Wasted Ventilation - Respiratory Therapy Files
advertisement

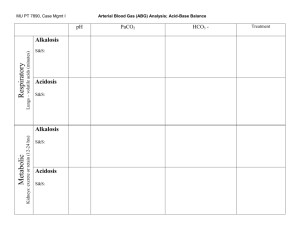
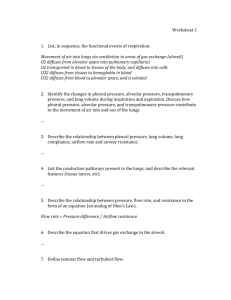
Wasted Ventilation Dead Space • dead space is the volume of air which is inhaled that does not take part in the gas exchange, either because it (1) remains in the conducting airways, or (2) reaches alveoli that are not perfused or poorly perfused. In other words, not all the air in each breath is available for the exchange of oxygen and carbon dioxide. • About a third of every resting breath has no change in O2 and CO2 levels. In adults, it is usually in the range of 150 mL. • The total dead space (also known as physiological dead space) is the sum of the anatomical dead space plus the alveolar dead space. Anatomical dead space • Anatomical dead space is that portion of the airways (such as the mouth and trachea) which conducts gas to the alveoli. • No gas exchange is possible in these spaces. In healthy lungs the alveolar dead space is small; measured by a nitrogen washout technique. • The normal value for dead space volume (in ml) is approximately the lean mass of the body (in pounds), and averages about a third of the resting tidal volume (450-500 mL). Alveolar dead space • Alveolar dead space is sum of the volumes of those alveoli which have little or no blood flowing through their adjacent pulmonary capillaries, i.e., alveoli that are ventilated but not perfused, and where, as a result, no gas exchange can occur Alveolar dead space is negligible in healthy individuals, but can increase dramatically in some lung diseases due to ventilation-perfusion mismatch. • Calculating the dead space • Just as dead space wastes a fraction of the inhaled breath, dead space dilutes alveolar air during exhalation. By quantifying this dilution it is possible to measure anatomical and alveolar dead space, employing the concept of mass balance, as expressed by Bohr equation. • where is the dead space volume and is the tidal volume; • is the partial pressure of carbon dioxide in the arterial blood, and • is the partial pressure of carbon dioxide in the expired (exhaled) air. Physiologic dead space • The concentration of carbon dioxide (CO2) in healthy alveoli is known - it is equal to its concentration in blood since CO2 rapidly equilibrates across the alveolar-capillary membrane. The quantity of CO2 exhaled from the healthy alveoli will be diluted by the air in the conducting airways, and by air from alveoli that are poorly perfused. This dilution factor can be calculated once the CO2 in the exhaled breath is determined (either by electronically monitoring the exhaled breath or by collecting the exhaled breath in a gas impermeant bag - a Douglas bag - and then measuring the mixed gas in the collection bag). Algebraically, this dilution factor will give us the physiologic dead space as calculated by the Bohr equation: Alveolar dead space • When the poorly perfused alveoli empty at the same rate as the normal alveoli, it is possible to measure the alveolar dead space. In this case, the end-tidal sample of gas (measured by capnography) contains CO2 at a concentration that is less than that found in the normal alveoli (i.e. in the blood): • • Caution: The end tidal CO2 concentration may not be a well defined number. Poorly ventilated alveoli do not generally empty at the same rate as healthy alveoli. Particularly in emphysematous lungs, diseased alveoli empty slowly, and so the CO2 concentration of the exhaled air increases progressively throughout the expiration.[ Monitoring alveolar dead space during a surgical operation is a sensitive and important tool in monitoring airway function.[11] During strenuous exercise, CO2 will rise throughout the exhalation and may not be easily matched to a blood gas determination, which led to serious errors of interpretation early in the history of dead space determinations.[8] Example: For a tidal volume of 500 mL, an arterial carbon dioxide of 42 mmHg, and an end-expired carbon dioxide of 40 mmHg: and so • • • • BEWARE OF TACHYPNEA WITH SMALL TIDAL VOLUMES • Clearance of carbon dioxide is determined by the alveolar ventilation and the physiologic dead space. • Residents frequently ask me: "why is this patient's PaCO2 (partial pressure of Carbon Dioxide in the blood) so high when he has a minute ventilation of 30 liters per minute?" • This is a common trap to fall into: confusing alveolar ventilation (which is difficult to measure) with minute ventilation (which is always measured). The difference between the two is determined by the anatomical dead space. • Two patients have a minute ventilation of 10 liters/minute: – Patient B is taking 50 breaths of 200ml tidal volume. – Patient A is taking 20 breaths of 500ml tidal volume. BEWARE OF TACHYPNEA WITH SMALL TIDAL VOLUMES • Using misplaced logic one would think that each would have the same PaCO2. In fact patient B has a significant respiratory acidosis, and patient A has a normal blood gas. Anatomical dead space is approximately 150ml in an adult male. It is important to calculate out the dead-space (Vd/Vt) to tidal volume ratio for each patient: patient A has a Vd/Vt of less than 30% (normal is 30%). Patient B has a Vd/Vt of 75%. What does this mean? In the case of patient B, 75% of his respiratory effort is being wasted, leading to severe muscular fatigue and acidosis. BEWARE OF TACHYPNEA WITH SMALL TIDAL VOLUMES • It is also important to realize that patients may have large amounts of alveolar dead space: a patient can be receiving tidal volumes of 500ml and still have a dead space ratio of 75%: how? Alveolar dead space is caused by increased volume of zone 1 (zone 1 is where alveolar pressure exceeds the perfusion pressure to the lung unit: alveoli are ventilated but not perfused): • Hypoperfusion - low pulmonary blood volume-pressure leads to underperfusion of non dependent lung segments. • Overdistension of compliant lung units: often caused by excessive PEEP. • Dead space is calculated by measuring the ratio of end tidal CO2 (etCO2) to arterial CO2 (PaCO2), using the equation: • Vd/Vt = PaCO2 - PetCO2/PaCO2 BEWARE OF TACHYPNEA WITH SMALL TIDAL VOLUMES • It is important that you are aware of physiologic dead space (anatomical dead space plus alveolar dead space) in the modern setting of low tidal volume ventilation for acute lung injury • Using tidal volumes of 4 - 5ml/kg in patients with significant atelectasis leads to considerable wasted ventilation: as a result a much higher respiratory rate than normal is required (25 to 30, frequently more) to control PaCO2. This frequently leads to problems with auto-PEEP • We know that permissive hypercapnia is associated with few complications, so most physicians elect to allow the PaCO2to climb rather than compromising oxygenation.