hyperlipidemia exists
Transdermal or weekly IM T in FTMs
Transdermal (especially if elevated TGs)
CVDz Risks: Diabetes
Annual fasting glucose in FTM and MTF
Both exogenous estrogen and testosterone
worsen glucose tolerance (Gooren et al.)
Both exogenous estrogen and testosterone
cause weight gain (Gooren et al.)
Transgender men with PCOS
are at increased risk of DM-2
DM-2 or DM-1 are not
contraindications to HRT
CVDz Risks: Smoking
LGBT communities have greater rates of
smoking, alcohol, and drug abuse
Bar culture
Targeted marketing
Vulnerable youth
Smoking is a greater risk in
MTFs due to risk of DVTs
with estrogen supplementation
Hormonal Treatments: Is this
safe?
Gooren L, et al. Hormone Dependent
Tumors
Lactotroph Adenoma
Rare
Check PROLACTIN
Prostate Cancer
Prostatectomy is not a part of SRS
Screen based on the organs present
Withdrawal of testosterone may
decrease but doesn't eliminate the risk
of BPH and malignancy
Hormonal Treatments: Is this
safe?
Digital Rectal Exam is a little different
Cancer – Breast MTF
Risk increases with
Age
Estrogen duration > 5 years
Progestagen exposure
Positive FH
Obesity
Consider mammogram for age > 50 +
other risk factor
Weigh risks and benefits of mammography
Augmentation and silicone pumping impair
sensitivity
Cancer – Vaginal MTF
Case reports of neovaginal condyloma
and one case of neovaginal dysplasia
In patients with penile inversion
vaginoplasty and history of genital warts
or HPV positivity or exposure to HPV
consider vaginal paps
HPV assay????
Hormonal Treatments: Is this
safe?
Gooren L, et al. Hormone Dependent
Tumors
Breast cancer FTM
Reported in 1 case 10 years after mastectomy
Mastectomy reduces but doesn't eliminate risk
Some injected testosterone is aromatized to
estrogen
Family history
Pre-op mammo and post-op path????
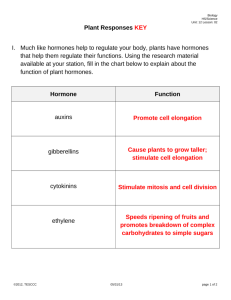
Hormonal Treatments: Is this
safe?
Gooren L, et al. Gynecologic Tumors
Gynecologic Tumors
Cervical
Ovarian
Endometrial
Gynecologic Cancer risks in
FTMs
4 + ???
???
Gynecologic Cancer risks in
FTMs
Normal
Hyperplasia
Dysplasia
F
T
M
???
P If
C infrequent
O periods
S
Cancer
ENDOMETRIAL
CANCER
Gynecologic Cancer risks in
FTMs
Gynecologic Cancer risks in
FTMs
Cervical Cancer Risk Reduction from Pap Smears
100
90
80
70
60
50
40
30
20
10
0
Never
Every 10 yr
Every 5 yr
Every 3 yr
Every 2 yr
Every year
IARC Working Group on Evaluation of Cervical Cancer Screening Programmes. Screening for squamous
cervical cancer: duration of low risk after negative results of cervical cytology and its implication for screening
policies. Br Med J. 1986;293:659-664.
Gynecologic Cancer risks in
FTMs
Gynecologic Cancer risks in
FTMs
Cancer – Cervical FTM
Consider HPV testing if very difficult paps
Testosterone induces atrophy: tell the
pathologist!
Consider hysterectomy as alternative if
greater surveillance needed in pts with
extreme difficulty with paps (ex high
grade SIL)
Osteoporosis
Vitamin D, Calcium and Exercise for
anyone
Gonadectomy increases risk
Osteoporosis – MTF
Pre-Orchiectomy – no different than risk
of cis-gender men
Post-Orchiectomy
Continue hormones permanently unless good
CI
If estrogen CI'd use Ca and Vit D and screen
for osteoporosis
If present treat osteoporosis/osteopenia as in
cis-gender women
Osteoporosis – FTM
Pre-Oophorectomy
Screen as cis-gender women
Effect of T uncertain
If on provera > 5 years risk may be increased
Post-Oophorectomy
Continue hormones permanently unless good CI
If T contraindicated, consider bisphosphonates
If T contraindicated (or patient on lower dose or
off for substantial periods) consider earlier
screening
Hormonal Treatments: Is this
safe?
Gooren L, et al. “Long term treatment of TSs with
hormones: Extensive personal experience.” J Clin Endo
& Metab. 93(1):19-25. 2008.
Conclusion: “It is clear now that sex reassignment of TSs
benefits their well-being, although suicide rates remain
high. Cross-sex hormone administration to TSs is
acceptably safe in the short and medium term. However,
potentially adverse effects in the longer term are
presently unknown. The data, although limited, of
surrogate markers of CVDz and the reports of cancer in
transsexuals leave room for cautious optimism. But true
insights can only come from close monitoring and
thorough reporting of adverse effects in the
literature.
Sexually Transmitted Diseases
Risk is determined by behaviors and partners
Risk is not determined by identity
Ask sexual health questions based on
behaviors while respecting identity
Example: A transwomen who has sex with
men is heterosexual but is at greater risk if:
She is the receptive partner in anal intercourse
Her partner has or had sex with men
She feels pressure to have unprotected sex due
to fear of rejection or desire to express love for
her partner
Sexually Transmitted Diseases
HIV
Hepatitis A, B, C
Syphilis
Gonorrhea, Chlamydia, Trichomoniasis
HPV
Herpes I and II
What about regret ???
Pfäfflin, F., & Junge, A. (1998). Sex reassignment –
Thirty years of international follow-up studies; SRS: A
comprehensive review, 1961-1991 Düsseldorf ,
Germany: Symposion Publishing.
74 f/u studies and 8 reviews published b/w 19611991
Less than 1% long term regret in over 400 FTMs
1.5% regret in over 1000 MTFs
Compare with regret rates for gastric bypass, breast
recon after mastectomy, surgical sterilization
Studies after 1991 show lower rates of regret (and
found risk of regret correlates well with surgical
success.)
Is it effective?
Suicidality decreased from 20-30% pretreatment to 3% post treatment
Decreased depressive symptoms,
improved social functioning, regrets rare
And you be the judge....
Surgical Treatments
Non-Genital Surgery
Transwomen
Transmen
Facial Feminization
Rhinoplasty
Facial bone reduction
Blepharoplasty
Face lift
Breast Augmentation
Thyroid chondroplasty
(trach shave)
Voice modification
Suction lipoplasty
Chest Reconstruction
b/l mastectomy
Nipple grafting
Re-contouring
Liposuction
Facial Feminization Surgery (FFS)
Facial Feminization Surgery
Chest Reconstruction
Genital Surgery Options
Transwomen
Orchiectomy
SRS/GRS
Transmen
Clitoral release /
Metoidioplasty
Urethroplasty
Scrotoplasty
Testicular Implants
Phalloplasty
Vaginectomy
Hyst/BSO
SRS/GRS for Transwomen
Removal of testes and scrotum
Creation of vagina using “penile inversion”
Re-positioning of urethra
Creation of clitoris and labia
Requires post-op dilations to maintain neovagina
Often require lubricant for intercourse
Can get vaginitis like any other women
SRS/GRS
Vaginoplasty & Labiaplasty
Metoidioplasty
Creates a small neo-phallus
Freeing of the hypertrophied glans clitoris from
suspensory ligaments
Repositioning to more superior location
+/- liposuction of mons area
+/- bulking up on glans with other tissues
+/- scrotoplasty, testicular implants, and
urethroplasty
Some patients will use topical 2% testosterone
and/or clitoral pumps to increase size of glans in
preparation for genital surgery
Metaidoioplasty
(before)
MtF Transsexuals - TransWomen
FtM Transsexuals - TransMen
Trans-Specific Care in the College
Health Setting
Safe, supportive environment at health
center
Sensitivity training / education for all staff
Use correct pronouns, preferred names
Don’t make assumptions – ask
Don’t be intrusive
Keep prejudices to yourself
Rethink forms, i.e. asking for gender M/F
Trans-Specific Care in the College
Health Setting
Support and Advocacy
LGBT resource center or equivalent
Housing, registrar, name changes
Community LGBT groups
Online LGBT groups
Knowledgeable mental health providers
Within the health/counseling center
In the area
Trans-Specific Care in the College
Health Setting
Medical Care
Routine health maintenance: care for the anatomy
Hormone Prescription and Monitoring
Peri-Surgical Care
At the health center
In the community
Letters
Pre-Op exams – be sure to thoroughly examine the anatomy
which will be altered
Post-Op Wound care – suture removal, pulling drains,
assessing healing
Surgery
Know who the surgeons are, call them if questions
Trans-Specific Care in the College
Health Setting
Insurance Coverage
AMA Resolution 122
www.ama-assn.org/ama1/pub/upload/mm/471/122.doc
Meeting the Student Need
Cornell
UC Davis
All-Staff Training on Gender Identity
Yes
yes
Physician initiates and monitors hormonal tx
yes
yes
Nurses administer injections and teach pts to selfinject
yes
yes
Follow the WPATH Standards of Care
yes
yes
Provide pre-and post-surgical care
yes
yes
Pharmacy stocks / special orders hormones,
syringes, needles, and sharps boxes
yes
yes
Physician has ongoing relationship with LGBT Center yes
yes
SHIP Covers medical care and counseling
yes
yes
SHIP covers surgical treatments
Not yet
yes
Counselor trained in gender identity
yes
Not yet
Campus Trans Support group
yes
Not yet
Trans info on website
yes
Not yet
Trans-Specific Care in the College
Health Setting
You can do this.
It’s the right thing to do.
Lots of resources available
Not technically difficult
To NOT provide proven effective medical
therapy is discriminatory
You will improve your patients lives
immeasurably.
Thank you!
Questions!
msfamula@ucdavis.edu
nick@lyon-martin.org
amh89@cornell.edu
seth.pardo@cornell.edu