The Hospital Response After an Earthquake
advertisement

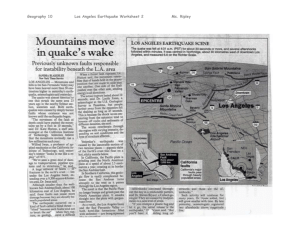
The Hospital Response After an Earthquake Carl H. Schultz, MD Professor of Emergency Medicine Director, Disaster Medical Services UC Irvine School of Medicine Introduction • Current research suggests earthquakes of magnitude 7.0 or larger occur on the Jordan Valley segment of the Dead Sea Fault about every 1000 years • The last major earthquake occurred in 1033 • Jerusalem located less than 40 km from the fault Introduction • Estimate of worst-case event: – Moment magnitude 7.5 earthquake on the Jordan Valley segment – 30 billion dollars U.S. in economic losses Introduction • Hospitals are vulnerable • 1971 San Fernando earthquake (Los Angeles, California, USA ) – 50 of 64 deaths due to hospital collapse – 4 hospitals with structural failure were closed Introduction • 1994 Northridge earthquake (Los Angeles, California, USA) – 8 hospitals evacuated patients • 6 completely – 4 of these closed and demolished • 1995 Hanshin-Awaji earthquake (Kobe, Japan) – 13 hospitals partially or totally destroyed Introduction • Delayed hospital closures can occur days to weeks after event – 2 hospitals closed 3 and 14 days after quake • Inspections not perfect – Red, yellow, and green tags – Based on objective and subjective criteria • ATC 20-1 – Political and financial considerations are involved Introduction • Office of Statewide Health Planning and Development, State of California, 2001 – 48% of California’s hospital buildings are at high risk for collapse or loss of function from structural failure after a Northridge magnitude event – 91% of nonstructural components essential to safety and patient care will fail or sustain serious damage • Rand Corporation 2007 – 305 acute care hospitals have buildings vulnerable to collapse. ½ will be condemned by the 2013 deadline due to failure to retrofit – Cost of seismic improvements: $110 billion U.S. Overview of Hospital Response • Initial assessment – Hospital – Regional • Hospital is functional – Convergence behavior – Personnel (staff) – Equipment (stuff) – Facilities (structure) – Standard of care • Hospital is non-functional – Triage – Internal patient evacuation – Off-site patient evacuation • Communication • Staff behavior • Government assistance Initial Hospital Assessment • Immediate status of environment – Performed by Charge Nurse – Manual ventilation of patients • Threats to patient safety – Evacuate to safer area of unit • Contact House Supervisor and report status Initial Hospital Assessment • House supervisor - makes initial assessment (hospital intact, partial damage, evacuation needed) – Assessment from patient care staff – Assessment from maintenance staff • Activates disaster plan – Implements hospital incident management system • Communicate with hospital director (if possible) Initial Hospital Assessment • Need basic tool for rapid assessment of structural safety – Building inspectors may take 6-12 hours to arrive – ATC-20-1 http://www.atcouncil.org/Merchant2/merchant. mv?Screen=CTGY&Category_Code=a201 • Assess not-structural components (plumbing, heating/air conditioning, generators, water supply) Initial Regional Assessment • Ideal metric – available quickly, identifies all areas of damage, easily disseminated • Traditional approach – Identification of epicenter – Measurement of moment magnitude • Richter scale – Reconnaissance – Systematic verbal reports from responders, government workers • Modified Mercalli Scale Initial Regional Assessment • Epicenter – Point on the earth’s surface overlying the where the fault rupture begins (hypocenter) – Not the area of greatest shaking • Advantages – Available quickly – Gives general location of the earthquake • Disadvantages – Not provide specific information on areas of significant shaking and damage Initial Regional Assessment • Moment magnitude – Measures overall energy release • Advantages – Gives a general measure of damage potential • Disadvantages – Poor predictor of shaking and damage at any one location – Energy not radiate out symmetrically Initial Regional Assessment • Reconnaissance – Helicopters, spontaneous reports • Advantages – Available quickly • Disadvantages – Large sampling error – ? reliability – Many areas with significant damage are not readily apparent from the air Initial Regional Assessment • Systematic reports – Government employees, typically postal workers, provide assessment of degree of shaking and observed damage – Use the Modified Mercalli Scale • Advantages – Gives fairly accurate assessment of damage distribution • Disadvantage – Slow – Difficult to distribute the information Modified Mercalli Scale Initial Regional Assessment • Any of these measure qualify? – NO. • What does? – Instrumental intensities • Peak ground velocity and peak ground acceleration are plotted as Shakemaps – Available within minutes of an earthquake – Can be downloaded by anyone from the internet – Easily interpreted by non-seismologists Instrumental Intensity Initial Regional Assessment • Shakemaps can depict the degree of ground shaking – Can this actually work and can it also assess risk for injuries and death? – YES • Data? • Epidemiologic – Ramirez, Peek-Asa: Epidemiology of Traumatic Injuries from Earthquakes. Epidemiol Rev 2005 – Peak ground acceleration was highly predictive – Distance from the epicenter in the Northridge quake was a poor predictor of injury and death Initial Regional Assessment • Disaster Medicine – Schultz, Koenig, Lewis: Decisionmaking in Hospital Earthquake Evacuation: Does Distance from the Epicenter Matter? Ann Emerg Med 2007 (in press) – No significant difference in distance from the epicenter for evacuated and non-evacuated hospitals – Statistically significant difference in peak ground acceleration measurements between both groups of hospitals Study Hospitals Control Hospitals Distance from Epicenter (miles) Peak Ground Acceleration (gravity) Condemned Distance from Epicenter (miles) Peak Ground Acceleration (gravity) Condemned Hospital 1 0.8 0.80 No Hospital A 2.8 0.49 No Hospital 2 4.0 0.89 No Hospital B 8.4 0.51 No Hospital 3 4.0 0.93 Yes Hospital C 12.7 0.34 No Hospital 4 6.7 0.74 No Hospital D 13.0 0.60 No Hospital 5 9.5 0.81 No Hospital E 15.3 0.38 No Hospital 6 12.9 0.59 Yes Hospital F 16.7 0.20 No Hospital 7 21.5 0.46 Yes Hospital G 17.3 0.28 No Hospital 8 21.8 0.46 Yes Hospital H 22.8 0.13 No 5 miles N Initial Regional Assessment • Median distance from the epicenter for evacuated hospitals = 8.1 miles (13.5 km) • Median distance from the epicenter for control hospitals = 14.1 miles (23.5 km) • Difference in medians = 6 miles 95% CI: -4.8 to 11.9 miles Not statistically significant Initial Regional Assessment • Median peak ground acceleration for evacuated hospitals = 0.77 g, where 1.0 g equals the force of gravity • Mean peak ground acceleration for control hospitals = 0.36 g • Difference in medians = 0.41 g 95% CI: 0.14 to 0.55 Statistically significant (p=0.009) Initial Regional Assessment • Take home message: – Shakemaps are useful way to assess the risk of damage across the entire region of an earthquake – Are predictive of increased risk for building damage, injury, and death – Shakemap assessment by hospital personnel and emergency managers in the immediate aftermath of an earthquake needs to be included in the disaster plans of all vulnerable regions where such information is available Hospital Is Functional • Prepare for patient convergence – Closest hospitals will receive most of the patients – Israel has real experience • Versailles nightclub collapse • Terrorist bombings – Earthquakes on larger scale – Credentialing of medical volunteers Hospital Is Functional • Alternate sites of care – Parking lots – Temporary structures (tents) – Areas not used for patient care • Classrooms • Auditoriums • Early discharge of patients – problematic • Delivery of supplies/equipment – Agreement with vendors, Home Front Command Hospital Is Functional • Change in standard of care? – Triage based on who receives care and who doesn’t – Delayed closure of lacerations – Use of ventilators – Admission to Intensive Care Units (ICUs) Hospital Is Not Functional • Triage Order of patient movement off unit: Sickest patients first – No immediate threat to safety (immediate building collapse unlikely) – Efficiency of movement not critical – Individuals use great deal of resources – Order of floor evacuation not matter Hospital Is Not Functional • Triage – Order of patient movement off unit • Healthiest patients first – Immediate risk to safety (building collapse possible) – Efficiency of evacuation important – Can move more patients with less resources (some can evacuate themselves) – May need to leave trapped patients behind – Evacuation lower floors first Hospital Is Not Functional • Internal patient evacuation – Movement of patients • Used gurneys, backboards, sheets, wheelchairs • Did not use specialized devices and would not use them if available • FLASHLIGHTS CRITICAL • Elevators will not work • Evacuation routes must only use stairs • Take patients charts and medications Hospital Is Not Functional Off-site patient evacuation • Control of hospital evacuations – Traditional model • Emergency Operations Center (EOC) controls all aspects of patient transfer • Transportation assets Ambulances, helicopters • Destination decisions – How many patients go to which hospitals – Northridge model • EOC provides vehicles to hospitals per their request • EOC and hospitals share destination decisions Hospital Is Not Functional • Northridge model (Schultz et al: New England Journal of Medicine, 2003) – 1066 patients evacuated totally, 818 in first day – How many people answering phones would it take for the EOC to coordinate the transfer of 800 patients in the midst of chaos? – Efficient use of time? – Other demands during first critical 24 hours – Use of shakemaps? Hospital Is Not Functional • Outcome – EOC able to mobilize transportation assets • Used ambulances, buses, county vehicles • Very effective at this task – EOC can coordinate movement of some patients but not all – Hospitals can and will move patients on their own – Hospitals belonging to systems will be most effective – Recognition of hospital role should be part of disaster plan Communication • Most forms of communication fail during a disaster – Telephones (damaged or over-utilized) – Cellphones (towers damaged, battery back-up fails, over-utilized) – Satellite phones (batteries not charged) – Microwave radios (repeaters down, power out) Communication • Forms of communication that function during a disaster – Pay phones – Fax lines – Certain types of internet lines – Ham radios – Police, fire, and ambulance radios (not compatible in the U.S.) Staff Behavior • Concerns regarding commitment of staff. Will they remain on duty and will replacements arrive? YES. – Studies by Quarantelli demonstrate basic volunteer nature of society – Article in JAMA after the Northridge Earthquake documenting staff dedication Staff Behavior • Hospitals reported staffing shortages after the Northridge Earthquake, some more than 50% – Not due to individuals refusing to remain on duty – Not due to unwillingness of staff to come to work. Unscheduled staff reported to hospitals – Due to inability to get to work or could not leave families Staff Behavior • Solutions to the staffing problem – Establish daycare, supervision for pets • Surge capacity – Use staff from other hospitals (Kazzi et al: Prehospital and Disaster Medicine, 2000) • Raises issues of credentialing • National vs local database • Resolved within 7 days Government Assistance • Government assistance critical for overall response but may not be acute care asset • May arrive too late to impact initial outcomes in a significant way • Biggest impact in supporting ongoing health maintenance • Attack after earthquake • Transportation an issue United States Teams • Urban Search and Rescue teams – Riverside County team 2 hours away by car – Earthquake occurs at 04:30 – Team not begin activities at site of Northridge Meadows Apartment collapse until 23:30 – Live victims already extricated United States Teams • Oklahoma City Bombing 1995 – Multiple USAR teams dispatched – Last survivor recovered from building 18 hours after explosion – Number of survivors recovered by out-of-state USAR teams: – ZERO United States Teams • Disaster Medical Assistance Teams – No teams arrived in the first 24 hour (Leonard et al: Prehosp & Disaster Med 1995) – 4 team arrived in the next 24 hours, 3 from California – Each team can see up to 200 ED type patients or 400 clinic patients per day – Demand for emergent care back to baseline by 7 days Israeli Home Front Command Urban Search and Rescue Team • January 2006: Nairobi, Kenya building collapse • 117 victims found in collapsed building • Israeli Home Front Command forces arrived 23 hours after event • Rescued 2 individuals, one a volunteer who became trapped after the event Government Assistance • Local solutions – Granada Hill hospital • Staff shortages • Used staff (MDs and RNs) from UCI Medical Center to support Emergency Department Care • Surge capacity: National database? TODA RABAH Carl H. Schultz, MD 1-714-456-3713 schultzc@uci.edu