CH14 Practice Questions
advertisement
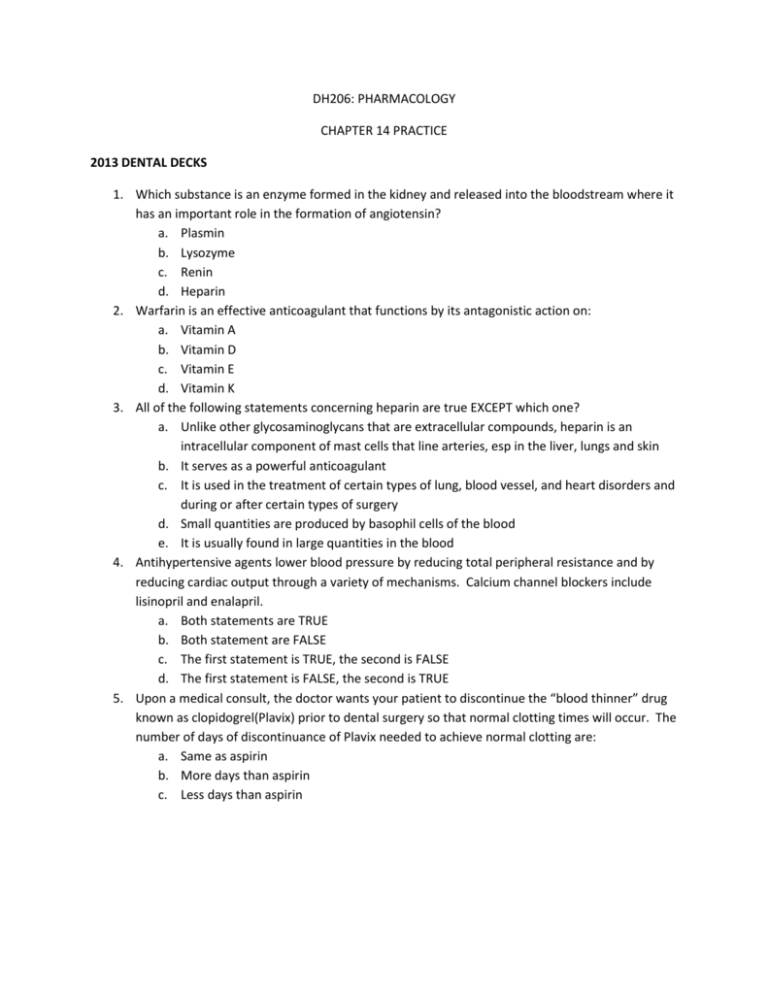
DH206: PHARMACOLOGY CHAPTER 14 PRACTICE 2013 DENTAL DECKS 1. Which substance is an enzyme formed in the kidney and released into the bloodstream where it has an important role in the formation of angiotensin? a. Plasmin b. Lysozyme c. Renin d. Heparin 2. Warfarin is an effective anticoagulant that functions by its antagonistic action on: a. Vitamin A b. Vitamin D c. Vitamin E d. Vitamin K 3. All of the following statements concerning heparin are true EXCEPT which one? a. Unlike other glycosaminoglycans that are extracellular compounds, heparin is an intracellular component of mast cells that line arteries, esp in the liver, lungs and skin b. It serves as a powerful anticoagulant c. It is used in the treatment of certain types of lung, blood vessel, and heart disorders and during or after certain types of surgery d. Small quantities are produced by basophil cells of the blood e. It is usually found in large quantities in the blood 4. Antihypertensive agents lower blood pressure by reducing total peripheral resistance and by reducing cardiac output through a variety of mechanisms. Calcium channel blockers include lisinopril and enalapril. a. Both statements are TRUE b. Both statement are FALSE c. The first statement is TRUE, the second is FALSE d. The first statement is FALSE, the second is TRUE 5. Upon a medical consult, the doctor wants your patient to discontinue the “blood thinner” drug known as clopidogrel(Plavix) prior to dental surgery so that normal clotting times will occur. The number of days of discontinuance of Plavix needed to achieve normal clotting are: a. Same as aspirin b. More days than aspirin c. Less days than aspirin 6. Which of the drugs listed below would increase the risk of bleeding in your dental hygiene patient during an invasive procedure? a. Acetaminophen(Tylenol) b. Diazepam(Valium) c. Pregabalin(Lyrica) d. Prasugrel(Effient) 7. The principle indication for digoxin is heart failure. The potential for toxicity is the major disadvantage of digoxin use. a. Both statements are TRUE b. Both statement are FALSE c. The first statement is TRUE, the second is FALSE d. The first statement is FALSE, the second is TRUE 8. All of the following drugs are ACE inhibitors EXCEPT which one? a. Methocarbamol(Robaxin) b. Ramipril(Altace) c. Benazepril(Lotensin) d. Enalapril(Vasotec) e. Lisinopril(Zestril) f. Fosinopril(Monopril) g. Quinapril(Accurpil) h. Perindopril(Aceon) 9. Which antiarrhythmic is effective only on the ventricle and is often administered IV to treat lifethreatening ventricular arrhythmias? a. Quinidine b. Lidocaine c. Disopyramide(Norpace) d. Propafenone(Rythmol) 10. The protype loop diuretic is HCTZ. Diuretics are used to treat CHF by relieving edema and symptoms of dyspnea arising from pulmonary congestion. a. Both statements are TRUE b. Both statement are FALSE c. The first statement is TRUE, the second is FALSE d. The first statement is FALSE, the second is TRUE 11. Which of the following calcium channel blocker agents is a useful anti-arrhythmic and antianginal agent? a. Verapamil(Calan) b. Nifedipine(Procardia) c. Amlodipine(Norvasc) d. All of the above 12. All of the following drugs are used to prevent or to provide relief of angina pectoris EXCEPT which one? a. Nitroglycerine b. Lisinopril(Prinivil) c. Nifedipine(Procardia) d. Diltiazem(Cardizem) e. Propranolol(Inderal) 13. All of the following conditions are managed by using anticoagulants and anti-platelet agents EXCEPT which one? a. Coronary artery disease b. Angina pectoris c. MI d. Stroke e. Hypertension 14. Which of the following drugs inhibits blood clotting by inhibiting platelet aggregation in an irreversible manner and does not cause gastric ulcers? a. Heparin b. Warfarin(Coumadin) c. Vitamin K d. Aspirin e. Clopidogrel(Plavix) 15. Warfarin(Coumadin) competitively blocks: a. Vitamin A-binding sites and inhibits the synthesis of vitamin A-dependent coagulation factors II, VII, IX, X b. Vitamin b-binding sites and inhibits the synthesis of vitamin B-dependent coagulation factors II, VII, IX, X c. Vitamin D-binding sites and inhibits the synthesis of vitamin D-dependent coagulation factors II, VII, IX, X d. Vitamin K-binding sites and inhibits the synthesis of vitamin K-dependent coagulation factors II, VII, IX, X 16. Your patient is taking Warfarin(Coumadin) as a blood thinner. To reduce the amount of bleeding during a root planning procedure, the doctor has adjusted the warfarin dose. After the procedure the dose was adjusted back to the original. He needs an analgesic after root planning and is a recovering alcoholic. Which pain reliever would be best in this case? a. Tylenol #3 b. OTC ibuprofen c. OTC acetaminophen d. Vicodin 17. The following drugs are noted for causing what prominent oral side effect? Amitripyyline(Elavil) Diphenhydramine(Benadryl) Atropine Diazepam(Valium) 18. All of the following drugs listed would NOT increase the risk of bleeding in your dental patient during an invasive procedure EXCEPT which one? a. Fexofenadine(Allegra) b. Dabigatran etexilate(Pradaxa) c. Levothyroine(Synthyroid) d. Metoprolol(Toprol XL) 19. All of the following drugs are HMG-CoA reductase inhibitors EXCEPT which one? a. Atorvastatin(Lipitor) b. Fluvastatin(Lescol) c. Lovostatin(Mevacor) d. Pravastatin(Pravachol) e. Gemfibrozil(Lopid) f. Rosuvastatin(Crestor) g. Simvastatin(Zocor) 20. For a patient who is taking anticoagulants such as Warfarin(Coumadn), what is the most valuable test used in evaluating the patient as a surgical risk? a. PTT (partial thromboplastin time) b. PT (prothrombin time) c. Platelet count d. Bleeding time 21. Which 3 of the following analgesics may interact with warfarin(Coumadin) to cause increased risk of bleeding? a. Acetaminophen b. Ibuprofen(Motrin) c. Hydrocodone with acetaminophen d. Naproxen(Anaprox) e. Etodolac(Lodine) 1.C 2.D 3.E 4.C 5.A 6.D 7.A 8.A 9.B 10.D 11.A 12.B 13.E 14.E 15.D 16.C 19.E 17.Xerostomia 20.B 18.B 21.B,D,E MULTIPLE CHOICE 1. The therapeutic actions of angiotensin-converting enzyme (ACE) inhibitors include: a. Arterial dilation b. Elimination of sodium c. Venous dilation d. All statements are true 2. The mechanism of action of loop diuretics is to: a. Block aldosterone receptors b. Increase sodium excretion at Loop of Henle c. Block sodium channel at nephron collecting ducts d. Increase the release of aldosterone 3. The actions of digoxin(Lanoxin) include: a. Decreased heart rate b. Inhibition of Na/K ATPase c. Increased calcium inside the heart muscle d. All statement are true 4. The actions of carvedolol(Coreg) include: a. Blockage of beta receptors b. Increased force of myocardial contraction c. Blockage of alpha-1 receptors d. Both A & C are true 5. The most effective drug to relieve edema and congestion in acute heart failure would be: a. Hydralazine(Apresoline) b. Furosemide(Lasix) c. Metoprolol(Lopressor) d. HCTZ 6. Which of the following reduces edema by blocking the reabsorption of sodium in the distal tubules? a. Eplerenone b. Torsemide c. Triamterene d. Chlorothiazide 7. Vasodilators increase afterload work on which part of the circulatory system? a. Veins b. Arteries c. Cardiac nervous tissue d. Myocardium 8. Select the 2 adverse effects of digoxin. a. Atrial tachycardia b. Hypokalemia c. Ventricular fibrillation d. Angioedema e. Arrhythmias 9. The 2 main effects of beta blockers include: a. Slowing the heart rate b. Reducing the release of renin c. Decreasing vasoconstriction d. Increasing sodium retention Match the following descriptions with definitions. 10. 11. 12. 13. 14. Arrhythmia that originate below the AV node A drug used to restore normal cardiac rhythm Heart area of abnormal electrical impulse generation Arrhythmia that originates in the atrial or AV nodal area A disorder of cardiac conduction a. antiarrhythmic b. arrhythmia c. ectopic foci d. ventricular arrhythmia e. supraventricular arrhythmia 15. Select all the ions that regulate heart activity a. Cl b. Na c. K d. Ca 16. Select the ion movement that is associated with depolarization of ventricular muscles a. Na ions move out of cell b. K ions move out of cell c. Na ions move into cell d. Ca ions move into cell 17. The pharmacological effects of verapamil include: a. Decreased heart rate b. Decreased force of contraction c. Slowed SA/AV condition d. All of the above 18. Arrhythmias can be treated with which of the following drug classes? SELECT ALL THAT APPLY. a. Na-blockers b. Ca-blockers c. Beta-blockers d. K-blockers 19. The therapeutic actions of propranolol to prevent angina attacks include: a. Decreased heart rate b. Reduced force of myocardial contraction c. Decreased oxygen consumption d. All the above are true 20. In the treatment of angina, the drug that is an arterial dilator and can be used in long-term management or acute attacks is: a. Nitroglycerine b. Metoprolol c. Nifedipine d. Varapamil 21. All of the following are used in the treatment and management of hypertension EXCEPT which one? Which one is the EXCEPTION? a. Beta-blocker b. Alpha-blocker c. Diuretic d. Na-blocker e. Vasodilator 22. The main mechanisms of action of nitrates include: a. Increasing the venous return to the heart b. Reducing arthrosclerosis in the arteries c. Increasing cardiac work and oxygen consumption d. Relaxation of systemic veins and arteries 23. Which of the following drugs causes vasodilation and can be useful in treating hypertension and congestive heart failure? a. Captopril(Capoten) b. Furosemide(Lasix) c. Amlodipine(Norvasc) d. Metoprolol(Lopressor) 24. Which of the following actions is related to thiazide diuretics? a. Hypokalemia b. Hypernatremia c. Hypercalcemia 25. Which of the following is NOT routinely used in the clinical management of hypertension? a. Thiazide diuretics b. Chlorthalidone c. Triamterene d. Ranolazine 26. Which of the following agents has the most dangerous interaction with Warfarin? a. Acetaminophen b. Aspirin c. NSAIDs d. Hydrocodone 27. The angiotension-converting enzyme (ACE) is released from which organ? a. Heart b. Liver c. Kidney d. Lungs 28. The antihypertensive action of HCTZ includes: a. Reduction of blood volume b. Blockage of alpha-receptors c. Blockage of beta-receptors d. Sodium retention 29. A decrease in the formation of angiotensin II and an increase in the concentration of bradykinin explains the vasodilator action of: a. Alpha-blockers b. Beta-blockers c. ACEI d. ARB 30. The release of renin causes which of the following? a. Activation of RAA mechanism b. Vasodilation c. Water excretion d. Decreased blood pressure 31. Prazosin(Minipress) works to reduce blood pressure by which of the following actions? a. Increasing sympathetic nerve activity b. Stimulating inhibitory alpha-2 receptors c. Dilating blood vessels d. Decreasing the release of renin in the kidneys 32. Which of the following makes platelets less sticky so a clot cannot form? a. Warfarin b. Clopidogrel(Plavix) and aspirin c. Standard heparin d. Urokinase Match the following terms with the definitions 33. A dietary lipid normally synthesized in the body 34. A protein in the plasma that transports triglycerides and cholesterol 35. Abnormally high levels of lipids in the plasma 36. A dietary lipid normally used by the body 37. A drug used to lower plasma lipid levels a. cholesterol b. hyperlipidemia c. hypolipidemic d. lipoprotein e. triglyceride 38. All of the following is correct about bad cholesterol EXCEPT which one? a. It is a high-density lipoprotein b. High levels of LDL contribute to atherosclerosis c. It is a lipoprotein d. It contains fat and less protein than good cholesterol 39. The greatest reduction in circulating LDL is associated with which 2 hyperlipidemic drugs? a. Statins b. Niacin c. Cholestyramine d. Gemfibrozil(Lopid) 40. Which of the following makes cholesterol so important for the body. a. Building block of glucocortoids b. Essential for building cell membranes c. Needed to help form myelin sheath d. All of the above 41. The main effects of the statins include which 2? a. Reducing LDL levels b. Reducing HDL levels c. Reducing acetyl CoA levels d. Reducing CPR levels 42. HMG-CoA reductase inhibitors work by doing which 2 of the following? a. Blocking the intestinal absorption of cholesterol b. Inhibiting triglyceride lipase c. Inhibiting the production of mevalonic acid d. Decreasing VLDL synthesis 1.D 2.B 3.D 4.A 5.B 6.D 7.B 8.B,E 9.A,B 10.D 11.A 12.C 13.E 14.B 15.B,C,D 16.A 17.D 18.A,B,C,D 19.D 20.A 21.D 22.D 23.A 24.A 25.D 26.B 27.D 28.A 29.C 30.A 31.B 32.B 33.A 34.D 35.B 36.E 37.C 38.A 39.A,C 40.D 41.A,C 42.C,D