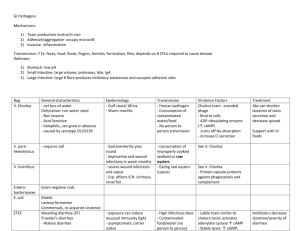
Bacillus food poisoning
advertisement

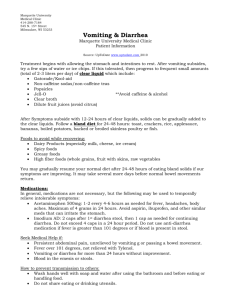
FOOD POISONING & DIARRHEA • Describe the terms diarrhea, dysentery and food poisoning • Discuss in detail about microorganisms causing diarrhea and dysentery • Identify the common microbial causes of food poisoning. • Discuss the laboratory diagnosis Definition • Food poisoning • Any illness resulting from the consumption of food • There are two types of food poisoning: food infection and food intoxication. 1) Food infection refers to the presence of bacteria or other microbes which infect the body after consumption. 2) Food intoxication refers to the ingestion of toxins contained within the food, including bacterially produced exotoxins, which can happen even when the microbe that produced the toxin is no longer present or able to cause infection • Diarrhea • Increase in water content, volume, or frequency of stools • Dysentery • Dysentery is an inflammation of the intestine causing diarrhea with blood Microorganisms causing diarrhea BACRTERIA 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Salmonella(GNR) Vibrio(GNR) Clostridium perfringens(GPR) Clostridium difficile(GPR) Campylobacter(GNR) Enterotoxigenic E.coli(GNR) Enterohemorrhagic E.coli Enteropathogenic E.coli Yersinia enterocolitica (GNR) Bacillus (GPR) Parasites 1. 2. 3. 4. 5. Giardia lamblia(cysts and trophozoite) Cryptosporidium(oocysts) Ankylostoma duodenale(eggs) Enterobius vermicularis Taenia saginata viruses 1. Rotavirus 2. Adenovirus 3. Norwalk virus fungi candida Dysentery • Ameabic dysentery • Entameaba histolytica • Bacillary dysentery • Shigella • Enteroinvasive E coli Mechanism of diarrhea and dysentery • Noninflammatory/secretory • Clinical manifestation • Diarrhea - watery to loose, ± nausea/vomiting/abd pain • Mechanism: • Preformed toxin, enterotoxin • Inflammation & invasion • Clinical manifestation • Diarrhea/dysentery – mucoid or bloody, fever, tenesmus, ± abd pain • Mechanism: • Cytotoxin, cellular invasion Salmonella • Member of Enterobacteriacae • Morphology :Gram negative bacilli, motile with peritrichous flagella • Non lactose fermenter, form acid and gas from sugar fermentation • Produce H2S • Classification: into two species 1. Salmonella enterica (5 subspecies) 2. Salmonella bongori • Human infections are caused by subspecies I strains(Salmonella enterica subspecies enterica) • Salmonella enterica subspecies enterica serotype Typhimurium can be shortened as S typhimurium • S typhi, S paratyphi A & B, S cholerasuis are primarily infective to humans Salmonella: laboratory diagnosis • Specimen: blood, bone marrow, urine and stool • Culture on 1. differential media: Mac conkey ,DCA, -non lactose fermenter 2. Selective media: salmonella shigella agar (SS agar), XLD agar 3. Enrichment media for stool: selenite F broth, tetrathionate broth-after 1-2 days this is plated on differential and selective media 4. Final identification: biochemical and slide agglutination tests with specific sera • Serology : 1. Agglutination with sera 2. Widal test(tube dilution agglutination test) Non typhoidal salmonellae infections • Salmonellae • NTS can be acquired from multiple animal reservoirs. Transmission is most commonly associated with animal food products, especially eggs, poultry, undercooked ground meat, and dairy products and fresh produce contaminated with animal waste. Mechanism of NTS food poisoning • NTS gastroenteritis is characterized by massive neutrophil (PMN) infiltration into both the large- and small-bowel mucosa. The degranulation and release of toxic substances by neutrophils may result in damage to the intestinal mucosa, causing the inflammatory diarrhea • occur 6–48 h after the ingestion of contaminated food or water. • Fever, Nausea, vomiting, and diarrhea and abdominal cramping • Dysentery may occur. • Usually self-limited and resolves within 3–7 days Vibrio cholera • The disease called cholera • Once in the human small bowel, the organism produces a powerful exotoxin called cholera toxin • Cholera toxin consists of two parts (A subunit) and a (B subunit). The B subunit binds to GM1 receptor on intestinal cells and delivers the A subunit inside the cell. The A subunit increases the intracellular levels of cyclic AMP. The, cAMP inhibits the sodium transport system in villus cells and activates chloride secretion, and thus causing accumulation of sodium chloride in the intestinal lumen. Water moves passively from the cell into the lumen by osmosis. Watery diarrhea results Clinical features of cholera • 24- to 48-h incubation period • Sudden onset of painless watery diarrhea that may quickly become voluminous • vomiting • Fever is usually absent • The stool has a characteristic appearance: , slightly cloudy fluid with flecks of mucus, no blood, and a somewhat sweet, inoffensive odor. It has been called "rice-water" stool because of its resemblance to the water in which rice has been washed Complications of cholera • Dehydration follows quickly due to fluid and electrolyte loss hypovolemic shock and death ensues. Signs of dehydration • • • • Intense thirst Loss of skin turgor Sunken eyes Week pulse • Renal failure due to acute tubular necrosis Shigella • Gram negative bacilli • Shigella as the etiologic agent of dysentery—a clinical syndrome of fever, and bloody stools • Shigella species are classified by four serogroups: • S. dysenteriae • S. flexneri • S. boydii • S. sonnei • Bacteria are transmitted most efficiently by the fecaloral route. • Most cases of shigellosis are caused by person-toperson transmission, although some outbreaks reflect contamination of water or food. • Shigella can also be transmitted by flies • A very few organisms are required for infection [103 organisms]. Pathogenesis of shigellosis • Invasion and inflammation: • Shigella invade colonic epithelial cells; followed by intracellular multiplication, spread of bacteria to adjacent cells, recruitment of inflammatory cells, and in the process destruction of colonic mucosa • Shiga toxin produced by S. dysenteriae type 1 • Inhibit cell protein biosynthesis and cell death Bacillary dysentery(shigella) • The incubation period usually lasts 1–4 days • Typical manifestations are • Initial watery diarrhea • vomiting • dysentery—a clinical syndrome of fever, abdominal cramps and frequent passage of small bloody stools • tenesmus Hemolytic uremic syndrome • The shiga toxin enters the systemic circulation where it is attached to (strong) Gb3 receptors on vascular endothelium . Toxins move into the cell,and shut down protein synthesis, resulting in cell death. Injury activates blood platelets and clot formation (thrombocytopenia) • The red blood cells are damaged(hemolysis) as the cells attempt to pass through partially obstructed microvessels. • Kidney failure occurs because of high distribution of microvasculature and Gb3 receptors. Pathogenic Escherichia coli ETEC - Enterotoxigenic • Enterotoxin (similar to cholera toxin), elaborated locally • Non-inflammatory: watery diarrhea known as travellers diarrhea EPEC- Enteropathogenic • EPEC causes diarrheal disease primarily in young children, including neonates • responsible for outbreaks of infantile diarrheas • The actual mechanism of diarrhea production is not known EHEC - Enterohemorrhagic / STEC • Cytotoxin (Shiga toxin), can cause hemolytic-uremic syndrome • Inflammatory: bloody diarrhea without fever EIEC - Enteroinvasive • Invasion • Dysentery: fever, abdominal pain, tenesmus, bloody or mucoid stool Campylobacter • Campylobacters are motile, curved, gramnegative rods • Campylobacters are found in the gastrointestinal tract of many animals used for food (including poultry, cattle, sheep, and swine) and many household pets (including birds, dogs, and cats). • These microorganisms usually do not cause illness in their animal hosts • The invasion of the intestinal cells is the main pathogenic mechanism • Clinical manifestations are acute onset of crampy abdominal pain, profuse diarrhea that may be grossly bloody, headache, malaise, and fever Amoeabic dysentery • Entameaba histolytica • Protozoa • Feco-oral transmission • PATHOGENICITY • Exist in two forms • Cyst is the infective form that is ingeted • Inside gut cyst changes to Trophozoite that are the active form that attach to the large gutInvadeflask shape ulcers • Acute-Extreme abd tenderness, dysentery, dehydration, Diarrhoea, abd cramps, vomiting, tenesmus • Liver abcess • Lab diagnosis • Trophozoites with pseudopodal movement in stool • Cysts in stool • Treatment • Metronidazole Staphylococcus food poisoning • S. aureus may harbor up to 15 enterotoxins, (staphylococcal enterotoxin A [SEA], B, Cn, D, E, G, H, I, J, K, L, M, N, O) • S. aureus food poisoning follows ingestion of preformed toxins that have been released into food or beverages. The toxins are heat stable and thus are not denatured by cooking. The disease typically starts 2 to 6 hours after ingestion with general malaise, nausea, vomiting, abdominal pain, and diarrhea but no fever. • Implicated foods are usually dairy, meat, bakery products Bacillus food poisoning • Bacillus cereus • Gram positive spore producing rod • Bacillus foodborne illnesses occur due to survival of the bacterial endospores when food is improperly cooked at less than or equal to 100°C allow some spores to survive. The food is then not refrigerated, allowing the spores to germinate. Germination and growth generally occur between 10°C and 50°C • Bacteria produces 2 types of toxins • The emetic toxin, called cereulide, which is highly heat resistant. This causes nausea and vomiting 16 hours after consumption • Diarrheal toxin causes diarrhea and abdominal pain 8-16 hrs after consumption Lab diagnosis • Culture • Stool • Vomitus • Left over food • Staphlocoocus enterotoxin detection Treatment(diarrhea) • Rehydration • Very important to replace fluid and electrolytes • Monitor blood pressure • Antibiotics • Not all pts require antibiotic therapy • Indications for therapy include high fever, bloody diarrhea, severe diarrhea, persistence for >1 week, and worsening of symptoms MYCOTIC POISONING • Many fungi form poisonous substances • It is of 2 types: 1. Mycetism in which a fungus which is eaten for itself causes toxic effects 2. Mycotoxicosis :in which fungal toxins contaminate some article of food • The best known mycotoxin is Aflatoxin produced by Aspergillus flavus present in foods like groundnuts, corn, peas, mushrooms