THE MALE REPRODUCTIVE SYSTEM
advertisement

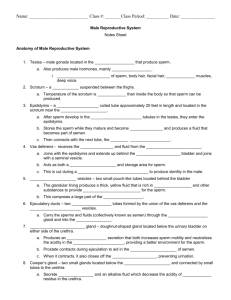
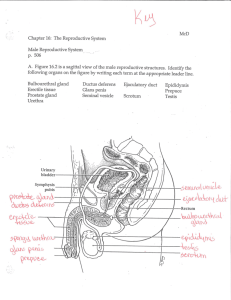
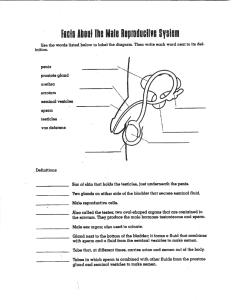
THE MALE REPRODUCTIVE SYSTEM HOMEOSTASIS male & female reproductive organs work together to produce offspring female reproductive organs also contribute to sustaining the growth of embryos and fetuses Sexual Reproduction process by which organisms produce offspring by making germ cells (gametes) fertilization: when male gamete (sperm) unites with female gamete (secondary oocyte) fertilized egg males & females have anatomically distinct reproductive organs that function to 1. produce gametes 2. facilitate fertilization 3. sustain growth of embryo & fetus (female) Reproductive Organs Females Males Gonads: testes Gonads: ovaries Ducts Ducts store & transport gametes Accessory Sex Glands Supporting Structures Penis transport gametes Accessory Sex Glands Supporting Structures: Uterus Male Reproductive System Organs: Testes 2. system of ducts 3. accessory sex glands 4. supporting structures: 1. scrotum penis Functions of the Male Reproductive System 1. 2. 3. 4. 5. Testes produces sperm & the male sex hormone Testosterone (T) Ducts transport, store, & assist in maturation of sperm Accessory sex glands secrete most of liquid portion of semen Penis contains the urethra, passageway for ejaculation of semen & excretion of urine Scrotum protects temperature-sensitive testes from temperature fluctuations Scrotum a supporting structure for the testes features: loose skin & superficial fascia attached from root of penis externally: raphe: median ridge that separates scrotum into right & left sides internally: scrotal septum: divides scrotum into 2 sacs, each with 1 testes Scrotum - 2 features continued: dartos muscle: smooth muscle fibers contraction causes wrinkled appearance (reduces heat loss) cremaster muscle: skeletal muscle 2 features regulate temp of testes: location outside trunk keeps temp 2 – 3 °C lower than core body temp 2. in response to cold temps, both muscles contract moving testes closer to body so can absorb body heat 1. Testes (plural)/ Testis (singular) aka testicles paired oval glands develop near kidneys begin descent into scrotum thru inguinal canals during latter half 7th month gestational age leading edge covered with peritoneum called tunica vaginalis Hydrocele: serous fluid collects between this & testis (injury or inflammation of epididymis) Hydrocele Testes - 2 tunica albuginea: internal to tunica vaginalis dense irregular CT extends inward into testis forming septa: divide testis into series of 200 – 300 lobules (internal compartments) each lobule contains 1 – 3 coiled seminiferous tubules : *site of production of semen spermatogenesis: process by which seminiferous tubules produce sperm Testes Seminiferous Tubules 2 types of cells: spermatogenic cells 1. sperm-forming cells: spermatogonia: stem cells primordial germ cells arise in yolk sac & enter testes during 5th wk of development: remain dormant until puberty 1° spermatocytes, 2° spermatocytes, spermatids, sperm cells (layers of progressively more mature cells) 2. Sertoli cells function in supporting spermatogenesis Spermatogenesis Sertoli Cells aka sustentacular cells extend from basement membrane lumen of tubule held together by tight junctions form obstruction known as the blood-testis barrier: all substances must pass thru Sertoli cells to reach developing sperm cells (after spermatogonia) Sertoli Cell Functions of the Sertoli Cells 1. 2. 3. 4. 5. 6. nourish spermatocytes, spermatids, & sperm phagocytoze excess spermatid cytoplasm as they develop into sperm control movements of spermatogenic cells & release of sperm into lumen of seminiferous tubules produce fluid for sperm transport secrete hormone inhibin mediate effects of T & FSH Leydig Cells interstitial cells (between seminiferous tubules) *secrete T Sperm ~300 million sperm complete spermatogenesis/d ~60 μm long once ejaculated last ~48 hours w/in female reproductive tract Hormonal Control of the Testes Ducts of the Male Reproductive System fluid secreted by Sertoli cells generates pressure which pushes sperm & fluid along lumen of seminiferous tubule eventually released as ejaculate Epididymis epi = over or above / didymis = testis aka: ductus epididymis plural:epididymides comma-shaped organ lies along posterior border of each testis ductus epididymis 2. head 3. body 4. tail 1. Ductus Epididymis ~6 m in length pseudostratified columnar epithelium lined with microvilli called stereocilia increase surface area for reabsorbing degenerated sperm surrounded by smooth muscle Function of epididymis: *sperm maturation (acquire motility & ability to fertilize an ovum) smooth muscle contraction propels sperm into ductus deferens sperm storage (viable up to several months) Ductus Deferens/ Vas Deferens ascends along posterior border of epididymis inguinal canal entering pelvic cavity loops over ureter passes down posterior surface of urinary bladder terminal end is dilated = ampulla pseudostratified columnar epithelium 3 layers smooth muscle (inner & outer layers longitudinal, middle layer circular) Function of Vas Deferens Function: conveys sperm from epididymis urethra by peristaltic contractions 2. sperm storage (several months) 1. sperm not ejaculated are reabsorbed Vasectomy main method for sterilization of males portion of each vas deferens is cut out & ends ligated sperm production continues but do not reach exterior degenerate & destroyed by phagocytes Ejaculatory Ducts formed by union of duct from seminal vesicle & ampulla of ductus deferens pass inferiorly & anteriorly thru prostate gland terminate in prostatic urethra where they eject sperm & seminal vesicle secretions just before the release of semen from urethra to exterior Urethra shared terminal duct of reproductive & urinary systems passes thru: prostate deep muscles of perineum penis Urethra 3 parts: Prostatic Urethra 2. Membranous Urethra 1. portion thru deep perineal muscles 3. Spongy (penile) Urethra portion thru corpus spongiosum of penis ends at external urethral orifice Parts of Male Urethra Accessory Sex Glands secrete most of liquid portion of semen Include: Seminal Vesicles 2. Prostate 3. Bulbourethral Glands 1. Seminal Vesicles aka seminal glands paired, convoluted, pouchlike structures posterior to base of urinary bladder (superior surface) & anterior to rectum *secrete alkaline, viscous fluid: (~60% of vol of semen) fructose prostaglandins clotting proteins (different from those in blood) Seminal Vesicles Fluid alkaline to neutralize acidic environment of male urethra & female vagina (acids inactivate or kill sperm) fructose:used for ATP production in sperm prostaglandins contribute to sperm motility & viability clotting proteins help semen clot after ejaculation Prostate single, donut-shaped gland ~size of a golf ball inferior to urinary bladder surrounds prostatic urethra increases in size from birth to puberty when it expands rapidly until ~ age 30, remains stable ~ age 45, further enlargement may occur after that Prostatic Fluid milky, slightly acidic ~25% of vol of semen empties urethra thru many prostatic ducts contains: citric acid (ATP production in sperm) 2. several proteolytic enzymes 1. PSA: prostate-specific-antigen 3. acid phosphatase (function unknown) 4. seminalplasmin: bacteriocidal Bulbourethral Glands aka Cowper’s glands pea sized, inferior to prostate gland on either side of membranous urethra ducts open into spongy urethra secrete 1. alkaline fluid (protects sperm from acidic environment of spongy urethra) 2. mucus lubricates end of penis & lining of urethra (decreases # of sperm damaged during ejaculation) Semen mixture of sperm & seminal fluid (secretions of seminiferous tubules, seminal vesicles, prostate, & Cowper’s glands) average vol: 2.5 – 5 mL with 50 – 150 million sperm/mL <20 million sperm per mL probably infertile pH: 7.2 – 7.7 provides sperm with: 1. transportation medium 2. nutrients 3. protection from hostile acidic environment of male urethra & female vagina Penis contains urethra passageway for urine & semen Parts: Body 2. Glans Penis 3. Root 1. Body of the Penis Corpora Cavernosa: 2 dorsolateral masses Corpus Spongiosum: midventral mass spongy urethra w/in Circumcision portion of prepuce (fore skin)surgical excised 3 – 4 days after delivery or 8th day for Jewish rite