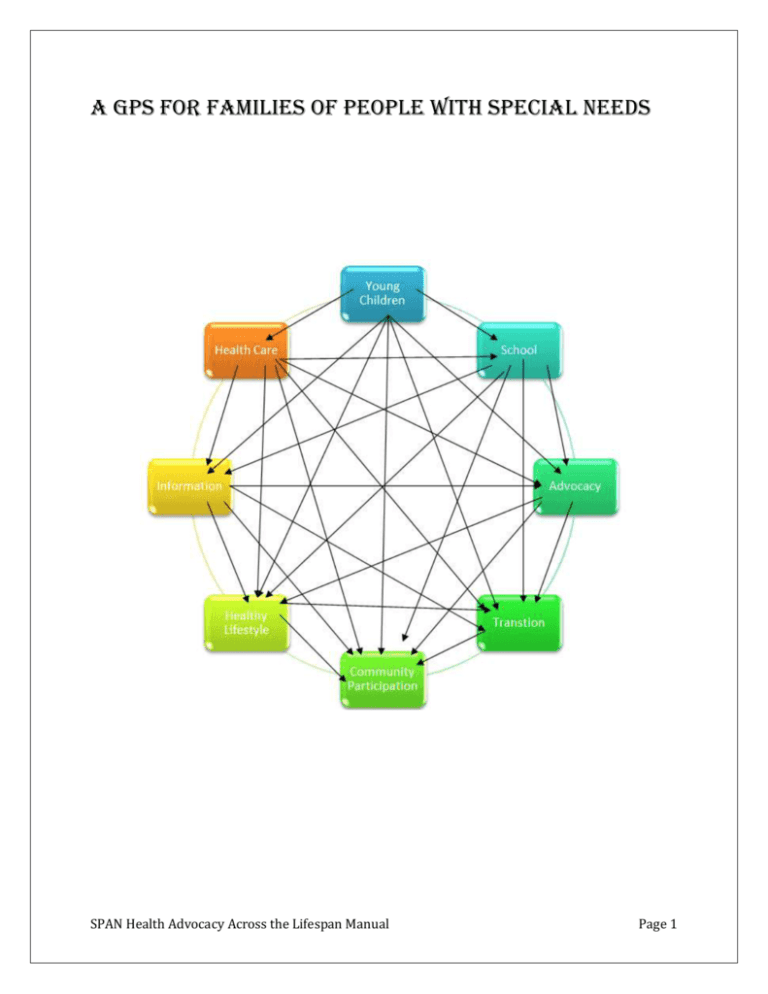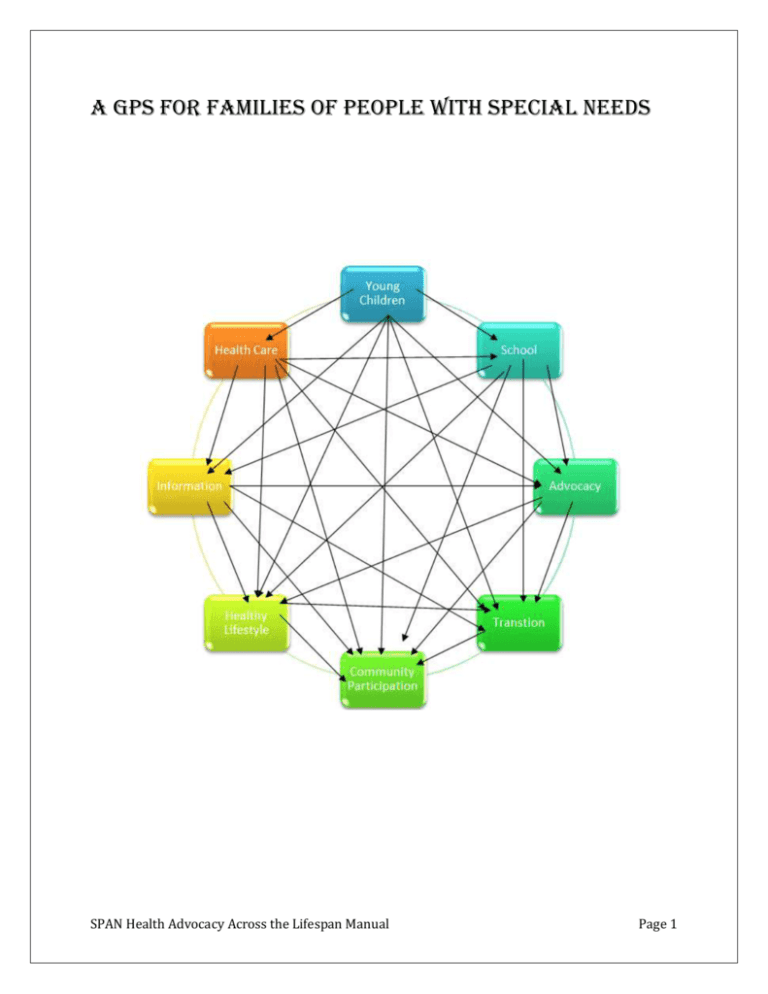
A GPS for Families of People with Special Needs
SPAN Health Advocacy Across the Lifespan Manual
Page 1
Introduction
I wrote this manual to help other families of individuals with special needs
and the professionals who work with them. My daughter now has 5 lifethreatening conditions, and autism just to keep things interesting. We have
been through everything from early intervention to currently going
through transition to adult care. I hope this helps you on your journey.
Lauren Agoratus
NJ Coordinator-Family Voices @ SPAN
SPAN Health Advocacy Across the Lifespan Manual
Page 2
Table of Contents
Introduction .................................................................................................................................................. 2
Early & Continuous Screening ....................................................................................................................... 5
Diagnosis ....................................................................................................................................................... 5
Early Intervention ......................................................................................................................................... 7
Child Care ...................................................................................................................................................... 7
Genetics & Rare Disorders ............................................................................................................................ 8
General Important Information .................................................................................................................... 8
Accessibility ................................................................................................................................................... 8
Advocacy ....................................................................................................................................................... 9
Stigma/People First Language .................................................................................................................... 10
Cultural Competence .................................................................................................................................. 11
Immigrant Issues ......................................................................................................................................... 11
Health Topics............................................................................................................................................... 12
Affordable Care Act.............................................................................................................................. 12
Dental care ............................................................................................................................................ 14
Emergencies ................................................................................................................................................ 15
Emergency care ................................................................................................................................... 15
Emergency Preparedness (Natural Disasters) ................................................................................ 15
Financial Help .............................................................................................................................................. 16
Financial Issues & Help ....................................................................................................................... 16
Financial Issues re: Insurance Plans/Appeals ................................................................................. 18
Health Information Privacy .................................................................................................................. 19
Hearing .................................................................................................................................................. 20
Hospitalization....................................................................................................................................... 20
Life Threatening Illness-Supports for Families ................................................................................ 21
Managed Care ...................................................................................................................................... 21
Medicaid ................................................................................................................................................ 23
Medicare (dual eligibles) ..................................................................................................................... 24
Prescriptions/Medication Management/Financial Help .................................................................. 25
Supplemental Security Income & Social Security Disability Insurance ....................................... 26
Title V ..................................................................................................................................................... 26
Transition (healthcare)................................................................................................................................ 27
Medical Systems ......................................................................................................................................... 29
Medical Appointments ......................................................................................................................... 29
SPAN Health Advocacy Across the Lifespan Manual
Page 3
Medical Decision-Making .................................................................................................................... 29
Medical Home ....................................................................................................................................... 30
Medical Records ................................................................................................................................... 32
Mental Health ........................................................................................................................................ 33
Wellness & Prevention................................................................................................................................ 34
Nutrition.................................................................................................................................................. 34
Physical Activity .................................................................................................................................... 35
Sexuality ................................................................................................................................................ 36
Vaccine Preventable Disease .................................................................................................................. 36
Vision Care ............................................................................................................................................ 37
Wellness-general.................................................................................................................................. 37
Miscellaneous ............................................................................................................................................. 38
Abuse/Trauma ...................................................................................................................................... 38
Alternative and Complementary Medicine........................................................................................ 39
General .................................................................................................................................................. 39
Quality Assurance in Health Care...................................................................................................... 40
Support: Individuals/Families ............................................................................................................ 41
Sample letters and forms ............................................................................................................................ 43
NJ FamilyCare Guidelines ............................................................................................................................ 60
What do the terms mean? .......................................................................................................................... 61
SPAN Health Advocacy Across the Lifespan Manual
Page 4
Early & Continuous Screening
Families may be concerned that their child isn’t doing what they should be by a certain age. One of the
Maternal and Child Health Bureau (MCHB) six core outcomes for children with special needs is, “Children
are screened early and continuously for special health care needs.” There are excellent checklists for
parents available from the Centers for Disease Control & Prevention “Act Early” at
http://www.cdc.gov/NCBDDD/actearly/milestones/index.html. Bright Futures, the American Academy of
Pediatrics’ health promotion website, has “What to Expect & When to Seek Help” at
http://www.brightfutures.org/tools/. Families should bring their concerns to their pediatrician as parents
are often the first to notice. Pediatricians also have screening tools that can help decide if more
evaluation is needed to make a diagnosis, or they may make a recommendation to a specialist. The
American Academy of Pediatrics (AAP) has recommendations for developmental screening at
http://www.aap.org/en-us/about-the-aap/Committees-Councils-Sections/Council-on-Children-withDisabilities/Pages/Description-and-Policy.aspx. If the pediatrician has a “wait and see” approach, the
family could continue to express their concern or perhaps request a referral. First Signs has tips on
having a discussion with the pediatrician at http://www.firstsigns.org/concerns/if.htm . Families can also
suggest to their pediatrician/family practitioner that they review the resources and recommendations
from the AAP including those found on the AAP’s National Center for Medical Home Implementation at
http://www.medicalhomeinfo.org/. This website includes a section on evidence-based guidelines and
screening resources at http://www.medicalhomeinfo.org/how/clinical_care/.
Diagnosis
Photo www.cdc.gov
When families are just getting a diagnosis, they need information on the condition and emotional
support. Exceptional Parent magazine has an annual resource guide that lists all the national
organizations for specific conditions at http://digital.turn-page.com/t/99327 (click on preview, then
archived.) For detailed information including research, databases, literature, etc., the Maternal & Child
Health Bureau (MCHB) has “Knowledge Paths” on some conditions at
http://www.mchlibrary.info/KnowledgePaths/index.html and resources for families at
www.mchlibrary.info/families/index.html. The National Dissemination Center for Children with
Disabilities information on specific disabilities can be found on the Parent Center Hub website at
http://www.parentcenterhub.org/repository/specific-disabilities/ or Spanish
http://www.parentcenterhub.org/repository/aprendizaje/. For emotional support, there are matching
groups like Parent-to-Parent and Friends Health Connection (see Support: Individuals/Families section.)
Other good resources on specific conditions are:
Health A-Z – Health Central
www.healthcentral.com
Health Conditions - WebMD
http://www.webmd.com/
SPAN Health Advocacy Across the Lifespan Manual
Page 5
Health Conditions & Diseases - Health Finder: U.S. Department of Health & Human
Services
http://www.healthfinder.gov/HealthTopics/Category/health-conditions-and-diseases
Spanish http://www.healthfinder.gov/espanol/ click on “Recursos de salud”
Health Issues: Conditions - American Academy of Pediatrics-information for families
http://www.healthychildren.org/English/health-issues/Pages/default.aspx
Spanish http://www.healthychildren.org/spanish/health-issues/paginas/default.aspx
Health Problems (click on Las Enfermedades) – Kids Health
English http://kidshealth.org/kid/health_problems/
Spanish http://kidshealth.org/kid/en_espanol/index.html?tracking=80002_F#cat20289
Health Topics – Medline Plus
www.nlm.nih.gov/medlineplus/healthtopics.html
Spanish http://www.nlm.nih.gov/medlineplus/spanish/healthtopics.html
Developmental Disabilities – Medline Plus
http://www.nlm.nih.gov/medlineplus/developmentaldisabilities.html
Disabilities - Medline Plus
http://www.nlm.nih.gov/medlineplus/disabilities.html
Explaining the Diagnosis/Self-Awareness
Families will often know when their child is ready to find out about their diagnosis because their child
starts asking questions. Children may ask, “Why I am I different,” or “Why is it so much harder for me to
do things?” Sometimes children may just want to know what something is called, other times they may
want their parents to explain what it means. Families can start with children’s books that explain certain
conditions. Children need to understand that they are not “better or worse,” simply different. They
should also explain that a diagnosis doesn’t define their life or their future. There is good information,
including explaining the diagnosis to the child, from Kids Health at http://kidshealth.org/parent/medical/ or
in Spanish at http://kidshealth.org/parent/en_espanol/index.html. Physical or visible disabilities can be
easier to explain and to understand for children (and even adults). Cognitive disabilities, autism
spectrum disorders, and learning disabilities may be more difficult to explain and understand. Families
may want to discuss their child’s condition privately until they are ready to understand. Once the child
is aware of their diagnosis, it’s easier to be more open. It’s almost like the “sex talk.” If parents pay
attention to their child, they will know that their child is ready. Families can figure out exactly what the
child is asking and how much they need to know. For older children there is a publication called
Accepting My Disability at http://www.going-to-college.org/myplace/disability.html.
Sometimes families think they are protecting their child by not telling them about their disability or
special healthcare needs. Unfortunately, this places their child at a disadvantage because they do not
learn how to understand their disability or advocate for the accommodations and supports that they
need. Explaining the diagnosis is one of the first steps toward building the self-awareness and skills
needed for independence.
SPAN Health Advocacy Across the Lifespan Manual
Page 6
Early Intervention
Photo-NICHCY.org
Early Intervention is a system that serves children from birth to three who have disabilities or
developmental delays. In NJ, there is a family “cost sharing” for services for families whose income is up
to 350% of the Federal Poverty Level (FPL). However, services that are at no cost to families include
Child Find (identifying and referring a child), Service Coordination (similar to case management),
Evaluation & Assessment, IFSP (Individualized Family Service Plan) Development and Review, and
Procedural Safeguards (e.g., parent consent, complaint resolution, etc.) The NJ Early Intervention
System (NJEIS) information can be found at www.state.nj.us/health/fhs/eis/index.shtml. There are also
“Regional Early Intervention Collaboratives” which are nonprofits that “plan and coordinate the state's
early intervention system at the regional/community level” and can be found at www.njeis.org/. The
National Dissemination Center for Children with Disabilities excellent overview of early intervention can
be found at the Parent Center Hub website at www.parentcenterhub.org/?s=early+intervention or
Spanish www.parentcenterhub.org/?s=intervencion+temprana.
Child Care
Photo-childandfamily-nj.org
Families of children with disabilities need to know that a child care provider can accommodate their
child appropriately. The Inclusive Child Care Project (NJICCP) works to increase inclusion of young
children with special needs in child care centers and other typical early childhood settings and can be
found at www.spanadvocacy.org/content/inclusive-child-care-project (English/Spanish). There are also
statewide resources listed by the Map to Inclusive Child Care Team at
www.state.nj.us/humanservices/clients/family/special/. For children who are medically fragile, NJ has
Pediatric Medical Daycare at http://web.doh.state.nj.us/apps2/healthfacilities/fsSearch.aspx. Families
can also add an Individual Health Plan to an IEP/504 plan that could include afterschool care at
www.spannj.org/Family2Family/individual_health_plan.htm. If the district runs an afterschool program,
they should accommodate children with special needs. Most families don’t know their child’s rights (for
example, they do not need to be potty trained) or the responsibilities of child care providers. There is an
excellent factsheet on what is legally required at
www.state.nj.us/humanservices/clients/family/special/10_ChildCare_NJLawAgainstDiscrimination_colu
mns%20.pdf.
SPAN Health Advocacy Across the Lifespan Manual
Page 7
Genetics & Rare Disorders
Photo-teachersnetwork.org
Learning about and understanding how genetics affects their child’s condition may help families feel as
if the child’s symptoms finally “have a name.” Genes in Life explains the basics of what genetics means
for families at http://genesinlife.org/genetics-101/why-learn-about-genetics. Another good resource is
the Genetic Alliance which has a variety of information including “Children and Youth with Special
Healthcare Needs in Healthy People 2020: A Consumer Perspective” at
www.geneticalliance.org/publications/healthypeople. If parents find out that their child has an unusual
condition, there is good information available from the National Institutes of Health at
http://rarediseases.info.nih.gov. There is also a searchable database available from the National
Organization for Rare Disorders at www.rarediseases.org/rare-disease-information/rare-diseases. For
chromosomal disorders, there are descriptions of genetic testing and conditions available from Unique
at www.rarechromo.org/html/ChromosomesAndDisorders.asp. There is even information on organ
transplants for children with developmental or other disabilities at
http://rwjms.rutgers.edu/boggscenter/products/documents/TransplantPampletFINAL6-11.pdf. If
families know ahead of time what to expect, they can take better care of their child, and the child will
reach their personal best potential.
General Important Information
Accessibility
Photo-Millikin.edu
After Medicaid managed care was mandated for the ABD (aged, blind, disabled) population in NJ,
accessibility became an issue. Patients with disabilities were not able to physically access doctor’s
offices whether it meant lacking wheelchair access ramps to get through the front door, assistive
devices to get on the exam table, etc. However, accessibility goes beyond the physical. For example,
there should be interpreters available when needed, whether it is for someone with a hearing
impairment or who speaks English as a Second Language (ESL). For more on interpretation, see also the
section on Cultural Competency. There is an excellent guide from the Office of Civil Rights called
“Access to Medical Care for Individuals with Mobility Disabilities” at
www.ada.gov/medcare_mobility_ta/medcare_ta.pdf. Beyond physical access, the Equal Rights Center
has a “Healthcare Accessibility Toolkit” at
www.equalrightscenter.org/site/DocServer/Accessible_Healthcare_toolkit.pdf?docID=2181. Families
need to know that accessibility is simply a civil rights issue.
SPAN Health Advocacy Across the Lifespan Manual
Page 8
Advocacy
Photo-sicklecellbodypolitics.wordpress.com
Beyond exercising their civil rights to access healthcare, families may need to further advocate for their
child as well as themselves. For example, they may need to insist on family support services to help
maintain their child at home. Family Support Services range from home or vehicle modification to
respite, which is a break for family caregivers from what could be 24 hour care. According to the
Caregiver Action Network, more people enter institutional care due to caregiver burnout than
deterioration of their condition. The “Health Care Advocacy Across the Lifespan” booklet by the
Statewide Parent Advocacy Network and Hinkle, Fingles & Prior Law Firm is a good starting point and
can be found at www.spanadvocacy.org/content/healthcare-advocacy-across-lifespan-what-parentschildren-disabilities-need-know. There are other advocacy tools throughout this manual in the
categories under which they fall.
Self-Advocacy in Healthcare
In addition to advocacy by families, children with special needs will learn how to advocate for
themselves. One of the easiest things families can do to foster self-advocacy is to give their child
choices. It can be something as simple as asking a toddler or preschooler which outfit they would like to
wear, or asking an older child if they would like to do math or spelling homework first. If a child doesn’t
have a choice regarding getting an injection or lab work, the family can
instead ask the child which arm they would prefer to have the work
done on. The Wyoming Council on Developmental Disabilities’ coloring
book for children can be found at
http://ddcouncil.state.wy.us/KidsCRSpring12.pdf. For older children
and self-advocates the National Gateway to Self-Determination has
"It’s My Future” at
http://ngsd.org/sites/default/files/its_my_future.pdf or the iPad app
www.ngsd.org/news/its-my-future-ipad-app. They also have “My
Health, My Choice, My Responsibility” which includes forms for health
information, health plans, and appointments as well as an iPad app at
www.ablelinktech.com/myhealth. The National Institute on Disability
autisticadvocacy.tumblr.com
and Rehabilitation Research has “This is Your Life! Creating Your SelfDirected Plan” which also includes mental health resources and is available at
http://www.ngsd.org/news/my-health-my-choice-my-responsibility-ipadapp.http://www.cmhsrp.uic.edu/download/sdlifeplan.pdf. Other relevant resources include:
SPAN Health Advocacy Across the Lifespan Manual
Page 9
Healthcare Frequently Asked Questions: Self Advocacy Series - Disability Rights NJ
http://www.drnj.org/pdf/drnj%20FAQs%20healthcare%20final%20version%20for%20web.pdf
Being a Healthy Adult: How to Advocate for your Health and Healthcare – Boggs Center on
Developmental Disabilities (NJ) in English and Spanish and read aloud, at
http://rwjms.rutgers.edu/boggscenter/products/BeingaHealthyAdultHowtoAdvocateforYourHe
althandHealthCare.html
My Health Passport - University of South Florida - AUCD
English http://flfcic.fmhi.usf.edu/docs/FCIC_Health_Passport_Form_Typeable_English.pdf or on
the SPAN website at www.spannj.org/cyshcn/core_outcome_6/Health_Passport_English.pdf
Spanish http://flfcic.fmhi.usf.edu/docs/FCIC_Health_Passport_Form_Typeable_Spanish.pdf or
on the SPAN website at www.spannj.org/cyshcn/core_outcome_6/Health_Passport_Spanish.pdf
Speak Up Guide University of Alaska - AUCD
www.uaa.alaska.edu/centerforhumandevelopment/selfdetermination/upload/Speak_Up_Guide
.pdf
Stigma/People First Language
In addition to cultural competency, there must be no stigma for physical and
mental health conditions. People first language means the person comes first,
then the description. It wouldn’t be said that someone is cancer, but rather that
they have cancer. The disease does not define the person. Further, biologically
based mental illness is just like any other physical condition. An individual with
diabetes would not be blamed for their illness or for the use of medication to
treat it. Mental illness is like any other illness except the organ affected just
Photot-peaceproject.com happens to be the brain, which symptoms manifest as behavior. There is an
appropriate way to talk with and about people with disabilities. For example, children with special
needs should think of themselves as “differently abled.” A variety of resources are listed below:
Disability Etiquette-United Spinal Association (various disabilities)
http://www.unitedspinal.org/pdf/DisabilityEtiquette.pdf
People First Language- Disability is Natural
English http://www.disabilityisnatural.com/images/PDF/pfl09.pdf
Spanish http://www.disabilityisnatural.com/images/PDF/pfl09spanish.pdf
People First Language - Self Advocates Becoming Empowered
http://www.aucd.org/docs/People%20First%20Language%20Manual.pdf
Stigma: Language Matters - MD Mental Hygiene Administration
http://www.onourownmd.org/wp-content/uploads/2011/12/LM-Flyer-Artwork207.pdf
Those of Us DisLabeled-(see Chapter 3)
http://www.hdi.uky.edu/Media/Default/Documents/DisLabeled.pdf
SPAN Health Advocacy Across the Lifespan Manual
Page 10
Cultural Competence
Photo-mocmhc.org
All families deserve to have healthcare access in a culturally competent manner. NJ was the first state
to require cultural competency training for health providers. The NJ Statewide Network for Cultural
Competence is at www.state.nj.us/njsncc/index.shtml or www.facebook.com/NJStatewideNetwork.
One of the key concepts of the medical home (also see section on Medical Home) is cultural
competence, which means that the “family’s culture and religious beliefs are recognized, valued, and
respected.” Cultural competency will help eliminate health disparities (which means that there are
worse outcomes including death), addressed in our blog at www.spanadvocacy.org/content/unfairaccess-healthcare-affects-our-families-lauren-agoratus. Family Voices national has information on
“Diversity & Cultural Competence” at www.familyvoices.org/work/diversity. The National Center for
Cultural Competence has “In Their Own Voices: Cultural Competence and Health Promotion” at
http://nccc.georgetown.edu/features/voices.html.
Immigrant Issues
Photo-ijpc-cincinnati.org
Closely related to cultural competency are immigrant issues. For example, many immigrant families may
not realize that some family members may be eligible for healthcare coverage even if others are not.
Research shows that uninsured families are diagnosed on average 2-4 years after their insured peers,
often when disease has progressed or even become fatal, which makes health insurance critical. For
information on how immigrant status affects eligibility for health plans in the Marketplace, see www.fvncfpp.org/blog/how-immigrant-status-affects-eligibility-health-plans-marketplace/. The National
Immigration Law Center has an excellent “Quick Guide to Immigrant Eligibility” for ACA (and other
national programs) at www.spanadvocacy.org/sites/g/files/g524681/f/files/imm-eligibility-quickguide2013-01-29_0.pdf.
SPAN Health Advocacy Across the Lifespan Manual
Page 11
Health Topics
Affordable Care Act
The Affordable Care Act (ACA) has several health care reform measures that help individuals with special
needs. Effective 9/23/10 new patient protections included:
No lifetime caps and limited annual caps (this means that there can no longer be a maximum
amount the insurance company will pay over the individual’s lifetime.)
No rescinding policies (this means that coverage can’t be dropped when someone gets sick.)
No pre-existing condition exclusions (this means that coverage can’t be denied for an individual
enrolling in the plan due to pre-existing conditions.)
Dependent coverage to age 26 (this means that all children, both with and without disabilities,
can be covered under their parent’s employer.)
Prevention with no cost share (this means that wellness benefits are provided with no additional
cost to families, see www.fv-impact.org/)
Plans will cover 10 “essential health benefits “including:
1. ambulatory patient services
2. emergency services
3. hospitalization
4. maternity and newborn care
5.
mental health and substance use disorder services, including behavioral health
6. prescription drugs
7.
rehabilitative and habilitative services and devices (such as physical/occupational/speech
therapy)
8. laboratory services
9.
preventive and wellness services and chronic disease management
10. pediatric services, including oral (dental) and vision care
SPAN Health Advocacy Across the Lifespan Manual
Page 12
*For different levels of plans, see www.healthcare.gov/choose-a-plan/plans-categories/. For New
Jersey’s essential health benefits, see www.cms.gov/cciio/resources/data-resources/downloads/newjersey-ehb-benchmark-plan.pdf.
If your state has better benefits than the federal law—such as dependent coverage, preexisting
condition coverage, or mental health parity—state law will still apply. Families of children with
disabilities should note that the Marketplace (“exchange”) will only select one plan. Families with
children who have special needs may be able to have private insurance as well as Medicaid and/or
Medicare. Also, most states have a “disabled adult dependent” form that allows families of children
with disabilities to keep their dependent covered as long as the parent is employed, regardless of the
age of the child (get the form from the insurance company or employer before the child turns 18.) Also,
even if a child didn’t previously qualify for Medicaid because of family income, at age 18 the child is
considered a “family of one” and may then be eligible. In addition, some children may be dually eligible
for Medicare, for example, those with kidney disease or whose parents retire. Parents need to be aware
that their child with special needs could have both public and private insurance through “coordination
of benefits” which means that the family would have less out of pocket expenses. A good resource on
comparing plans for people with disabilities is a fact sheet from the National Disability Navigator
Resource Collaborative at http://www.nationaldisabilitynavigator.org/ndnrc-materials/fact-sheets/factsheet-1/\ Please note: This information does not pertain to persons in New Jersey who are enrolled in
Medicaid/NJ FamilyCare because the health care benefits and coverage for Medicaid/NJ FamilyCare
enrollees are all standardized and there are no out-of-pocket expenses (as long as enrollees are using
providers in the network of their health plan).
Families can apply for coverage during open enrollment (or special enrollment if there are life changes
affecting insurance such as job loss) at the Marketplace (exchange) at www.healthcare.gov/ or Spanish
www.cuidadodesalud.gov/es/. Parents and self-advocates can see how healthcare reform has helped
other families in the Family Healthcare Story Book at
www.spannj.org/Family2Family/NJ_Family_Healthcare_Stories_REVISED.pdf. The most up-to-date
information on the ACA from the Georgetown Center for Children and Families can be found at
http://ccf.georgetown.edu/aca/. Check out the ongoing blog on the ACA which includes information on
people with disabilities, Medicaid expansion, finding providers before choosing a plan, mental health,
how immigrant status affects eligibility (e.g. children may be eligible even if their parents are not), and
more at www.fv-ncfpp.org/blog . Listen to SPAN’s recorded teleconference on the ACA at
www.spanadvocacy.org/content/aca-teleconference-recording-english.
*For information on help paying for costs, see https://www.healthcare.gov/lower-costs/qualifying-forlower-costs/. For help enrolling, call 1-800-318-2596, TTY: 1-855-889-4325 or find local help at
https://localhelp.healthcare.gov/.
SPAN Health Advocacy Across the Lifespan Manual
Page 13
Dental care
Photo Vanderbilt Kennedy Center “Oral Health Tips”
Dental care is an important component of
health care. Poor oral health can adversely affect overall physical health. Neglecting oral health can
lead to the development of infections and even death (see the story of a little boy who died of a
toothache (at www.hopefulparents.org/2014/02/the-little-boy-who-died-of-toothache.html.) The same
story by ABC News reported that by age 11, half of all children have dental decay. National Family
Voices’ blog, Why Oral Health Is Important for Children with Special Needs and How to Access It can be
found at http://www.fv-ncfpp.org/blog/why-oral-health-important-children-special-needs-how-accessit/.
The Marketplace of the Affordable Care Act also has dental coverage, either as part of Qualified Health
Plans, or “stand-alone” plans. Families can find out if dental benefits are included in their medical plan
at www.healthcare.gov/find-premium-estimates/. Parents and self-advocates can also get information
on available stand-alone dental plans at www.healthcare.gov/dental-plan-information/. Medicaid also
has dental coverage. The private plan would pay first, and Medicaid would cover the difference.
SPAN’s Healthcare Financing Fact Sheet Series has a fact sheet on Medicaid and oral health care at
http://www.spanadvocacy.org/sites/g/files/g524681/f/files/ISG_Healthcare_Financing_Factsheet_Serie
s_Updated_4-2013.pdf. If the family member is uninsured, Donated Dental Services provides free care
and can be found at http://dentallifeline.org/new-jersey/. If the individual needs braces, Smile for a
Lifetime has free orthodontics at http://slf.memberclicks.net/zip-code-search.
Bright Futures also has a guide on what families need to know about dental care at
www.mchoralhealth.org/pocket.html. The American Academy of Pediatrics has information for families
at English www.healthychildren.org/english/healthy-living/oral-health/Pages/default.aspx or Spanish
www.healthychildren.org/spanish/healthy-living/oral-health/paginas/default.aspx. Lastly, MCHC has a
“Knowledge Path” www.mchoralhealth.org/Topics/cshcn.html.
Dental health could also be affected by special needs. This could be due to the child’s poor motor skills
or sensitivity to touch. The Vanderbilt Kennedy Center has an excellent publication “Oral Health Tips” at
http://kc.vanderbilt.edu/kennedy_files/OralHealthTips.pdf. For individuals with developmental delays,
Autism Speaks has a “Dental Tool Kit” at www.autismspeaks.org/family-services/tool-kits/dental-toolkit. Dental health is an important part of overall health.
SPAN Health Advocacy Across the Lifespan Manual
Page 14
Emergencies
Emergency care
Photo www.nhpediatricems.org
Families of individuals with disabilities need to be prepared in an emergency. There are things families
can do ahead of time that will make it easier to get out the door quickly with everything they need. The
American Academy of Pediatrics and American College of Emergency Physicians has “Emergency
Information for children with special needs” at
www.acep.org/content.aspx?LinkIdentifier=id&id=26276&fid=896&Mo=No which has Emergency
Information Forms and a Children with Special Health Care Needs Fact Sheet. Another great resource is
Pack a “To Go” Kit available from Family Voices/ Family-to-Family New Hampshire at
http://nhfv.s481.sureserver.com/wp-content/uploads/2013/10/To_Go_Kit_brochure.pdf. Please also
see the Hospitalization section of this manual, which has tips whether the stay was planned or not.
Emergency Preparedness (Natural Disasters)
Hopefully this information won’t be needed but is good to know. The individual could wear a medical id
bracelet (caregivers can, too) and caregivers can also carry a paper copy of essential information in their
wallets. NJ also has two good forms which could be used as templates; the universal health record,
www.state.nj.us/health/forms/ch-14.pdf and the care plan for children with special needs,
www.state.nj.us/health/forms/ch-15.pdf. NJ also has a Special Needs Registry at
www13.state.nj.us/SpecialNeeds/. It’s also a good idea to register with the county Office of Emergency
Management at www.ready.nj.gov/about/association.html. The NJ Council on Developmental
Disabilities has information on emergency preparedness at www.njcdd.org/initiatives/emergencypreparedness/174-emergency-preparedness.
Photo www.ohsu.edu
SPAN Health Advocacy Across the Lifespan Manual
Page 15
In addition to actual health records, there are other things that caregivers of individuals with special
needs must consider. For example, if their medication is refrigerated or if the individual uses electrical
equipment, families may want to consider an emergency generator. Family Voices national has many
resources for emergency preparedness for both home and school, found at
http://www.familyvoices.org/work/caring?id=0004. There’s a useful publication, “Staying in Your Home
During Emergencies,” by the Wyoming Institute for Disabilities AUCD at
www.uwyo.edu/wind/_files/docs/utse_resources/guide_to_sheltering_in_place_4_18.pdf. Other
resources on emergency preparedness for individuals with special needs can be found at:
Emergency Management & People with Disabilities - West Virginia University-AUCD
http://wvats.cedwvu.org/emergencybrochure.php
Emergency Preparedness - Temple University AUCD Pennsylvania
http://disabilities.temple.edu/programs/eprep/
Emergency Preparedness for Children with Special Health Care Needs-Cincinnati
Children’s Hospital
www.cincinnatichildrens.org/patients/child/special-needs/home/emergencies/
(includes links for Families Planning for an Emergency, Supply Kit, and Child
Identification Products)
Financial Help
Financial Issues & Help
Families of children with special healthcare needs and individuals with disabilities have financial
burdens. According to Families USA, 60% of bankruptcies are caused by medical debt (see
http://familiesusa.org/sites/default/files/product_documents/medical-debt-fact-sheet.pdf.) The
Catalyst Center has a publication, “Breaking the Link Between Children’s Special Healthcare Needs &
Financial Hardship,” at www.hdwg.org/catalyst/breaking-the-link
There are things that families can do to avoid financial
difficulties. The NJ Community of Care Consortium developed
healthcare financing factsheets on topics such as
Medicaid/SCHIP, Federally Qualified Health Centers and hospital
charity care for the uninsured, etc. at
www.spannj.org/ISG_HealthcareFinancingFactSheetSeries.pdf or
www.spannj.org/cyshcn/core_outcome_3/Healthcare_Financing
_Factsheet_Series_-_SPANISH.pdf. There is also the National
Association of Free & Charitable Clinics at
http://www.nafcclinics.org/
SPAN also developed a factsheet “Economic & Health Resources
for Families” for necessities at
www.spanadvocacy.org/sites/g/files/g524681/f/files/Economic%
20%26%20Health%20resources_2012_0.pdf or Spanish
www.spanadvocacy.org/sites/g/files/g524681/f/files/Economic%
20%26%20Health%20resources%20Spanish_2012_0.pdf.
SPAN Health Advocacy Across the Lifespan Manual
Page 16
These resources help with everything from housing and utilities to eyeglasses, hearing aids, etc. NJ also
has the Catastrophic Illness in Children Relief Fund which reimburses families for related medical
expenses above 10% of household income in any 12-month period. These expenses can include
mileage/parking/tolls, phone calls to doctors, hotel stays during hospitalization, etc. The Fund also
covers medically necessary home modifications up to $25,000 for things like accessible bathrooms, grab
bars, etc. Families must be able to submit receipts and proof of payment. The application can be found
at www.state.nj.us/humanservices/cicrf/home/index.html. NJ has a referral line by calling 2-1-1 or going
to www.nj211.org/ or Spanish
http://translate.google.com/translate?u=http%3A//www.nj211.org/&hl=en&langpair=auto|es&tbb=1&i
e=utf-8 and putting in a search for a service like transportation. In addition, NJ Helps has an online
screening tool for possible benefits and links to online applications for things like food assistance,
heating help, etc. at www.njhelps.org/ or Spanish www.mynjhelps.com/.
Family leave also helps families stay financially stable while caring for their ill member. The
National Family Medical Leave Act is a federal law that provides up to 12 weeks of unpaid leave and
information is available at www.dol.gov/whd/fmla/index.htm. NJ was one of the first states to pass a
law providing paid family leave for up to 6 weeks and information is available at
http://lwd.state.nj.us/labor/fli/fliindex.html (for Spanish click on “language” top of page.) Financial
planning can also include things like special needs trusts so that the individual won’t lose eligibility for
future benefits.
Lastly, parents want to ensure that their child is as independent as possible as an adult, regardless of
disability. There are Centers for Independent Living that help students and self-advocates gain life skills,
postsecondary education, and employment. You can find your local CIL at www.njsilc.org/. Vocational
rehabilitation services can also help youth and young adults with disabilities gain skills for competitive
employment. (Please also see the section on Transition.)
Other resources to help families with finances are:
Financial toolkit - Caregiver Action Network
http://nfca.typepad.com/financial_planning
Healthcare Financing- Family-to-Family Georgia (Parent-to-Parent Georgia)
http://p2pga.org/images/stories/CMS_P2P_Health_care_Financing_Fact_sheet_Octob
er_8_2012.pdf
Help for the Costs of Raising a Child with Special Needs-Exceptional Parent magazine
www.spanadvocacy.org/content/help-costs-raising-child-special-needs
Possibilities: A Financial Resource Book for Parents of Children with Disabilities-PACER
Center
www.pacer.org/publications/possibilities/images/stories/contentpdfs/possibilities_full_
site/possibilities_full.pdf
SPAN Health Advocacy Across the Lifespan Manual
Page 17
Financial Issues re: Insurance Plans/Appeals
Closely related to financial burden is getting the most out of insurance coverage. Another of the MCHB
core outcomes is “families of CSHCN [Children with Special Health Care Needs] have adequate private
and/or public insurance to pay for the services they need.” Families need to know that they can use the
“disabled dependent” provision to continue insurance coverage for their child even past age 26 under
the ACA (and age 31 under NJ law), as long as the parent stays employed by the same company.
Children may be eligible for Medicaid, or if denied due to family income, families and self-advocates can
reapply at age 18 as a “family of one.” Also, children could be eligible for Medicare early due to kidney
disease or if their parent becomes disabled or dies. For more information, see the section on the
Affordable Care Act.
Most families don’t know that they can “appeal” if a claim is denied. They don’t have to take “no” for an
answer and even though only 1/3 of families appeal, half of the families that do appeal have the
decision reversed in their favor. Each type of insurance has their own process and timeline for appeals,
so families need to check their member handbook, but often a doctor’s note of medical necessity is all
that is needed. A good starting point is “Defining Medical Necessity” found at
www.jhsph.edu/research/centers-and-institutes/womens-and-childrens-health-policycenter/publications/cshcn-MedicalNecessity.pdf. Families should also send everything certified/return
receipt and keep copies. The NJ Department of Banking and Insurance has an appeal guide at
www.state.nj.us/dobi/division_consumers/insurance/appealcomplaintguide.pdf.
For families of individuals with developmental disabilities, the publication “Maximizing Coverage Under
NJ’s Autism and Other Developmental Disabilities Insurance Mandate” at
www.spannj.org/cyshcn/core_outcome_3/Maximizing%20Coverage%20ASD%20&%20Other%20DD.pdf
is very helpful. For people needing special dietary items not covered by insurance like food thickeners,
caloric supplements, etc. sometimes a company will give a 50% discount if you order from them
directly. Families can check with Special Child Health Services in their county for help funding these
items at www.state.nj.us/health/fhs/sch/sccase.shtml. For families of individuals with mental health
issues, federal and state mental health “parity” (equal coverage for physical and mental illness) will help
children get the most benefits. (See also the sections on the Affordable Care Act as well as Mental
Health.)
If families are fortunate enough to have multiple insurance plans, whether
it’s the parents’ coverage or a public/private combination, “coordination of
benefits” will help get the best coverage. This means that the primary plan
pays first and then the other insurance plan covers all or most of the rest.
However, families may need to let providers know to rebill. If families use
Medicaid to supplement a private insurance plan, even if the
doctor/medical provider doesn’t usually accept Medicaid, the billing
department can call the Medicaid HMO for the directions on how bill
Medicaid as “out of network.” If a provider doesn’t take Medicare, the
provider just needs to send his “Medicare opt out” with the bill using this
Photo blog.equifax.com
Medicare form in English or Spanish at www.cms.gov/Medicare/CMS-Forms/CMS-Forms/CMS-FormsItems/CMS012949.html. The NJ Department of Human Services has an excellent guide, “When You
Have Medicaid and Other Insurance,” available at
www.state.nj.us/humanservices/dmahs/home/Medicaid_TPL_Coverage_Guide.pdf.
SPAN Health Advocacy Across the Lifespan Manual
Page 18
Other resources to help families with insurance issues are:
Health Insurance Rights – Family Voices/ Family-to-Family Tennessee (Tennessee
Disability Coalition)
http://www.tndisability.org/tndisability/childrens-health-care
Help for Families with Health Insurance Issues - Family Matters-Family Voices national
http://www.thefamilymatterswebsite.org/PDF/GuideDealingwithInsuranceCo.pdf
Things to Consider When Evaluating a Health Insurance Plan-Family Voices/ Family-toFamily Alabama
http://www.familyvoicesal.org/documents/ThingstoConsiderwhenevaluatingahealthpla
nTipSheet.pdf
Understanding Your Health Care Insurance and Appeal Rights - Hinkle, Fingles, & Prior
Law Firm
http://www.hinkle1.com/pdf/health_care_rights.pdf
Children’s Specialized Hospital-Health Insurance Education
http://www.childrens-specialized.org/insurance-education
Health Information Privacy
The use of Health Information Technology (HIT) has many benefits, Photo www.bocatc.org
such as avoiding duplicative forms/tests, sharing information between providers, making appointments
online, e-prescribing, and preventing medical errors. Families need to know that they can “opt out” of
information sharing but that this may have consequences, such as not being able to access information
in an emergency when the patient can’t communicate. There are protections in place to prevent
unauthorized access to the private health information of individuals. The Health Insurance Portability
and Accountability Act (HIPAA) protects health records and can be found at http://www.dlcma.org/Resources/Health/HEA%2013%20HIPAA_healthrecords_HHS.pdf. The Office of Civil Rights has a
publication, “Your Health Information Privacy Rights,” at
www.hhs.gov/ocr/privacy/hipaa/understanding/consumers/consumer_rights.pdf or in
Spanish, www.hhs.gov/ocr/privacy/hipaa/understanding/consumers/privacy-rights-20130204-spn.pdf.
Most recently, Healthcare.gov posted tips on preventing fraud at www.healthcare.gov/how-can-iprotect-myself-from-fraud-in-the-health-insurance-marketplace/.
SPAN Health Advocacy Across the Lifespan Manual
Page 19
Hearing
Hearing, dental (see above), and vision care (also see section on Vision) are an
important component of overall health for growing children. Unfortunately,
sometimes hearing issues aren’t discovered quickly and can even be misinterpreted
as behavioral, affecting speech and academic development. Newborn screening,
including hearing screening, helps with early diagnosis. NJ has the Early Hearing
Detection & Intervention program and information for families is at
www.state.nj.us/health/fhs/ehdi/parentinfo.shtml. In the event that hearing loss is
confirmed, the U.S. Department of Education as an excellent publication “Opening
Doors: Technology and Communication Options for Children with Hearing Loss” at
Photo www.gahcd.org
www2.ed.gov/about/offices/list/osers/products/opening_doors/index.html or
Spanish www2.ed.gov/about/offices/list/osers/products/opening_doors/espanol.html. There is also
“Just in Time: Hearing-Related Resources for Families” at www.infanthearing.org/familysupport/just-intime-color.pdf. Parents can decide what works best for their child using technology such as cochlear
implants, sign language, lip-reading etc. Much like those with learning disabilities see LD as a “learning
difference” (i.e., the student can still learn although differently), the deaf community views deafness as
a difference rather than a disability. Early diagnosis and treatment will result in the best outcomes such
as speech and facilitate inclusion in the community.
Hospitalization
Families of individuals with disabilities may need to be prepared for hospital stays, either through
planned procedures or through the emergency room. Families who have a member with lifethreatening illness should be trained in First Aid/CPR and emergency medication administration,
sometimes known as “rescue meds” and to have them wherever the individual goes. Families need to
know how to care for the individual upon discharge from the hospital, when to call the doctor, and how
to tell if it’s an emergency that requires a call to 911. Family members may also need to monitor the
individual at night, even while asleep, and there are video/audio monitors as well as motion detectors
that are sensitive enough to hear breathing. Please also see the section Emergencies-Emergency Care
for more information.
Photo www.boston.com
There is information on preparing for a hospital stay, even if it is unplanned, such as having some items
pre-packed and lists to organize what is needed, at www.spannj.org/familywrap/SPANhospital_visit_factsheet-revised.pdf. There are also resources for when your child is already in the
SPAN Health Advocacy Across the Lifespan Manual
Page 20
hospital from the Caregiver Action Network (“When Your Loved One Is Hospitalized”) at
http://caregiveraction.org/_doc/pdf/WhenHospitalized.pdf.
Guidelines for a Hospital Stay from the National Transition of Care Coalition are found at
www.ntocc.org/portals/0/hospital_guide.pdf. There is also information on the transition “Hospital to
Home” from Families Together at http://familiestogetherinc.org/wpcontent/uploads/2011/07/Hosptial_to_Home_Final_July_2011.pdf or Spanish
http://familiestogetherinc.org/wp-content/uploads/2011/07/Hospital-to-Home-Spanish-1.pdf as well as
“Surviving a Hospital Stay…and After” at www.spannj.org/familywrap/SPAN-hospital_staypreparing_to_go_home-revised.pdf.
Life Threatening Illness-Supports for Families
Parents of children with life-threatening illness need even more support
(please also see the sections on Hospitalization and Emergencies).
Families will need to be trained in CPR and First Aid. They also need to
know when to call 911. Parents can find CPR and First Aid classes from
the American Heart Association at
www.heart.org/HEARTORG/CPRAndECC/FindaCourse/Find-aCourse_UCM_303220_SubHomePage.jsp. They can also find classes
from the American Red Cross at www.redcross.org/take-a-class or
Spanish http://www.redcross.org/cruz-roja/cursos. Families can also
check with hospitals, fitness/wellness centers, county colleges, and
Photo Chai Lifeline
evening adult classes. There is another organization called Chai Lifeline
whose motto is “Fighting Illness with Love.” Their resources include housing and meal support (kosher,
too), for the entire family during hospitalization and can be found at www.chailifeline.org. Lastly
information on end-of-life care, called hospice care, can be found from WebMD at
www.webmd.com/balance/tc/hospice-care-topic-overview, as well as the National Hospice and
Palliative Care Organization at www.nhpco.org/about/hospice-care.
Managed Care
Managed care is intended to be a system of health care delivery and financing which coordinates and
provides timely access to high-quality, medically-necessary health care services for its members in a
cost-effective manner. When it works well, managed care can provide a comprehensive approach to
providing and paying for quality medically needed services through either public or private insurance.
According to the Boggs Center, the “Hallmarks of Managed Care” are:
1.
Using specific providers (in the insurance company network)
2. Not relying on the emergency room for primary care services
3.
Authorizing of specialty care and referrals (a primary care physician such as a pediatrician or
family practitioner would do this)
SPAN Health Advocacy Across the Lifespan Manual
Page 21
Source: Boggs Center
A very important component of managed care is care management. This is mandated by NJ Medicaid
for all children with special health care needs and also available in most private insurance plans. In
Medicaid, the HMO will assign the child to a care manager. Under NJ Medicaid the care manager is
usually a nurse or social worker who is responsible to help coordinate the child’s care and is the first
person to contact with a question or concern about the child’s health coverage. Families should
request a care manager if they are not automatically assigned one.
Another important piece of managed care is for families to use emergency rooms only for emergencies.
Families can use the “prudent layperson” definition, which means if they as a non-medical layperson
think that the individual needs emergency care, then they can go to the E.R. Other resources include:
Your Guide for Making Managed Care Work for You – AUCD
www.aucd.org/docs/urc/TA%20Institute%202013/MedicaidManagedCareEnglishfinal20
11.pdf
Parents Partnering with Managed Care Plans - Family Voices national
http://www.familyvoices.org/admin/work_leadership/files/ParentsPartnering.pdf
Medicaid Managed Care Supplement (hard copy only) - Community Health Law Project
http://www.chlp.org/publications
To Your Health (hard copy only) - Community Health Law Project NJ
http://www.chlp.org/publications
SPAN Health Advocacy Across the Lifespan Manual
Page 22
Medicaid
Medicaid is a joint federal-state program which pays for health care
services for low income families with dependent children, senior citizens,
and people with disabilities, as well as some people who are medically
needy because their health expenses are high. Most of Medicaid in NJ is
now Medicaid managed care (see section on Managed Care). The Boggs
Center’s “Your Guide for Making Medicaid Managed Care Work for You”
can be found at
http://rwjms.rutgers.edu/boggscenter/products/documents/MedicaidManage
Photo www.yalescientific.org dCareEnglishfinal2011.pdf or
http://rwjms.rutgers.edu/boggscenter/products/documents/Medicaidmanagedcarespanishfinal2011.pdf.
An important part of Medicaid for children is EPSDT (Early Periodic Screening Diagnosis & Treatment)
http://mchb.hrsa.gov/epsdt/overview.html. The Maternal and Child Health Bureau defines it as:
Early
Identifying problems early, starting at birth
Periodic
Checking children's health at periodic, age-appropriate intervals
Screening
Doing physical, mental, developmental, dental, hearing, vision, and other screening
tests to detect potential problems
Diagnosis
Performing diagnostic tests to follow up when a risk is identified, and
Treatment
Treating the problems found.
Despite the stigma sometimes associated with Medicaid, EPSDT has better coverage for children than
most employer health plans.
In NJ, Medicaid and SCHIP (State Children’s Health Insurance Program) are together. Information on
Medicaid/SCHIP can be found under the Family Care Program. Various resources for New Jersey Family
Care include:
NJ FamilyCare factsheet- who is eligible/what is covered (bilingual)
www.njfamilycare.org/docs/facts_english.pdf
Healthy Facts at a Glance http://www.njfamilycare.org/docs/healthy_facts_english.pdf
or Spanish http://www.njfamilycare.org/docs/healthy_facts_spanish.pdf
Important News: Will Using Benefits Hurt my Changes of Getting a Green Card or
Becoming a U.S. Citizen? http://www.njfamilycare.org/docs/flyer_english.pdf or Spanish
http://www.njfamilycare.org/docs/flyer_spanish.pdf
General information on Medicaid and how it works can be found at
www.spannj.org/familywrap/medicaid_fact_sheets.htm or Spanish
www.spannj.org/publications/index.html#espanol. The Arc of NJ also has regular Medicaid updates on
their program Mainstreaming Medical Care at www.arcnj.org/programs/mainstreaming_medical.html
as well as their excellent newsletter Healthy Times at
www.arcnj.org/information/publications.html/title/healthy-times-.
SPAN Health Advocacy Across the Lifespan Manual
Page 23
Some families have had difficulties with the “Disabled Adult Child (DAC)” provision affecting Medicaid
eligibility. This means that if the child had SSI before but the parent becomes disabled, retires, or dies,
the child is a DAC and should maintain Medicaid eligibility. There are two good publications available
from the NJ Department of Human Services on this topic at
www.state.nj.us/humanservices/ddd/documents/Documents%20for%20Web/DisabledAdultChildren(D
AC).pdf and www.state.nj.us/humanservices/dmahs/info/resources/medicaid/2013/1303_Continued_Eligiblity_For_Disabled_Adult_Children_DAC.pdf.
Families can ask questions about their Medicaid benefits from their HMO member services or care
manager. NJ also has a Medicaid hotline at (800) 356-1561. If families still have concerns, they can
contact Medical Assistance Customer Centers in their county found at
www.state.nj.us/humanservices/dmahs/info/resources/macc/. The Kaiser Family Foundation has “A
Guide to the Medicaid Appeals Process” at
http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8287.pdf. If families haven’t been able to
resolve the issue using this process, they can fill out the Medicaid problem reporting form found at
www.spannj.org/medicalproblemreportingform.htm. The last resort is a Medicaid fair hearing and
there is a guide explaining the process from Family Connection, which, although not NJ specific, gives
tips on how to prepare at http://pandasc.org/wp-content/uploads/2012/01/Medicaid-Fair-Hearing.pdf
New developments in NJ Medicaid include the Comprehensive Medicaid Waiver and information is
available on forthcoming changes at www.state.nj.us/humanservices/dmahs/home/waiver.html.
Please note that effective 7/1/14, all Medicaid waivers transitioned to Medicaid Managed Long Term
Services and Supports found at www.state.nj.us/humanservices/dmahs/home/mltss.html. See also
SPAN’s factsheet at www.spanadvocacy.org/content/nj-medicaid-waivers-transition-managed-careeffective-7114.
Medicare (dual eligibles)
Photo www.Medicare.gov
In some circumstances, individuals with special health care needs may also be eligible for Medicare,
such as for dialysis or kidney transplant. When some children with disabilities become adults, they may
become dually eligible for both Medicaid and Medicare. The Social Security Administration has a
booklet “Benefits for Children with Disabilities www.ssa.gov/pubs/index.html.” A good resource for
families who have questions on Medicare is the State Health Insurance Program counselors at
www.state.nj.us/humanservices/doas/home/sashipsite.html.
SPAN Health Advocacy Across the Lifespan Manual
Page 24
Prescriptions/Medication Management/Financial Help
One of the main causes of treatment failure resulting in hospitalization for both physical and mental
health is medication error. Families may be told to increase or reduce the dosage of a medication they
already have on-hand, or to use a pill splitter. This may cause confusion because it is different from what
was on the bottle. Or the next time they pick up the medication, it might look different because it is a
generic instead of a brand name version. Each time they get a new medication, families should ask if it
will have a bad reaction when taken with any of the individual’s current medications. Families may even
need to get medications from a specialty pharmacy—sometimes called compounding pharmacy because
a special mixture is needed to create the medicine—though sometimes the hospital can give the
formula directly to a local pharmacy. Other times families may encounter issues if they are getting care
across state lines. In this case, even if they have an out-of-state authorization for medical care, they may
need to pay for medications up front and get reimbursed when they get home. Or they may have to get
a prescription or approval for use of home medication while in-patient if the family member is
hospitalized and the hospital doesn’t carry the medication in their “formulary” (list of drugs), though
some hospitals have pharmacies like CVS on the same campus in addition to their “in-house” pharmacy.
Organizing medicine will help avoid giving the wrong dose or at the wrong time or missing a dose. A
good free tool is MyMedSchedule at www.mymedschedule.com, which has a medication schedule, what
each one looks like, its use, and a checklist for filling the pill box. FDA has a form called My Medicine
Record at www.fda.gov/downloads/AboutFDA/ReportsManualsForms/Forms/UCM095018.pdf. Family
Voices/ Family-to-Family New Hampshire has a publication “Medical Prescription Tips” at www.fvncfpp.org/files/5813/0593/6859/Prescip_Tips.pdf. Please also see the diagram below on how to read a
prescription bottle label.
Photo www.merckengage.com
The challenge of paying for medications sometimes causes families to either skip doses or even take a
medicine from another family member, which can cause even more health problems. The first thing
families can do is make sure their insurance covers what it should and that both prescription plans are
billed (if there is more than one plan). There are organizations that help pay for medicine, especially for
those without insurance. The Partnership for Prescription Assistance will help families get free or low
cost medicine and information is available at www.pparx.org/en/prescription_assistance_programs or
Spanish www.pparx.org/es/prescription_assistance_programs_es. Pfizer Helpful Answers has a similar
program and does not limit families to only use Pfizer-brand prescriptions. The program can be found at
www.phahelps.com/pages/Find/FindAll.aspx or Spanish www.phahelps.com/pages/Find/FindAll_s.aspx.
SPAN Health Advocacy Across the Lifespan Manual
Page 25
Supplemental Security Income & Social Security Disability Insurance
Photo www.ssa.gov
According to the Social Security Administration (SSA), “Supplemental Security Income (SSI) program pays
benefits to disabled adults and children who have limited income and resources.” The SSA has a booklet
on this and other benefits at http://www.ssa.gov/pubs/index.html in English/Spanish (see Benefits for
Children with Disabilities.) It is important to note that if the child isn’t eligible for SSI due to family
income, at age 18 s/he can reapply as a “family of one.” In many states, SSI and Medicaid (see also
Medicaid section) are linked. Social Security Disability Insurance (SSDI) SSDI “pays benefits to you and
certain members of your family if you are ‘insured,’ meaning that you worked long enough and paid
Social Security taxes.” Children may get benefits if their parent becomes disabled. Young adults with
disabilities who have worked may be eligible for benefits under their own record. For more information
see http://www.ssa.gov/dibplan/index.htm or SPAN’s Healthcare Financing Fact Sheet series at
www.spanadvocacy.org/content/health-care-financing-factsheets-english and
www.spanadvocacy.org/content/healthcare-financing-factsheets-spanish.
Title V
Photo www.mchb.hrsa.gov
According to the Maternal & Child Health Bureau, Title V is a “Federal-State partnership” that
“acknowledges the uniqueness of each State and…maternal and child health program and the differing
needs of their individual populations.” NJ has county “case management units” that provide families of
children 0-21 find health resources and discounted medical supplies, as well as assist with early
intervention, Medicaid, SSI, and the Catastrophic Illness Relief Program application, including home
modification (see section on Financial Help.) They link families to charitable organizations that do fund
raisers for items like medical equipment (leg braces, wheelchairs, etc.). Families can find help in their
county at http://www.state.nj.us/health/fhs/sch/sccase.shtml. Family Voices national has a booklet for
families at http://www.familyvoices.org/work/title_v under “Title V Information System.” In NJ, Special
Child Health Services county case management units are found at
http://www.state.nj.us/health/fhs/sch/sccase.shtml.
SPAN Health Advocacy Across the Lifespan Manual
Page 26
Transition (healthcare)
Photo www.fvkasa.org
Transition to adult life for children with special needs is more than “school to work.” A big part of the
transition is changing to adult healthcare. A core Maternal & Child Health Bureau outcome is “Youth
with special health care needs receive the services necessary to make transitions to all aspects of adult
life, including adult health care, work, and independence.” But transition to adult life needs to start
when children are young and be reinforced throughout their lives. This can be done by beginning to give
the child choices and some control, even for something as simple as what to wear on a daily basis.
When the child has limited choice – for example, medical procedures like lab work –the child can choose
something simple, like which arm to use. Children need to learn to advocate for themselves to
maximize their independence. Families should try not to do everything for their child with special
needs, but also recognize the child may need more time to do things themselves. Even if the child may
not be completely independent as an adult, families can help ensure that their child can reach their
personal best potential, whatever that may be. Resources to help with health care transition include:
By Age
Being a Healthy Adult: How to Advocate for Your Health and Health Care- Boggs Center
http://rwjms.rutgers.edu/boggscenter/products/documents/TransitiontoAdultHealthca
re-EN-complete.pdf or Spanish
http://rwjms.rutgers.edu/boggscenter/products/documents/TransitiontoAdultHealthca
re-SP-complete.pdf
Going from Tween 2 Teen: It’s Time to Be More in Charge of Your Health (ages 12-14) –
http://here.doh.wa.gov/materials/tween-2-teen/13_CSHCN-12yr_E14L.pdf
Your Life, Your Health, Your Way: It’s Time to Be More in Charge of Your Health (ages
15-17) http://here.doh.wa.gov/materials/life-health-way/13_CSHCN-15yr_E14L.pdf
Your Future, Your Life (young adults) http://here.doh.wa.gov/materials/transition-planyoung-adults/13_CSHCN-18yr_E14L.pdf
Planning for a Healthy Transition: A Family Transition Plan – Washington Department of
Health http://here.doh.wa.gov/materials/healthy-transition-plan/13_CSHCNparent_E14L.pdf
Transition Resources: Health -Kentucky Cabinet for Health & Family Services
ages 12-14 http://chfs.ky.gov/ccshcn/transition12-14.htm
ages 15-17 http://chfs.ky.gov/ccshcn/transition15-17.htm
ages 18-21 http://chfs.ky.gov/ccshcn/transition18-21.htm
For Youth
Transition to Adult Life On-Line Resource Guide-Champions for Progress
www.spannj.org/transition/TransitionCD/
SPAN Health Advocacy Across the Lifespan Manual
Page 27
Transition Tip Sheets for Teens - Statewide Parent Advocacy Network
www.spannj.org/Family2Family/Healthcare_Transition_for_Teens_with_Special_Needs.
pdf or Spanish
www.spannj.org/Family2Family/Healthcare_Transition_Summary_for_Teens_Spanish.pdf
Healthcare Transition Resources for Youth & Families-Got Transition?
www.gottransition.org/youthfamilies/index.cfm
For Families
Transition Checklist for Parents - American Academy of Pediatrics (Illinois)
www.spanadvocacy.org/sites/g/files/g524681/f/files/CaregiverChecklist_RE_0.pdf
Healthcare Transition Resources-Got Transition
www.gottransition.org/resources/index.cfm
For Professionals
Transition Resources for Health Practitioners – Champions for Progress
www.spanadvocacy.org/sites/g/files/g524681/f/files/Transition%20Resources%20for%2
0Health%20Practitioners_0.pdf
Resources related to work, post-secondary education, and independence can be found at Healthy &
Ready to Work For Youth By Youth, www.syntiro.org/hrtw/youth/group_etc.html. There is also a
website on college, including accommodations, at Think College-College Options for People with
Intellectual Disabilities, www.thinkcollege.net/. There are work incentive programs which allow people
with disabilities to maintain their eligibility for benefits like Medicaid and SSI. The NJ Workability
Program describes how to maintain Medicaid eligibility and Discoverability (transportation) and can be
found at www.state.nj.us/humanservices/dds/projects/discoverability/. The Family Resource Network
has information on NJ Work Incentive Network Support at www.njwins.org/.
There are also general transition resources with good overviews of the entire process at:
Student Transition workbook-Statewide Parent Advocacy Network
www.spannj.org/pti/Workbook_English.pdf
Transition Toolkit Tab 2 Transition Planning – Colorado Department of Education
www.cde.state.co.us/sites/default/files/documents/cdesped/download/pdf/tk_transpla
n.pdf
Transition Toolkit-Health - Autism Speaks (good for all disabilities)
www.autismspeaks.org/sites/default/files/documents/transition/health.pdf
Family Voices national has Kids as Self Advocates (KASA), which is run by youth, at
http://fvkasa.org/resources/health.php or Spanish http://fvkasa.org/espanol.php. Centers for
Independent Living (CILs) help people with disabilities with activities of daily living and independent
living skills www.njsilc.org/. Area Agencies on Aging have now formed Aging and Disability Resource
Centers found in each county at www.state.nj.us/humanservices/doas/home/saaaa.html.
SPAN Health Advocacy Across the Lifespan Manual
Page 28
Medical Systems
Medical Appointments
Photo www.friendshipcircle.org
Families need to be organized to make the most out of doctor’s appointments. There are many
resources available to address issues such as preparing questions for doctors, coordinating specialists to
avoid multiple visits, and efficient use time with providers in the managed care system. One of the most
important things for families to know is what their child should be doing at a certain age. Bright Futures
has “encounter forms” by age for families at www.brightfutures.org/encounter/family/. Another good
resource is Handling Medical Appointments from Family Voices/ Family-to-Family New Hampshire at
http://nhfv.org/publication/tips-on-handling-medical-appointments/. Family Voices Wisconsin has
“Making the Most of Doctor’s Appointments” with tips on what do to before, during, and after the
appointment at http://fvofwi.org/wp-content/uploads/2012/01/Right-Doctor-fact-sheet-new1.pdf.
Families can find tips on preparing their child in the publication “Prepare Your Child for Doctor Visit”
from Parents Reaching Out at http://parentsreachingout.org/cd/pdfs_en/hc003.pdf or Spanish
http://parentsreachingout.org/cd/pdfs_es/hc003_es.pdf. Another issue facing families is special needs
transportation. Families can find information on what is available and how to address transportation
concerns from the NJ Council on Special Transportation at www.njcost.com/ or their local Center for
Independent Living found at www.njsilc.org. By having everything ready ahead of time, families and
their family member with special needs will get the best experience during their medical visit.
Medical Decision-Making
Photo www.aboutkidshealth.ca
Shared decision-making is one of the key concepts in healthcare. When patients partner with their
health providers, they get better outcomes. This is one of the key core outcomes of the Maternal &
Child Health Bureau, which states, “Families of children and youth with special health care needs
partner in decision making at all levels and are satisfied with the services they receive.” One of the main
ideas behind the medical home concept (see section on Medical Home also) is that care needs to be
patient and family centered. Children with special needs should have as much input as they can based
on age and ability (see also section on Transition.) Parents need to decide if and when their children are
SPAN Health Advocacy Across the Lifespan Manual
Page 29
capable of making medical decisions. The individual with disabilities should maximize their
independence, including medical decisions. One of the most difficult decisions for parents of children
with special needs is deciding how much they need to be involved in medical decisions as their child
grows older. Besides guardianship (which could also be limited), there are other tools such as power of
attorney that parents can use. Alternatives to guardianship resources can be found at:
Alternatives to Guardianship
http://ruralinstitute.umt.edu/images/archived_publications/Alternatives_To_Guardians
hip.pdf
Guardianship-Family Options (see Power of Attorney)
http://nj.gov/humanservices/ddd/services/guardianship/
Guardianship & Alternatives to Guardianship
www.ridlc.org/publications/RIDLC_Guardianship_Booklet.pdf
Guardianship and its Alternatives – (see Chapter 3)
http://mcdd.kennedykrieger.org/guardianship-and-its-alternatives-handbook-2011.pdf
Thinking About Guardianship?
www.gcdd.org/images/Reports/guardianship%20guide%20-%20gcdd.pdf
There is information on Palliative and End of Life Care: What is an Advance Directive (see Healthcare
Proxy) available at www.state.nj.us/health/advancedirective/whatis.shtml from the NJ Department of
Health. Lastly, but perhaps most importantly, there is a guide for self-advocates “Self Advocacy Guide to
Guardianship” (see chapter 2) from the Idaho Disability Rights available at
www.disabilityrightsidaho.org/images/content/docs/SelfAdvocacy%20Guide%20to%20Guardianships.pdf.
Medical Home
The medical home isn’t a physical place but the concept of having all of
a person’s medical care information together and having a primary care
provider coordinate all needed care, including primary care and
specialty care. This is especially important for individuals with complex
needs. The Primary Care Physician (PCP) has comprehensive
information on the child’s conditions and helps care run smoothly
across different settings and using specialists. The medical home care
is family-centered, continuous, comprehensive, coordinated,
compassionate, and culturally competent.
Family-centered care acknowledges that families are the primary
caregiver and support for individuals with special needs. Care is
continuous when there is the same PCP over time and there is also help
with transition to adult care. Comprehensive care covers both sick and
well care such as immunizations. Care is coordinated when families are
given community-based resources.
SPAN Health Advocacy Across the Lifespan Manual
Photo www.fmstudented.org
Page 30
Another of the six core outcomes for the MCHB is “Children and youth with special health care needs
receive coordinated ongoing comprehensive care within a medical home.” Compassionate care means
that concern for well-being of both the individual and family is demonstrated by providers. Culturally
competent care respects the diversity of families served (see also section on Cultural Competence.)
There are resources to help families understand and use the medical home concept (see section on
Medical Records for care plans).
General information on medical home:
Every Child Deserves a Medical Home
www.spannj.org/Family2Family/medicalhomeflyer.pdf
Medical Home
www.pacer.org/health/medicalhome.asp
Medical Home-Not Just a Place
www.gucchdgeorgetown.net/ucedd/documents/MedicalHome.pdf or Spanish
www.gucchdgeorgetown.net/ucedd/documents/3_spanish.pdf
Medical Home Fact Sheet - Family-to-Family Georgia (Parent-to-Parent of Georgia)
http://p2pga.org/images/stories/P2P_CMS_Medical_Home_Fact_Sheet_October_8_20
12.pdf
Your Medical Home
http://www.spannj.org/cyshcn/medical_home/MedicalHomeFamilyBrochure.pdf or
Spanish
www.spannj.org/cyshcn/core_outcome_2/MedicalHomeFamilyBrochureEspanol.pdf
Family-Centered Care
Family-Centered Care Self-Assessment Tool
www.familyvoices.org/admin/work_family_centered/files/fcca_FamilyTool.pdf
Families Partnering with Providers
Building a Partnership with Your Child’s Doctor
www.gucchdgeorgetown.net/ucedd/documents/BuildingPartnership.pdf or Spanish
www.gucchdgeorgetown.net/ucedd/documents/4_spanish.pdf
Healthcare Checklist (picking providers, preparing for appointments)
www.spanadvocacy.org/sites/g/files/g524681/f/files/Healthcare_Checklist_0.pdf
Partnering with Your Child’s Provider
www.familyvoices.org/admin/work_caring/files/partnering_providers.pdf
Partnering with Your Doctor
www.ncdhhs.gov/dph/wch/doc/providers/Partnering_with_Your_DoctorA_Medical_Home_Guide.pdf
SPAN Health Advocacy Across the Lifespan Manual
Page 31
Medical Records
Photo www.nymetroparents.com
Closely related to the medical home (see also Medical Home section) is the use of medical records to
keep track of care. Besides records kept by medical professionals, families can also keep track of the
most important information regarding their family member. Individuals with special needs could wear
medical ID bracelets and families can carry a sheet in their wallet with essential information such as
conditions, doctor contact information, medications/allergies etc. There is also a movement towards
electronic medical records, including medical id bracelets that connect to computers. Either way,
families can decide what works best for them.
A good starting point would be to look at the Universal Child Health Record at
www.state.nj.us/health/forms/ch-14.pdf as well as the Care Plan for Children with Special Health Care
Needs at www.state.nj.us/health/forms/ch-15.pdf. These forms simplify the child’s basic medical
information. The American Academy of Pediatrics also has “Build Your Own Care Notebook” for families
at www.medicalhomeinfo.org/for_families/care_notebook/care_notebook.aspx. This detailed
notebook has information on providers, insurance, appointments, hospitalization, immunizations,
medical bills, etc. Other good resources are:
Care Notebook -Exceptional Children’s Assistance Center
http://ecacparentcenter.org/userfiles/F2F/Care%20Notebook%20FINAL%20ss%2012.1.09.pdf or
Spanish http://ecac-parentcenter.org/userfiles/F2F/Care_Notebook_Spanish_Final_3-111.pdf
Care Notebook - Washington Department of Health
www.pluk.org/Pubs/CareNotebook_790k.pdf
Care Plans for Teens
http://cshcn.org/planning-record-keeping/care-plans-teens
Teen Care Notebook
http://cshcn.org/planning-record-keeping/teen-care-notebook
My Health Pocket Guide (for self-advocates)
www.waisman.wisc.edu/cedd/pdfs/products/health/PG.pdf
It’s also important for families to be aware of their rights – and their children’s rights – to privacy and
confidentiality regarding their medical records under HIPAA.
SPAN Health Advocacy Across the Lifespan Manual
Page 32
Mental Health
Mental Health is just as important as physical health. In recognition of this fact, the Affordable Care Act
strengthened access to mental health services. One of the ten Essential Health Benefits under the ACA
is coverage for “mental health and substance use disorder services, including behavioral health
treatment.” Increased access to behavioral health treatment may also make it easier to get coverage for
autism. Although NJ has an “autism and other developmental disabilities” mandate, it only applied to
25% of plans which were subject to state regulations. Federal mental health parity means that mental
health treatment must be equal to that for physical health. However, NJ already had mental health
parity that was even stronger than the federal law.
In dealing with mental health, families must try to avoid the stigma associated with mental illness. The
National Alliance on Mental Illness (NAMI) likens it to any other biologically-based illness except the
organ affected just happens to be the brain, and the symptoms manifest as behavior. Just as no one
would blame someone with diabetes who needed insulin, the same should be true for those who need
treatment for mental illness. Although the recent displays of school violence have opened the dialogue
on mental illness, research indicates that people with mental health issues are more like to be victims,
rather than perpetrators, of violence. NAMI also has workshops and classes for families dealing with
mental illness at www.naminj.org/programs/children-info-services/nami-basics/ or Spanish contact
Martha Silva at (888) 803-3413 or naminjenespanol@msn.com. Nationally NAMI has additional
resources from their Child & Adolescent Action Center at
www.nami.org/Template.cfm?Section=For_Parents,_Caregivers,_and_Youth&Template=/ContentMana
gement/ContentDisplay.cfm&ContentID=37809 or Spanish
www.nami.org/Template.cfm?Section=Child_and_Adolescent_Action_Center&template=/ContentMana
gement/ContentDisplay.cfm&ContentID=21090. They also have a family guide on how the primary care
provider (e.g. pediatrician) can address mental health at
www.nami.org/Content/ContentGroups/CAAC/FG-Integrating.pdf. In NJ, there are also Family Support
Organizations in each county have information and support for parents at http://njfamilyalliance.org/ or
for Spanish just click on translate. There is also the Children’s System of Care and an overview of
services, including emergency mobile response, which will go to where the child is located for crisis
stabilization is available at www.nj.gov/dcf/about/divisions/dcsc/. Performcare, the Contracted System
Administrator (gatekeeper) of the Children’s System of Care, has a “Youth & Family Guide” at
www.performcarenj.org/pdf/provider/youth-family-guide-eng.pdf or Spanish
www.performcarenj.org/pdf/provider/youth-family-guide-span.pdf.
Other good resources for families on what to look for and when to seek help:
Young Children
Center on the Social and Emotional Foundations for Early Learning-Family Tools
http://csefel.vanderbilt.edu/resources/family.html
First Steps: A guide for Parents of Young Children with Developmental Disabilities Chapters 1-4
(diagnosis based on age, parent feelings, definition of developmental disabilities,
individual/family adjustment)
SPAN Health Advocacy Across the Lifespan Manual
Page 33
English www.fddc.org/sites/default/files/file/publications/first_steps/FSSTEPSEngColor0105.pdf
Spanish www.fddc.org/sites/default/files/file/publications/first_steps/FSSTEPSSpaColor0105.pdf
All ages
A Family Guide to Children’s Mental Health Services and Supports - Florida Department of
Children and Families
www.dcf.state.fl.us/programs/samh/mentalhealth/docs/FamilyGuideBookDCF.pdf
Bright Futures in Practice (what to expect by age)
www.brightfutures.org/mentalhealth/pdf/tools.html
Emotional, Behavioral, and Mental Health Challenges in Children and AdolescentsMaternal/Child Health Knowledge Path - U.S. Department of Health and Human Services,
Health Resources and Services Administration, Maternal/Child Health Bureau
www.mchlibrary.org/KnowledgePaths/kp_Mental_Conditions.html
Family Guide to Systems of Care for Children with Mental Health Needs - English & Spanish
http://store.samhsa.gov/product/Family-Guide-to-Systems-of-Care-for-Children-With-MentalHealth-Needs-bilingual-English-Spanish-/SMA05-4054
Families of individuals with disabilities need to recognize when their family member, or even other
family members, need some support to address mental health and wellness.
Wellness & Prevention
Wellness and preventive care are especially important for people with special health care needs. So
often, the focus is on the person’s condition that typical measures such as lead screening,
immunizations, etc. could be forgotten. The Affordable Care Act has a prevention and wellness initiative
which means that these services are provided to families at no cost.
Nutrition
According to the Centers for Disease Control (CDC), 18% of children and 21% of teens are obese (not just
overweight.) Obesity causes children to develop “adult” diseases like diabetes, high blood pressure,
high cholesterol etc. The two most important factors in reducing obesity
are nutrition and activity (see also section on Physical Activity.) The CDC
has good information on nutrition for children at
www.cdc.gov/bam/nutrition/index.html or similar information in Spanish at
www.cdc.gov/spanish/especialesCDC/ObesidadNinos/ .
Wellness guidelines from Bright Futures have been endorsed by the
American Academy of Pediatrics (AAP). The nutrition guide is broken down
by age and explains ideas such as portion control. It also addresses related topics such as breastfeeding
and food allergies. The guide is available at www.brightfutures.org/nutrition/index.html. The AAP also
has nutrition information for families available at www.healthychildren.org/english/healthyPhoto abilitiesexpo.co m
SPAN Health Advocacy Across the Lifespan Manual
Page 34
living/nutrition/Pages/default.aspx or Spanish www.healthychildren.org/spanish/healthyliving/nutrition/paginas/default.aspx. This website has information on healthy snacks, food
substitutions, picky eaters, gluten free diets, etc. The AAP NJ Chapter has “Obesity Prevention
Resources for Parents” at www.aapnj.org/showcontent.aspx?MenuID=998 in English and Spanish. This
website also has tips by age, particularly for young children. Children who are overweight or obese are
more likely to grow up to be obese or overweight adults, so prevention is essential.
Physical Activity
Closely related to nutrition (see Nutrition section) and obesity prevention is physical activity. Physical
activity is essential for good health for all people with disabilities, regardless of ability. It is even more
important for children with special needs to start early as they may be more likely to have weight
problems, and there are ways to make activities accessible to them. There are resources on wellness
and prevention from Bright Futures, endorsed by the American Academy of Pediatrics (AAP). Bright
Futures has “Bright Futures in Practice: Physical Activity” available at
www.brightfutures.org/physicalactivity/about.htm. They have activities for children with and without
special healthcare needs and address topics such as asthma and preventing heat stroke/exhaustion, etc.
The AAP also has a fitness guide at www.healthychildren.org/english/healthyliving/fitness/Pages/default.aspx or Spanish www.healthychildren.org/spanish/healthyliving/fitness/paginas/default.aspx. This guide has ideas on making time for fitness, involving the whole
family, developing a fitness plan, and overcoming obstacles such as living in unsafe neighborhoods.
The U.S. Department of Health and Human Services has a special guide on physical activities for girls at
www.girlshealth.gov/fitness/index.html and www.girlshealth.gov/padres/forma_fisica/index.html
(Spanish) The Centers for Disease Control & Prevention has a program “Body & Mind: Physical Activity”
at www.cdc.gov/bam/activity/index.html and www.cdc.gov/spanish/hojas/actividad_fisica.html
(Spanish) designed for children to use for motivation. There is also a free online course on nutrition and
fitness, which is personalized to the individual called “14 Weeks to a Healthier You” from the National
Center on Health, Physical Activity, and Disability at www.ncpad.org/14weeks/. The National Center on
Health, Physical Activity, and Disability developed a guide “Discover Accessible Fitness” for wheelchair
users that can be found at www.nchpad.org/discoverfitness/index.html. In addition to the resources
above that include special needs, there are groups that work just with children with disabilities. There is
a listing of accessible playgrounds at www.accessibleplayground.net/united-states/new-jersey/. Other
organizations have peer buddies that mentor children and adults with special needs such as:
Little League Challenger Division
www.littleleague.org/media/challenger.htm
Miracle League
www.miracleleague.com/findaleaguestartone.
html
Special Olympics NJ
http://www.sonj.org/
Photo www.mychildwithoutlimits.org
SPAN Health Advocacy Across the Lifespan Manual
Page 35
Sexuality
Families need to remember that individuals with disabilities have the same sexuality feelings as
everyone else. Some children may need help in understanding what is happening to their bodies as they
grow up. The Vanderbilt Kennedy Center has guides for both boys and girls. One is “Healthy Bodies: A
Parent’s Guide on Puberty for Boys with Disabilities” and the other is “Healthy Bodies: A Parent’s Guide
on Puberty for Girls with Disabilities.” The University of Minnesota has a factsheet for families
“Promotion of Healthy Relationships and Sexuality for Individuals with Disabilities” at
http://lend.umn.edu/docs/LEND-FACT-sexuality.pdf. The University of South Florida’s “Sexuality and
Developmental Disabilities Across the Lifespan” is at
http://flfcic.fmhi.usf.edu/docs/Parent_LowRes_English.pdf or Spanish
http://flfcic.fmhi.usf.edu/docs/Parent_LowRes_Spanish.pdf. Dr. Peter Gerhardt, chair of the
Organization for Autism Research (OAR) has good information on adult issues, including sexuality, at
http://www.researchautism.org/.
There are also resources with a special focus on
women’s health, such as “Being a Healthy Woman” at
www.health.nsw.gov.au/pubs/2010/being_healthy_wo
man.html. Another excellent resource is “Let’s Talk
About Health” from The Arc of NJ’s Mainstreaming
Medical Care Project. There is a workbook and video
explaining exams available at
http://mainstreamingmedicalcare.org/ and click on
“Women’s Health Project” order form.
www.butterflywheel.com
Vaccine Preventable Disease
Families need to make sure that their children do not get illnesses that could be prevented by vaccines.
Some parents may think that because they themselves had some of these diseases as children, that it
won’t hurt their children to experience the same diseases. However, even chicken pox can have serious
consequences, including hospitalization and death. The American Academy of Pediatrics has a list of
recommended immunizations at www2.aap.org/immunization/izschedule.html. The AAP also has a
family page, including making educated decisions on vaccines and safety, at
www2.aap.org/immunization/families/families.html.
A Special Note about Flu Prevention
Families of individuals with disabilities need to know that some people are at
higher risk of flu complications. The Centers for Disease Control & Prevention has
“People at High Risk of Developing Flu–Related Complications:” available at
www.cdc.gov/flu/about/disease/high_risk.htm or Spanish
http://espanol.cdc.gov/enes/flu/about/disease/high_risk.htm. In addition, The
Arc national has information on “Steps You Can Take to Prevent the Flu” at
www.thearc.org/document.doc?id=4470.
Photo www.mybergen.com
SPAN Health Advocacy Across the Lifespan Manual
Page 36
Vision Care
Vision care is an essential component for overall
health. Children with poor eyesight may experience
headaches, or miss out academically in school. In NJ,
the Commission for the Blind & Visually Impaired of
the Department of Health does free screenings and
also works with schools on IEPs for low vision tools like
slantboards, etc. An overview is found at
www.state.nj.us/humanservices/cbvi/services/prevent
ion/screening/ and more information specifically
about services for children is available at
www.state.nj.us/humanservices/cbvi/services/services/.
Photo www.downsyndromedaily.com
Due to the importance of vision care to overall health, one of the 10 Essential Health Benefits under the
Affordable Care Act is pediatric vision care. NJ FamilyCare also covers eyeglasses. Some families may
still not have vision coverage, but there are programs that can help. These include:
New Eyes for the Needy - free vision care
http://neweyesfortheneedy.org/apply-for-assistance/
One Sight
http://onesight.org/news/events
Vision USA
www.aoafoundation.org/vision-usa/how-to-apply/
Wellness-general
There are other general resources on prevention and wellness that
are beneficial to families of children with special needs. For the
children themselves, Bright Futures has an activity book for
children available in English and Spanish at
http://brightfutures.aap.org/pdfs/BFActivityBook_L%200626.pdf?S
ite=nf.aap.org&WebKey=68530b27-2adb-43ae-9c872fa20cb86cae&url_keyword=Bright+Futures+Activity+Book. The
book has pages to color, information on nutrition and activities,
dental care, etc. Family Voices has “Family Matters: Promoting
Health & Wellness for Children with Special Health Care Needs
Family Booklet at
https://org2.salsalabs.com/o/6739/images/family_matters_book.p
df or Spanish at www.familyvoices.org/page?id=0005. This booklet
helps parents with nutrition, physical activity, and reducing “screen
time”—the time kids spend in front of computers, videogames, TV,
Photo www.brightfutures.aap.org
etc. For self-advocates, the Centers for Disease Control and
Prevention “People with Disabilities: Living Healthy” website, at www.cdc.gov/features/disabilities/,
discusses resources on healthy living for individuals with special needs.
SPAN Health Advocacy Across the Lifespan Manual
Page 37
Miscellaneous
Abuse/Trauma
Photo www.kidslinkcares.com
Children and adults with special needs are more likely to experience trauma and abuse. Resources for
support for families that are available include:
Domestic Violence
www.state.nj.us/dcf/women/resources/countyresourcesdv.html
Family Success Centers (crisis prevention)
www.state.nj.us/dcf/families/support/success/
Parents Anonymous (strengthening families)
www.pa-of-nj.org/
Institutional Abuse (restraints/aversives/seclusion)
www.state.nj.us/dcf/about/divisions/iaiu/
Building family skills and preventing crisis is the key to success. Also, getting help when needed is
essential for individuals with special needs.
SPAN Health Advocacy Across the Lifespan Manual
Page 38
Alternative and Complementary Medicine
Photo www.organicgardening.com
There are some other health related concerns for families of individuals with special needs. For
example, according to the National Institutes of Health, almost 12% of all children have been given an
alternative medicine product. For children with multiple medical conditions, the number is almost
double at close to 24%. Alternative medicine use for children with autism climbs to 40%
(www.healthline.com.) It is essential that families inform their healthcare providers of any therapies,
herbs, vitamins etc. they are using, as it may affect other health care such as prescription medication.
The U.S. Department of Health & Human Services, National Institutes of Health created the National
Center for Complementary and Alternative Medicine (NCCAM) to research which complementary
therapies are being proven effective. Here, families and professionals can research conditions, such as
allergies, or treatments, such as acupuncture. This information can be found at
http://nccam.nih.gov/health/atoz.htm. Although the Spanish version doesn’t have A-Z topics, they do
have guidelines “Are You Considering Complementary Medicine? at http://nccam.nih.gov/node/3858.
Family-to-Family Utah also has an excellent factsheet “Alternative Therapies” at
www.utahfamilyvoices.org.php5-5.dfw1-2.websitetestlink.com/wpcontent/uploads/2010/12/AlternativeTherapies.pdf.
General
There are various resources for families of individuals with special needs if they need more information
or assistance. Family-to-Family Health Information Centers can be found at
https://org2.salsalabs.com/o/6739/images/F2FBrochure_07-11-2011.pdf and Family Voices state
organizations are at www.familyvoices.org/admin/miscdocs/files/FV_Brochure_English.pdf or Spanish
www.familyvoices.org/admin/miscdocs/files/FV_Brochure_Spanish.pdf. These are non-profit
organizations run by families of children with special needs to help other parents. NJ was the first state
to have the Parent Training and Information Center(PTI), Family Voices/Family-to-Family Health
Information Center (FV/F2FHIC), and Parent-to-Parent (P2P)—in one location at the Statewide Parent
Advocacy Network(SPAN)—to have one-stop shopping for free help for parents in education (PTI),
Health (FV/F2F), and Support (P2P). The Family WRAP (Wisdom, Resources, Advocacy, Parent-to-Parent
support) information at www.spanadvocacy.org/content/family-wrap-project-care (for Spanish click on
“translate”) explains these projects with links to each. SPAN is also the home for the Integrated Systems
of Care for Children with Special Needs with more information at
www.spanadvocacy.org/content/integrated-systems-children-special-needs (for Spanish click on
translate.) Here families will find information on the Maternal & Child Health six core outcomes of
SPAN Health Advocacy Across the Lifespan Manual
Page 39
screening, medical home, community services, paying for care, transition to adult care, and family
involvement. Family Voices national also has “What Do Families Say About Health Care for Children with
Special Health Care Needs?” available at www.familyvoices.org/admin/miscdocs/files/National-Famrpt1.pdf or Spanish www.familyvoices.org/admin/miscdocs/files/National-Famrpt-Spanish-1.pdf.
The Waisman Center has an excellent publication “Finding Your Way A Navigation Guide for Wisconsin
Families Who Have Children and Youth with Special Health Care Needs and Disabilities” available at
www.waisman.wisc.edu/cedd/pdfs/products/community/FYW_e.pdf or Spanish
www.waisman.wisc.edu/cedd/pdfs/products/community/FYW_s.pdf. Another guide from Family
Connection is “Roadmap to Success” at www.familyconnectionsc.org/resource-roadmap.html . The
Wisconsin Council on Developmental Disabilities has a “Healthcare Toolkit” at www.wibpdd.org/publications/2010/Health%20Care%20Tool%20Kit%20Web.pdf . The National Arc has free
webinars “Health Meet” on various topics and they are also archived to access anytime at
www.thearc.org/page.aspx?pid=3686 . Lastly, the American Academy of Pediatrics has “Healthy
Children” which is their family website and includes resources for special needs. Topics such as what to
expect at what age, health conditions, and safety are on the site. It is available at
www.healthychildren.org or Spanish www.healthychildren.org/spanish/Paginas/default.aspx.
Quality Assurance in Health Care
An important component of health care for individuals
with special needs is access to quality care. Family
Voices/ Family-to-Family New Hampshire has a booklet
“Best Practices for Children and Youth with Special
Health Care Needs” at
http://nhfv.s481.sureserver.com/wpcontent/uploads/2013/07/best_practices.pdf. This
Photo www.childrenshealthfund.org
guide has information on family-centered care,
community based resources, medical home, and other important pieces of medical care that is of high
quality. New England SERVE has an extensive report “Enhancing Quality: Standards and Indicators of
Quality Care for Children with Special Health Care Needs.” This publication has information in addition
to family-centered care such as health provider characteristics and is found at
www.neserve.org/neserve/pdf/NES%20Publications/Enhancing_Quality.pdf. The National Association
for Healthcare Quality, www.nahq, has information about healthcare quality ,as does the Agency for
Healthcare Quality at http://www.ahrq.gov/. Families need to make sure that their family member with
special needs have high quality care for best outcomes.
SPAN Health Advocacy Across the Lifespan Manual
Page 40
Support: Individuals/Families
Lastly, but perhaps most importantly, is family support for families of individuals with special needs.
There are many different kinds of resources available to families. NJ is fortunate to now have a
Department of Children and Families. For information on developmental disabilities and/or mental
health for children, see www.state.nj.us/dcf/families/csc/. Please note that children should be
transitioned to adult services as needed. For individuals with developmental disabilities, the Division of
Developmental Disabilities is launching the new Supports Program and information can be found at
www.state.nj.us/humanservices/ddd/programs/supportsprgm.html.
There are disability resources that explain what is available to families throughout the individual’s
lifespan. The Division of Disability Services publishes an excellent guide” NJ Resources” annually and it’s
found at www.state.nj.us/humanservices/dds/documents/RD%2014_webqxd.pdf or Spanish (2013)
www.nj.gov/humanservices/dds/documents/RD13SpanishES.PDF. They also provide free help to
families at their hotline at (888)285-3036. The Family Support Center (FSC) publishes a similar guide
that goes into even more detail on explanations of programs. The FSC “Options Manual” is available at
http://njcaregivers.org/wp-content/uploads/2013/08/Options2010.pdf or Spanish www.fscnj.org/wpcontent/uploads/sites/4/2013/10/Options_Manual_Spanish.pdf. The FSC also has a searchable
database so families can look for resources like transportation etc. at
http://www4.irissoft.com/IFTWSQL4prod/show/home_show.aspx. They also have a hotline at (800)
FSC-NJ10.
Families of individuals with disabilities need to recognize that they have an extra role as caregiver. The
Caregiver Action Network has a Family Caregiver Toolbox found at
http://caregiveraction.org/resources/toolbox/. Here families can find information on communicating
with health professionals, how technology assists with caregiving, financial planning etc.
Sometimes parents just need to talk to another parent who has experienced similar issues. NJ Parentto-Parent matches trained volunteer parents to families of children with the same condition at
www.spanadvocacy.org/content/nj-statewide-parent-parent (for Spanish click on “translate”). Friends
Health Connection also matches people with the same condition, or their caregivers at
http://friendshealthconnection.org. They also have free webinars with experts and have an online
community. Some families prefer going to support groups to talk to other
families. The NJ Self Help Clearinghouse has information statewide at
www.njgroups.org/ or Spanish www.mededfund.org/NJgroups/CulturalLanguage.pdf.
Families need to remember that they are the best advocates for their family
member because they have a personal stake in the outcome and can teach
them to self-advocate. In addition, because parents are with their child with
special needs 24-7, they need to realize that they are the experts in their
child’s strengths, needs, and development!
Photo ww.dshs.state.tx.us
SPAN Health Advocacy Across the Lifespan Manual
Page 41
SPAN Health Advocacy Across the Lifespan Manual
Page 42
Sample letters and forms
a. Sample letters appealing denials of services
Source: www.healthlawadvocates.org/tools/documents/files/HLA-Guide-to-Appeals-2-1513.pdf pages 19-20
Sample Appeal Letter
(1) [Your Name]
[Address]
[Phone Number]
(2) Sent by Certified Mail
Return Receipt Requested
(3) [Date]
(4) [Insurer Name/Address]
(5) Patient Name:
Member Name (if different):
ID#:
Group (if through an employer or group):
Plan:
Provider:
Treatment:
Treatment Date:
To Whom It May Concern:
(6) I am appealing the denial of [name of treatment] dated [date of denial] for service
provided/requested on [date of service or authorization submission].
(7) The standard that is being applied to this treatment is [include the exact language from
the denial notice].
(8) I have included a copy of the denial.
(9) I believe this denial should be overturned for the following reasons [list each of the
reasons you meet the criteria, including, e.g., your medical needs, prior unsuccessful
treatments, expected result].
SPAN Health Advocacy Across the Lifespan Manual
Page 43
(10) I have enclosed a letter of support from my doctor that states [summarize the
information in the doctor’s letter].
(11) I have included the following medical records [list the copies of documents (not
originals) you are including].
(12) I have included a personal statement [if you are and briefly summarize it].
For the reasons outlined above, I request that the denial be reversed. Please do not hesitate
to call me if you require additional information or have any questions.
Sincerely,
Your Name/Signature
(13) Enclosures
SPAN Health Advocacy Across the Lifespan Manual
Page 44
b. Sample logs for communication with healthcare providers
Exceptional Children’s Assistance Center- Care notebook- page 10
http://ecac-parentcenter.org/userfiles/F2F/Care%20Notebook%20FINAL%20ss%2012.1.09.pdf
SPAN Health Advocacy Across the Lifespan Manual
Page 45
Exceptional Children’s Assistance Center- Libreata de Salud
Pagina 10
http://ecac-parentcenter.org/userfiles/F2F/Care_Notebook_Spanish_Final_3-1-11.pdf
SPAN Health Advocacy Across the Lifespan Manual
Page 46
c. Sample healthcare transition forms
For Families:
Transition Checklist for Caregivers –AAP Illinois (2 pages)
www.spanadvocacy.org/sites/g/files/g524681/f/files/CaregiverChecklist_RE_0.pdf
SPAN Health Advocacy Across the Lifespan Manual
Page 47
SPAN Health Advocacy Across the Lifespan Manual
Page 48
For Youth and Self-advocates
Got Transition
http://www.gottransition.org/UploadedFiles/Files/NHCTC_ReadinessYouthTool_06_Oct_20
11.pdf
SPAN Health Advocacy Across the Lifespan Manual
Page 49
d.
Sample consent to release information forms (to share health information with schools
and other providers)
Medical release form
American Academy of Family Physicians-Authorization Form
www.aafp.org/fpm/2003/0200/p29.html
Authorization form
Your Practice Name
Patient Authorization for Use and Disclosure of Protected Health Information
By signing, I authorize [Insert name of practice] to use and/or disclose certain protected health
information (PHI) about me to _________________________.
This authorization permits [Insert name of practice] to use and/or disclose the following
individually identifiable health information about me (specifically describe the information to be
used or disclosed, such as date(s) of services, type of services, level of detail to be released,
origin of information, etc.):
The information will be used or disclosed for the following purpose:
(If disclosure is requested by the patient, purpose may be listed as “at the request of the
individual.”)
The purpose(s) is/are provided so that I can make an informed decision whether to allow release
of the information. This authorization will expire on [enter date or defined event].
The Practice will ___ will not ___ receive payment or other remuneration from a third party in
exchange for using or disclosing the PHI.
I do not have to sign this authorization in order to receive treatment from [insert name of
practice]. In fact, I have the right to refuse to sign this authorization. When my information is
used or disclosed pursuant to this authorization, it may be subject to redisclosure by the recipient
and may no longer be protected by the federal HIPAA Privacy Rule. I have the right to revoke
this authorization in writing except to the extent that the practice has acted in reliance upon this
authorization. My written revocation must be submitted to the privacy officer at:
[Insert name and address of practice]
SPAN Health Advocacy Across the Lifespan Manual
Page 50
Signed by: ______________________________
Signature of Patient or Legal Guardian
_______________________________
Print Patient’s Name
_______________________
Relationship to Patient
______________________
Date
_______________________________
Print Name of Patient or Legal Guardian, if applicable
Patient/guardian must be provided with a signed copy of this authorization form.
Note: This document is a template only. It does not reflect the requirements of your state’s laws.
You should consult with advisors (e.g., your state or local medical or specialty society, or legal
or other counsel) familiar with your state’s privacy laws prior to using this document.
Copyright © 2002 Gates, Moore & Company. Used with permission. “The HIPAA Privacy Rule: Three Key
Forms.” Bush J. Family Practice Management. February 2003:29-33,
www.aafp.org/fpm/20030200/29theh.html.
Copyright © 2016 by the American Academy of Family Physicians. All rights reserved.
SPAN Health Advocacy Across the Lifespan Manual
Page 51
School release form
American Academy of Pediatrics-Clinical Topics-Confidentiality
HIPAA/FERPA Information Release Form 1
https://schoolhealthteams.aap.org/public/content.cfm?m=13&id=13&startRow=1&mm=0&
parentMenuID=0
__________________ School District
AUTHORIZATION FOR USE OR DISCLOSURE OF HEALTH INFORMATION TO AND
FROM SCHOOLS
Completion of this document authorizes the disclosure and/or use of individually identifiable
health information, as set forth below, consistent with federal laws (e.g., HIPAA) concerning
the privacy of such information. Failure to provide all information requested may invalidate
this authorization.
USE AND DISCLOSURE INFORMATION:
Patient/Student Name:
/
Last
First
MI
Date of
Birth
I, the undersigned, do hereby authorize (name of health care provider, health plan and/or
agency):
(1)
(2)
to provide health information from the above-named child’s medical record to and from:
School District to Which Disclosure Is Made
Address / City and State / Zip Code
Contact Person at School District
Area Code and Telephone Number
Disclosure of health information is required for the following purpose:
_____________________________
Requested information shall be limited to the following: All minimum necessary health
information; or
Disease-specific information as described:
________________________________________
DURATION:
SPAN Health Advocacy Across the Lifespan Manual
Page 52
This authorization shall become effective immediately and shall remain in effect until
_________ (enter date) or for one year from the date of signature, if no date entered.
RESTRICTIONS:
[California] law prohibits the Requestor from making further disclosure of my health
information unless the Requestor obtains another authorization form from me or unless
such disclosure is specifically required or permitted by law.
YOUR RIGHTS:
I understand that I have the following rights with respect to this Authorization: I may revoke
this Authorization at any time. My revocation must be in writing, signed by me or on my
behalf, and delivered to the health care agencies/persons listed above. My revocation will
be effective upon receipt but will not be effective to the extent that the Requestor or others
have acted in reliance to this Authorization.
RE-DISCLOSURE:
I understand that the Requestor (School District) will protect this information as prescribed
by the Family Educational Rights and Privacy Act (FERPA) and that the information
becomes part of the student’s educational record. The information will be shared with
individuals working at or with the School District for the purpose of providing safe,
appropriate, and least restrictive educational settings and school health services and
programs.
I have a right to receive a copy of this Authorization. Signing this Authorization may be
required in order for this student to obtain appropriate services in the educational setting.
APPROVAL:
Printed Name
Relationship to Patient/Student
Signature
Date
Area Code and Telephone
This form may be duplicated or changed to suit your needs and your patients’ needs.
SPAN Health Advocacy Across the Lifespan Manual
Page 53
e. Sample healthcare power of attorney forms
American Academy of Family Practitioners-Advance Directive/Power of Attorney Form
www.aafp.org/afp/1999/0201/p617.html
Please note: This information was current at the time of publication. But medical information is always
changing, and some information given here may be out of date. For regularly updated information on a
variety of health topics, please visit familydoctor.org, the AAFP patient education Web site.
Sample Advance Directive Form
Am Fam Physician. 1999 Feb 1;59(3):617-620.
This form is a combined durable power of attorney for health care and a living will (in some
jurisdictions). With this form, you can name someone to make medical decisions for you if in the
future you're unable to make those decisions yourself. You can also say what medical treatments
you want and what medical treatments you don't want if in the future you're unable to make your
wishes known.
Instructions
Read each section carefully. Before you fill out the form talk to the person you want to name, to
make sure that he/she understands your wishes and is willing to take the responsibility. Write
your initials in the blank spaces before the choices you want to make. Write your initials only
beside the choices you want under Parts 1, 2 and 3 of this form. Your advance directive should
be valid for whatever part(s) you fill in, as long as it is properly signed.
Add any special instructions in the blank spaces provided. You can write additional comments
on a separate sheet of paper, but you should write on this form that there are additional pages to
your advance directive. Sign the form and have it witnessed. Give copies to your doctor, your
nurse, the person you name to make your medical decisions for you, people in your family and
anyone else who might be involved in your care. Discuss your advance directive with them.
Understand that you may change or cancel this document at any time.
Definitions to Know
Advance directive—A written document (form) that tells what a person wants or doesn't want if
he/she in the future can't make his/her wishes known about medical treatment.
Artificial nutrition and hydration—When food and water are fed to a person through a tube.
Autopsy—An examination done on a dead body to find the cause of death.
Comfort care—Care that helps to keep a person comfortable but doesn't make him/her get well.
Bathing, turning and keeping a person's lips moist are types of comfort care.
SPAN Health Advocacy Across the Lifespan Manual
Page 54
CPR (cardiopulmonary resuscitation)—Treatment to try to restart a person's breathing or
heartbeat. CPR may be done by pushing on the chest, by putting a tube down the throat or by
other treatment.
Durable power of attorney for health care—An advance directive that names someone to make
medical decisions for a person if in the future he/she can't make his/her own medical decisions.
Life-sustaining treatment—Any medical treatment that is used to keep a person from dying. A
breathing machine, CPR, and artificial nutrition and hydration are examples of life-sustaining
treatments.
Living will—An advance directive that tells what medical treatment a person does or doesn't
want if he/she is not able to make his/her wishes known.
Organ and tissue donation—When a person permits his/her organs (such as the eyes or kidneys)
and other parts of the body (such as the skin) to be removed after death to be transplanted for use
by another person or to be used for experimental purposes.
Persistent vegetative state—When a person is unconscious with no hope of regaining
consciousness even with medical treatment. The body may move and the eyes may be open, but
as far as anyone can tell, the person can't think or respond.
Terminal condition—An ongoing condition caused by injury or illness that has no cure and from
which doctors expect the person to die even with medical treatment. Life-sustaining treatments
will only prolong the dying process if the person is suffering from a terminal condition.
Complete this portion of advance directive form
I, _____________________________________________________________, write this
document as a directive regarding my medical care.
In the following sections, put the initials of your name in the blank spaces by the choices you
want.
PART 1. My Durable Power of Attorney for Health Care
______ I appoint this person to make decisions about my medical care if there ever comes a time
when I cannot make those decisions myself. I want the person I have appointed, my doctors, my
family and others to be guided by the decisions I have made in the parts of the form that follow.
Name: ________________________________________________________________________
Home telephone: ____________________________ Work telephone: _____________________
Address:
________________________________________________________________________
________________________________________________________________________
If the person above cannot or will not make decisions for me, I appoint this person:
SPAN Health Advocacy Across the Lifespan Manual
Page 55
Name: ________________________________________________________________________
Home telephone: ___________________________ Work telephone: ______________________
Address:
________________________________________________________________________
________________________________________________________________________
______ I have not appointed anyone to make health care decisions for me in this or any other
document.
PART 2. My Living Will
These are my wishes for my future medical care if there ever comes a time when I can't make
these decisions for myself.
A. These are my wishes if I have a terminal condition
Life-sustaining treatments
_____ I do not want life-sustaining treatment (including CPR) started. If life-sustaining
treatments are started, I want them stopped.
_____ I want the life-sustaining treatments that my doctors think are best for me.
_____ Other wishes
_______________________________________________________________________
Artificial nutrition and hydration
_____ I do not want artificial nutrition and hydration started if they would be the main treatments
keeping me alive. If artificial nutrition and hydration are started, I want them stopped.
_____ I want artificial nutrition and hydration even if they are the main treatments keeping me
alive.
_____ Other wishes
_______________________________________________________________________
Comfort care
_____ I want to be kept as comfortable and free of pain as possible, even if such care prolongs
my dying or shortens my life.
_____ Other wishes
_______________________________________________________________________
B. These are my wishes if I am ever in a persistent vegetative
state
SPAN Health Advocacy Across the Lifespan Manual
Page 56
Life-sustaining treatments
_____ I do not want life-sustaining treatments (including CPR) started. If life-sustaining
treatments are started, I want them stopped.
_____ I want the life-sustaining treatments that my doctors think are best for me.
_____ Other wishes
_______________________________________________________________________
Artificial nutrition and hydration
_____ I do not want artificial nutrition and hydration started if they would be the main treatments
keeping me alive. If artificial nutrition and hydration are started, I want them stopped.
_____ I want artificial nutrition and hydration even if they are the main treatments keeping me
alive.
_____ Other wishes
_______________________________________________________________________
Comfort care
_____ I want to be kept as comfortable and free of pain as possible, even if such care prolongs
my dying or shortens my life.
_____ Other wishes
_______________________________________________________________________
C. Other directions
You have the right to be involved in all decisions about your medical care, even those not
dealing with terminal conditions or persistent vegetative states. If you have wishes not covered in
other parts of this document, please indicate them below.
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
SPAN Health Advocacy Across the Lifespan Manual
Page 57
PART 3. Other Wishes
A. Organ donation
_____ I do not wish to donate any of my organs or tissues.
_____ I want to donate all of my organs and tissues.
_____ I only want to donate these organs and tissues:
___________________________________________
_____ Other wishes
_______________________________________________________________________
B. Autopsy
_____ I do not want an autopsy.
_____ I agree to an autopsy if my doctors wish it.
_____ Other wishes
________________________________________________________________________
C. Other statements about your medical care
If you wish to say more about any of the choices you have made or if you have any other
statements to make about your medical care, you may do so on a separate piece of paper. If you
do so, put here the number of pages you are adding: _____________
PART 4. Signatures
You and two witnesses must sign this document before it will be legal.
A. Your signature
By my signature below, I show that I understand the purpose and the effect of this document.
Signature ____________________________________________ Date ____________________
Address
_____________________________________________________________________________
B. Your witnesses' signatures
I believe the person who has signed this advance directive to be of sound mind, that he/she
signed or acknowledged this advance directive in my presence and that he/she appears not to be
acting under pressure, duress, fraud or undue influence. I am not related to the person making
this advance directive by blood, marriage or adoption nor, to the best of my knowledge, am I
SPAN Health Advocacy Across the Lifespan Manual
Page 58
named in his/her will. I am not the person appointed in this advance directive. I am not a health
care provider or an employee of a health care provider who is now, or has been in the past,
responsible for the care of the person making this advance directive.
Witness #1
Signature _______________________________________ Date ____________________
Address
________________________________________________________________________
Witness #2
Signature ________________________________________ Date ___________________
Address
________________________________________________________________________
Adapted with permission from the District of Columbia Hospital Association, 1250 Eye, N.W.,
Suite 700, Washington, DC 20005; telephone: 202-682-1581; fax: 202-371-8151.
This handout is provided to you by your family doctor and the American Academy of Family
Physicians. Other health-related information is available from the AAFP online at
http://familydoctor.org.
This information provides a general overview and may not apply to everyone. Talk to your
family doctor to find out if this information applies to you and to get more information on this
subject.
Copyright © 1999 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the
material and may use that printout only for his or her personal, non-commercial reference. This
material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in
any medium, whether now known or later invented, except as authorized in writing by the
AAFP. Contact afpserv@aafp.org for copyright questions and/or permission requests.
SPAN Health Advocacy Across the Lifespan Manual
Page 59
NJ FamilyCare Guidelines
http://www.njfamilycare.org/income.aspx
SPAN Health Advocacy Across the Lifespan Manual
Page 60
What do the terms mean?
Accessibility
Removing barriers so people can get a service, participate in the community, etc.
Alternative Medicine
Care outside of traditional medical care.
Advocacy
Speaking on behalf of yourself or someone else so they get what they need.
Advance Directive
A person’s wishes for medical care, usually at the end of life.
Affordable Care Act (ACA)
Improving health care, covering more people, providing patient protections, and helping
with cost.
Appeal
Asking the insurance company to take a new look at a claim they turned down.
Care Coordination
All providers work together on a person’s health care needs.
Care Manager
Helps the person put together their health care services.
Caregiver
Someone who cares for another who can’t do everything him or herself.
Comprehensive Care
Supports the patient’s needs through their lifetime.
Coordination of Benefits
Figuring out who pays what when there is more than one insurance.
Cultural Competency
Understanding and respecting that people from other cultures may have different beliefs
toward health care, disability, etc.
Diagnosis
The name of the condition.
Disabled Adult Child (DAC)
Someone who is disabled before age 22 and has a parent that is disabled, retired, or
passed on.
SPAN Health Advocacy Across the Lifespan Manual
Page 61
Dual Eligible (in terms of health insurance coverage)
A person who can be on both Medicaid and Medicare.
Early Intervention
Services for children with special needs from birth to age 3, some of which are at no
cost to families.
Early Periodic Screening Diagnostic and Treatment (EPSDT)
Medicaid services for children to ensure children get what they need.
Emergency Preparedness
Being ready in case of natural disaster.
Essential Health Benefits (EHB)
10 services under the ACA that must be covered by health plans.
Family-Centered
Families and professionals are partners in care. The knowledge and wishes of families
are respected by professionals.
Family-to-Family Health Information Center/Family Voices
Help families of children with special needs find services.
Family Support
Services to help parents of children with special needs.
Genetics
How parents may pass on conditions to their child.
Guardianship
Taking charge of someone’s life when they are an adult.
Health Insurance Portability and Accountability Act (HIPAA)
Keeps the person’s health information private.
Health Information Technology
How details on a person’s condition is stored (usually on a computer.)
Health Maintenance Organization (HMO)
A type of plan under managed care.
Managed Care
Patients can only visit certain providers in the “network” and their doctor needs to give
the ok to see other doctors.
SPAN Health Advocacy Across the Lifespan Manual
Page 62
Medicaid
Public insurance that covers people with low income or disabilities
Medical Home
An idea where the team of doctors work together for best care.
Medicare
Public insurance that covers people over 65 or with certain disabilities.
Network
Doctors, drugstores, and hospitals covered by an insurance plan.
People First Language
Recognizing that people with disabilities are people first and not their disability.
Power of Attorney
Another person’s authority to decide on care for an adult.
Prescription
Medicine authorized by a doctor.
Preventive care
Wellness care to prevent disease.
Primary Care Provider (PCP)
The main doctor the person uses.
Quality Assurance
Making sure care is of good value.
Referral
The Primary Care Provider gives the ok to see another doctor or service.
Regional Early Intervention Collaboratives
Help families of children from birth to age 3 with early intervention in New Jersey.
Screening
Tests to decide if the child is at risk; screening is not a diagnosis.
Self Advocacy
Speaking up for yourself and having control.
Shared Decision-Making
The family and doctor decide together on choices for care.
SPAN Health Advocacy Across the Lifespan Manual
Page 63
State Children’s Health Insurance Program (SCHIP)
Medicaid plan for children.
Stigma
Negative, untrue, and unfair beliefs about a condition, a disability, etc.
Supplemental Security Income
Money for children with disabilities based on family income (family income no longer
counts as the person’s income at age 18.)
Title V
Programs for mothers and children with special needs.
Transition (health)
Changing from child to adult health care.
Vaccine preventable disease
Shots to avoid illness.
SPAN Health Advocacy Across the Lifespan Manual
Page 64