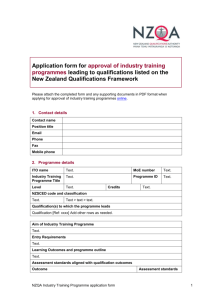
Consultant Guidance Document
advertisement

Guidance for Consultants Conducting Site Visits and Preparing Site Visit Reports for Health Resources and Services Administration/Bureau of Primary Health Care Programs Updated November2014 This document provides guidance to consultants on conducting site visits and completing site visit reports for Health Resources and Services Administration (HRSA)/Bureau of Primary Health Care (BPHC) grant and non-grant programs. Site visits support HRSA/BPHC program oversight roles and responsibilities. The most common type of site visit is the Operational Site Visit (OSV), which provides an objective assessment and verification on the status of each Health Center Program grantee and look-alike’s compliance with statutory and regulatory requirements of the Health Center Program (http://www.bphc.hrsa.gov/about/requirements/index.html). OSVs also provide a review of progress on clinical and financial performance, and, if applicable, progress on the implementation and completion of capital and/or other grant activities. When appropriate, other types of site visits may be conducted and utilized to: provide health centers with assistance in addressing areas of non-compliance; focus on specific areas of clinical, financial or other areas of performance improvement; and/or assist with the identification and implementation of best practices. HRSA/BPHC also conducts other specialized site visits, such as those for Primary Care Associations, the Federal Tort Claims Act (FTCA) Program, and other grant programs administered by HRSA/BPHC as well as for other special purposes (e.g., Service Area Overlap Analysis, etc.). See Table A for summary of site visit types and required report formats. I. Site Visit Process A. Summary of Required Elements of all Operational Site Visits (OSVs). As appropriate a subset of these elements are to be utilized for other BPHC Site Visit Types: Pre-OSV conference call with consultant Site Visit Team, BPHC, and health center staff. Entrance Conference on first day of the OSV. Complete assessment of all applicable sections of the Health Center Program Site Visit Guide (http://www.bphc.hrsa.gov/policiesregulations/centerguide.html). At least one consultant team meeting during the site visit to: ensure that draft Site Visit Report findings and recommendations are consistent and cohesive; resolve any discrepancies or duplication of findings; and assure that all documentation/assessment of findings have been completed. Debrief of health center’s Chief Executive Officer/Executive Director (CEO/ED) prior to the Exit Conference. 1 of 38 Exit Conference on last day of the OSV. Time permitting, consultants may also use time on site during the OSV to: Begin collaborative report writing with team members. Provide limited TA above and beyond assessment activities required of the OSV to the health center (e.g., provide suggestions for successful Board recruitment/retention). This TA is NOT to be documented in the Site Visit Report, but rather to be communicated directly to the health center. Document any innovative/best practices in Site Visit Report observed during the site visit. B. Site Visit Team Roles and Responsibilities Consultant Team Leader (TL) Roles and Responsibilities: Contact BPHC Project Officer (PO) to obtain background information on the health center, including any critical issues identified since the last review. Contact individual team members prior to site visit in order to share information about the health center, provide grantee point of contact information, location/address for OSV entrance conference, etc. Contact health center’s CEO/ED to make an introduction and confirm Entrance Conference arrangements. Establish interview schedule with Key Management Staff, Board Members, and other partners. Request meeting space and directions to the site. Contact should be made at least three weeks prior to the site visit. Prior to arriving on site, identify documents needed from the health center in order to facilitate the review. Develop an agenda for the site visit, finalize it upon PO approval, and share it with BPHC staff and the grantee at least one week prior to the site visit. See template agenda in Appendix B. Coordinate and schedule the pre- and post-site visit conference call, as needed, with the Site Visit Team, health center leaders, and the BPHC PO. Facilitate Entrance Conference. (If the PO is on the site visit in person or by phone, he/she will open and close the Entrance Conference.) Clarify each team member’s role while on site. Conduct daily briefings with the team and CEO/ED. Conduct site visit in accordance with the Health Center Program Site Visit Guide (http://www.bphc.hrsa.gov/policiesregulations/centerguide.html) or other applicable HRSA/BPHC site visit guide (e.g., FTCA Site Visit Guide). Facilitate pre-Exit Conference with CEO/ED. Facilitate Exit Conference with health center staff/board members. (If the PO is on the site visit in person or by phone, he/she will open and close the Exit Conference.) 2 of 38 Encourage the health center to complete and submit the Consultant Evaluation Form once the visit has concluded. Contribute to and finalize the consolidated Site Visit Report that includes the findings of all team members using the MSCG Online Site Visit Report (OSVR) System based on the site visit type (see Table A and Appendix A for details). Check for inconsistencies in findings and correct any incomplete sentences, spelling mistakes, grammatical errors, formatting issues, etc. Upload the final report into the HRSA Technical Assistance Tracking System (TATS) (see Table A for details) for BPHC staff review. TATS is HRSA’s centralized system for the initiation and tracking of a site visit or other TA within the HRSA Electronic Handbooks (EHBs). Submit reimbursement voucher and receipts to MSCG. Contact MSCG regarding changes to site visit logistics, such as changes in hotel or flight schedule, team member participation and attendance, cooperation of site personnel, etc. Does not make contact with the health center following the site visit without the BPHC PO’s knowledge or consent. Consultant Team Member Roles and Responsibilities: Coordinate with MSCG staff to confirm travel arrangements. Contact Team Leader and BPHC PO to obtain background information on the grantee, including any critical issues identified since the last review, for review prior to the OSV. Participate in pre- and post-site visit calls, if required. Schedule staff interviews and document reviews. Attend team meeting prior to Entrance Conference with grantee. Interact with other team members during the course of the review. Participate in the Entrance and Exit Conference. Complete assigned areas of review (e.g. clinical, financial, governance) in accordance with the Health Center Program Site Visit Guide (http://www.bphc.hrsa.gov/policiesregulations/centerguide.html) or other applicable HRSA/BPHC site visit guide. Coordinate findings with other members of the Site Visit Team. Attend pre-Exit Conference, as applicable, and participate in Exit Conference. Complete Team Member’s portion(s) of the consolidated site visit report using the Online Site Visit Report (OSVR) System in the required format (See Table A and Appendix A for details) Submit the reimbursement voucher along with receipts to MSCG, BPHC’s current contractor. Contact MSCG regarding changes to site visit logistics, such as changes in hotel or flight schedule, team member participation and attendance, cooperation of site personnel, etc. 3 of 38 Does not make contact with the health center following the site visit without the BPHC PO’s knowledge or consent. Note: For OSVs, the Team Leader and Team Members must conduct at least one consultant team meeting during site visit to: ensure that the draft Site Visit Report findings and recommendations are consistent and cohesive; resolve any discrepancies or duplication of findings; and assure that all documentation/assessment of findings have been completed. BPHC Project Officer/Staff Roles and Responsibilities: The BPHC Project Officer (PO) and any other BPHC staff participants have an oversight and facilitation role during the site visit, with continued interaction and direct feedback to the health center in terms of policy assistance and interpretation, problem resolution, and ongoing monitoring of compliance, as well as clinical and financial performance improvement measures after the site visit. Consistent with their role as the health center’s primary BPHC point of contact with, the BPHC PO/staff members: Develop the TA request in EHB TATS. The TA request must detail the specific purpose for the site visit and the site visit report. This is essential so that the consultants have a clear understanding of what is expected of them on site and in their report. This PO documentation is essential because consultants must copy the purpose from the TA request from TATS directly into the report without the ability to rewrite, reword, or change the purpose without concurrence from the BPHC Health Services Senior Manager. Based on site visit type, transmit the necessary required background documents and information to MSCG for the consultant(s). Contact the appropriate state/regional Primary Care Association (PCA) to inform them of any OSVs to Newly Funded Health Center Program grantees; invite them to attend, and include them (per BPHC PO and/or Branch Chief’s discretion) in the pre-site visit conference call. As appropriate for all other types of health center site visits, notify the PCA of an upcoming site visit and reiterate their potential role as an observer and contributor of state-specific information. Participate in pre-site visit conference call(s) with the consultant(s), PCA, capital grant PO, and others, as appropriate, identify any additional materials needed for the visit, review and approve the final agenda, discuss logistics and share any specific concerns/issues. An hour-long call is recommended for the pre-site visit conference call, with the first half reserved for discussion among the consultant(s), PO, and any other BPHC staff. The consultant(s), PO, and the health center should be included during the second half of the call only. Lead the site visit as HRSA’s official agent by introducing the team, kicking off both the Entrance and Exit Conference, and assisting in any way that contributes to an effective review, whether on site or by phone. Provide information, responses, and resources for questions (or follow-up on such questions after the visit) related to: HRSA/BPHC policy, Health Center Program requirements, approved grantee budgets, funding opportunities (as applicable), and other 4 of 38 relevant BPHC and/or HRSA activities, and TA resources. Conduct follow up with the grantee on any findings included in the final Site Visit Report and subsequent conditions issued by BPHC. Provide necessary support/technical assistance to support the grantee in addressing compliance and/or performance measures. C. Entrance and Exit Conferences Entrance Conference: All site visits begin with an Entrance Conference. At a minimum, the Entrance Conference must include participation of the BPHC PO, the health center’s senior management staff, and Board members. Participation may include other federal officials and/or health center staff as determined by the health center. The Entrance Conference should be approximately one hour in length, and include the following steps and components: 1. Introduction of the team including a brief statement about each consultant’s professional expertise and experience. n all site visits where the BPHC PO participates, the introductory portion of the Entrance Conference is kicked-off by the BPHC PO. 2. Opening remarks by the BPHC PO and Consultant Team Leader in order to: Review the purpose, scope and intended outcome of the visit; Review the agenda for the visit and make any necessary changes; Conduct a question and answer session about the purpose of the visit; If requested, BPHC PO may provide a BPHC/Health Center Program overview using the BPHC-approved Project Officer Site Visit Presentation; and Thank the health center staff and Board in advance for their time. 3. Optional grantee overview, including any major accomplishments/successes and any recent changes at the health center. 4. Closing remarks by the BPHC PO in order to indicate that any findings and recommendations identified during the site visit will be shared with the grantee via the final Site Visit Report and that the BPHC PO will be the central point of contact for any follow-up questions or actions. Exit Conference/Debriefing: The site visit concludes on the last day with an Exit Conference. The participant list for the Exit Conference mirrors that of the Entrance Conference. For OSVs, the Site Visit Team must conduct a short debrief for the health center’s CEO/ED prior to the full Exit Conference. On all site visits, the Exit Conference is kicked-off by the BPHC PO whether on site or via phone, in coordination with the consultant Site Visit Team. General findings from all aspects reviewed while on site (e.g., for an OSV, Program Requirement Compliance Analysis, Clinical and Financial Performance Analysis, Capital Programs Reviewed) are summarized by members of the team and any follow-up actions/steps are discussed, if applicable. As compliance 5 of 38 determinations may require further input and review from BPHC staff, it should be clarified that the final status of individual program requirement findings (met or not met) will be communicated by the BPHC PO through the transmission of the final site visit report. Note: If there are major issues and/or sensitive situations regarding compliance findings, the BPHC PO, BPHC staff and, if appropriate, the Branch Chief, may request a post-site visit conference call/debrief with the consultant(s) to clarify the findings of non-compliance with Health Center Program requirements PRIOR to the consultant(s)’ completion of the initial draft of the report. In these cases, MSCG and/or the Consultant Team Leader organizes the debrief call within the 7 business days to ensure timely submission of the report to MSCG. II. Site Visit Report Completion: A. General Points for Site Visit Report Completion (See Appendix C for report examples) Reports are expected to provide BPHC staff with an accurate, objective depiction of the compliance status of the health center (or other BPHC program, e.g., FTCA). The health center/other BPHC program organization will also receive a copy of the final report, after it is approved by BPHC. All information contained in the report must be based on facts. Consultants must not include opinions, use terms that could be considered inflammatory or derogatory, or use blanket statements. All information must be sourced to clarify if the information was gathered from a specific grantee document or from statements made by specific grantee staff/Board members, direct observation by the consultant during the site visit or other specific source. When assessing Health Center Program requirements, a requirement is either “Met” or “Not Met,” not “partially met” or “not completely met.” If any part of the requirement is not met, then the finding is “Not Met” (or “Not in Compliance”). “Met” or “Not Met” is to be assessed for each part of each Health Center Program requirement when the site visit type indicates compliance assessment. Consultant findings must address every question associated with each Health Center Program requirement contained within the online OSV report format. If the site visit included BPHC/MSCG vetted training documents and/or packaged presentations (PowerPoint, etc.), the consultant must include these and any other items of informational value as attachments to the uploaded report in EHB TATS. Note: Only documents that have been vetted by BPHC/MSCG can be shared with the health center/BPHC program. In circumstances where there is sensitive information that falls outside the scope of the visit (e.g. beyond an assessment of compliance and performance improvement) and must be conveyed to BPHC for a complete understanding and assessment of the grantee’s situation (or individual(s) within the grantee organization or Board), it should not be incorporated into the Site Visit Report but rather conveyed to the BPHC PO via post-site visit conference call. B. Site Visits-Report Completion by Site Visit Type: 6 of 38 o o o o Reports for OSVs: Consultants must ensure that all sections of the online report are completed and that all questions included in the Health Center Site Visit Guide are addressed in the report: Sections I-IV: Compliance assessment of all 19 Program Requirements across Need, Services, Management and Finance, Governance; Section V: Clinical and Financial Performance Analysis; Section VI: Capital and Other Grant Progress Review (if applicable); Section VII: Best Practices Documentation (if appropriate). OSV Supplemental Questions for 340B To Be Completed: When applicable, consultant teams must ensure that the 5 Questions added to the report template to assess the 340B Program are addressed in the report. Please note the following expectations for the team: o The consultants are not expected to review patient records or conduct any other type of sampling. o The clinical consultant will be responsible to address/ask the 340B questions and verify the existence of appropriate documents. o The Team Lead will be responsible for ensuring that the 340B questions have been answered electronically. o The site visit report will not be able to be submitted until the 340B responses have been entered. Reports for Program Requirement Verification Site Visits and Targeted Program Requirement Assessment Site Visits: Consultants must complete only the applicable sections (I-IV) of the online report based on the Health Center Program requirement(s) reviewed. Reports for Program Requirement Assistance Site Visits, Performance Improvement Site Visits, and Specialized Site Visits must utilize the Generic Report Format. See Appendix A for Online Generic Report Process. For further details on the report completion process and timeline, see Appendix A Table A. Summary of Site Visit Types and Corresponding Required Report Format: Site Visit Type Focus Areas Operational Site Visit (Includes Grantee and Look-Alike OSVs and Look-Alike Pre-designation Compliance Assessments) Program Requirement Verification Site Visit Compliance Only Compliance Clinical, Financial Performance Capital and Other Grant Progress Innovative/Best Practices Documentation 7 of 38 Site Visit Report Format Online Report Format-All Sections Online Report Format-Applicable Sections (e.g., Program Site Visit Type Focus Areas Site Visit Report Format Requirements #2 and #4 only) Targeted Program Requirement Assessment Site Visit Compliance Only Program Requirement Assistance Site Visit Compliance Only Performance Improvement Site Visit Specialized Site Visit FTCA Performance Improvement Only Best Practices Targeted TA for PCAs Strategic Planning Closeout Financial Recovery Plans Service Area Overlap PCA/NCA Assessment HCCN FTCA requirements 8 of 38 Online Report Format-Applicable Sections (e.g., Governance Program Requirements #17, #18, and #19 only) Online Generic Report Format Online Generic Report Format (e.g., Targeted TA provided to Newly Funded Grantees during their first year of funding) Online Generic Report Format Online FTCA Specific Format Appendix A Online Report Completion and Submission: Process and Timelines A. Online OSV/Compliance Related Site Visit Report The website link to the online report is: http://www.mscginc.com/OSVRTemplate. The report will become available on the day that the site visit begins. NOTE: Steps 1-7 must be completed prior to TATS upload and steps 1-8 are to be completed within 20 total calendar days of completion of the site visit. 1. Team Members complete their online sections for OSV within five business days (7 calendar days) of completion of the site visit. 2. Team Lead (TL) reviews online report and makes any changes deemed necessary; changes are to be completed online. 3. TL submits report to MSCG Reviewers and MSCG Technical Assistance Reviewer (TAR), using the “Send to MSCG Reviewers” button. This step MUST be done PRIOR to “Send for Edit” 4. MSCG Reviewer responds with comments via email to TL and cc to TAR within five business days for revisions, to be completed online. Note: TL does not send for edit until comments are returned from MSCG Reviewer and any revisions are completed. 5. Revisions are completed online. TL submits to MSCG TARS and MSCG Editors via the online system, using the “Send the Report to MSCG Editors” button. 6. MSCG Editor completes edits (e.g., format, grammar, punctuation, and spelling). 7. MSCG Editor sends the edited version in a Word document to the TL as a clean draft. 8. TL uploads MSCG edited draft into TATS within 1-3 business days of receipt of MSCG edit. (https://tats.hrsa.gov/webTATSEPSConsultant/login.aspx). 9. BPHC review process begins via TATS. B. Online Generic Report Reports for Program Requirement Assistance Site Visits, Performance Improvement Site Visits, and Specialized Site Visits must utilize the “Generic Report Format.” The website link to the online Generic Report is the same as for the Operational Site Visit Report: http://www.mscginc.com/OSVRTemplate. This will become available on the day that the site visit begins and the online system will only allow the correct format to be downloaded based on the type of site visit. NOTE: Generic report steps 1-3 are to be completed within 10 business days of the completion of the site visit. 1. Consultants must enter information into the report system within five business days of 9 of 38 completion of the site visit using the “Send the Report to MSCG Editors” button. 2. MSCG Editor completes edits (format, grammar, punctuation, and spelling) and sends edited version as a Word document to the consultant as a clean draft. 3. Consultant uploads MSCG edited draft report into HRSA’s Technical Assistance Tracking System (TATS) for BPHC’s review (https://tats.hrsa.gov/webTATSEPSConsultant/login.aspx ) within 1-3 days of receipt of MSCG edit. 4. BPHC review process begins via TATS. 10 of 38 Appendix B: Suggested Template OSV Agenda Site Name Site Visit Agenda Day 1 8:30 a.m. Consultants Arrive on Site 9:00 a.m. Entrance Conference Purpose of site visit (Federal Project Officer if participating, Team Lead if PO not participating) Introduction of each consultant(Team Lead) o Name o Professional background and experience o Area of focus for site visit Administration/Governance Clinical Fiscal 10:00 a.m. Health Center Updates/Status (Health Center CEO/delegate) Facility tour of main facility Optional: Team members visit satellite sites as previously discussed during pre-site visit conference call. Time permitting: Consultant team members commence document review and/or begin to meet individually with senior management team members as appropriate. 12:00 p.m. Lunch: Team members available to meet with Board Members in closed session (no staff present) during lunch on Day One or Day Two or at any other mutually convenient time as arranged by the Board Chair and CEO/ED. 1:30 p.m. Consultant team members continue document review and meeting with senior management team members/center staff as appropriate. 4:30 p.m. Adjourn. Day 2 11 of 38 8:30 a.m. Consultant team members continue document review and meeting with senior management team members/center staff as appropriate. Consultant team members provide on-site TA as requested and as appropriate. 12:00 p.m. Lunch − Option: Meet with Board or health center staff as appropriate. 1:30 p.m. Consultant team members continue document review and meeting with senior management team members/center staff as appropriate. Consultant team members review progress on current Capital Grants including: C81 Capital Improvement Program (CIP), C80 Facility Investment Program (FIP), C8A Capital Development (CD), and C12 School-Based Health Center Capital (SBHCC) Grants, as well as any one-time funding for minor construction activities included within New Access Point (NAP) Grants, 340B, or other grant programs, as appropriate. 4:30 p.m. Adjourn. Day 3 8:30 a.m. Consultant team members continue document review, or review on current NAP, Capital Development and other BPHC grants and meeting with senior management team members/center staff, as appropriate. 12:00 p.m. Lunch − Site visit team may use time to begin to discuss findings. 1:00 p.m. Consultant team members discuss and finalize compliance findings. If Project Officer or other BPHC staff is available, discuss compliance concerns prior to Exit Conference. If time permits, each consultant team member begins online report write-up. 2:00 p.m. Consultant team (and Project Officer if present/available) debriefs with CEO/ED prior to Exit Conference. 3:00 p.m. Exit Conference with health center senior management team and Board members who may be available, but expectation is for Board Chair to be present. Consultant team/Project Officer summarizes findings, make recommendations, and answer questions. Team Leader presents Site Visit Evaluation Form. 4:00 p.m. Adjourn (Note: If additional time is needed, this time may be pushed back). 12 of 38 Appendix C: Report Examples Operational Site Visit Report: III. Health Center Program Site Visit Report TA Request Number: TA000XXX Grantee Information: Name of Grantee Address 1 Address 2 Contact: Name, Title Contact phone/email Type of Visit: Operational Site Visit Date(s) of Visit: Month XX, XXXX Consultants: Consultant Name (Clinical/Financial/Admin./Governance); consultant email; consultant phone Consultant Name (Clinical/Financial/Admin./Governance); consultant email; consultant phone Consultant Name (Clinical/Financial/Admin./Governance); consultant email; consultant phone Site Visit Participants Name Title Interviewed Entrance Exit XXXX CEO Yes Yes Yes XXXX COO Yes Yes Yes XXXX CFO Yes Yes Yes XXXX CMO Yes Yes Yes XXXX Chief Dental Director Yes Yes Yes XXXX Chief Pharmacist Yes Yes Yes 13 of 38 Name Title Interviewed Entrance Exit XXXX Chief Compliance Yes Officer Yes Yes XXXX WBC Program Director No Yes Yes XXXX CIO Yes Yes Yes XXXX Director of Public No Affairs Yes Yes XXXX PCMH Director Yes Yes Yes XXXX Director of Programs No Yes Yes XXXX State PCA No Yes Yes XXXX Clinic Administrator Yes No No XXXX Pediatric NP Yes No No XXXX X-ray Technician Yes No No XXXX Lab Technician Yes No No XXXX Facilities Director Yes No No XXXX Board Member Yes No No XXXX Board Member Yes No Yes XXXX Board Member Yes No No XXXX Board Member Yes No No XXXX Board Member Yes No No 14 of 38 15 of 38 Program Requirement Compliance Review Summary Program Requirement Compliance Review Compliance Status 1. Needs Assessment Met 2. Required and Additional Services Met 3. Staffing Requirement Not Met 4. Accessible Hours of Operation/Locations Met 5. After-Hours Coverage Met 6. Hospital Admitting Privileges and Continuum of Care Met 7. Sliding Fee Discounts Met 8. Quality Improvement/Assurance Plan Not Met 9. Key Management Staff Met 10. Contractual/Affiliation Agreements Met 11. Collaborative Relationships Met 12. Financial Management and Control Policies Met 13. Billing and Collections Met 14. Budget Met 15. Program Data Reporting Systems Met 16. Scope of Project Not Met 17. Board Authority Met 18. Board Composition Met 19. Conflict of Interest Policy Met 16 of 38 Section 1. Need - Program Requirement #1 Program Requirement #1 - Needs Assessment Health center demonstrates and documents the needs of its target population, updating its service area, when appropriate. (Section 330(k)(2) and (k)(3)(J) of the PHS Act) Compliance Status: Met. Documents reviewed onsite or in advance: Most recent Needs Assessment(s) Service Area Map UDS patient origin data Health center’s list of sites with service area zip codes (Form 5B) Compliance Review Findings: XXXX has a comprehensive, written Community Health Needs Assessment that was updated as recently as February 2014. XXXX serves the defined service areas of XXXX and XXXX counties. This health service area is consistent with the patient origin data in the UDS. (Ethnic group) comprised approximately 81% of the population. A unique subset of the XXXX population are XXXX, who are from XXXX and speak a language other than English or Spanish and whose culture requires special consideration for accessing health care services. The primary industry in the health service area is XXXX and many of the patients are seasonal migrant workers. Another growing special population for XXXX is the homeless population. XXXX opened a New Access Point in XXXX to serve the homeless population. The comprehensive Needs Assessment prepared in 2014 is a tool that serves XXXX well in identifying and planning for the needs of its health service area. Section 2. Services - Program Requirement #2 Program Requirement #2 - Required and Additional Services Health center provides all required primary, preventive, enabling health services and additional health services as appropriate and necessary, either directly or through established written arrangements and referrals. (Section 330(a) and (h)(2) of the PHS Act) Compliance Status: Met. Documents reviewed onsite or in advance: Health center’s official Scope of Project for Services (Form 5A) Clinical practice protocols and/or other policies and procedures that support the delivery of 17 of 38 health center services Contracts, MOAs, MOUs, etc. for services provided via formal written agreements and/or formal written referral arrangements, including general tracking and referral policies and procedures Other: Tracking of referrals, hospitalizations, laboratory results, x-rays, and mammograms policy and procedures Compliance Review Findings: Based on a review of documents, interviews with staff, and a tour of the facilities, the grantee provides all required primary, preventive, enabling health services as appropriate and necessary, both directly and through established written arrangements and referrals. Memoranda of Agreement (MOAs) exist for the following: Quest Lab Services (diagnostic lab) Imperial Radiology Services (diagnostic x-ray) Radiology Services of the Desert (x-ray over read) Imperial County Office of Education Head Start Program Imperial County Department of Health (HIV services) Imperial County Behavioral Health Services Walgreens and RiteAid (340B pharmacy services) The MOAs appropriately describe the manner by which referrals will be made and managed and the process for referring the patients back to the center. A Board-approved Tracking Policy and Procedures for the tracking of normal labs as well as the tracking and notification for abnormal lab and critical labs and x-rays are present. Section 2. Services - Program Requirement #3 Program Requirement #3 - Staffing Health center maintains a core staff as necessary to carry out all required primary, preventive, enabling health services and additional health services as appropriate and necessary, either directly or through established arrangements and referrals. Staff must be appropriately licensed, credentialed and privileged. (Section 330(a)(1), (b)(1)-(2), (k)(3)(C), and (k)(3)(I) of the PHS Act) Compliance Status: Not Met. Documents reviewed onsite or in advance: Staffing Profile Provider contracts, agreements, and any subrecipient arrangements related to staffing (as applicable) Credentialing and Privileging Policies and Procedures Documentation of provider licensure or certification for all licensed or certified health center practitioners 18 of 38 Privileging Lists Other: Six LIP credentialing files; six other licensed or certified health practitioner files Compliance Review Findings: Although the organization’s Board-approved Credentialing Policy and Procedures appropriately reflect the requirements of PIN 2002-22, “Clarification of Credentialing and Privileging,” a review of six LIP and six other licensed or certified health practitioner files does not appropriately reflect a credentialing process that meets the requirements of PIN 2002-22. Specifically, this includes the lack of documentation to support the following: Licensed Independent Practitioners No primary source of education is reflected in credentialing files. Other Licensed or Certified Health Practitioners Inconsistent primary source verification of licensure in credentialing files; No secondary source verification of education in credentialing files; and No NPDB queries. If Not Met - Steps/Actions Recommended for Compliance: The grantee must credential and privilege its LIPs and licensed or other certified health care practitioners either directly or through a CVO contract that meets the requirements set forth in PIN 2001-16, “Credentialing and Privileging of Health Center Practitioners,” and PIN 2002-22, “Clarification of Credentialing and Privileging.” In accomplishing this, the grantee should utilize the chart provided in the HRSA Site Visit Guide under Program Requirement #3 to ensure all components of credentialing and privileging for both LIPs and other licensed or certified health practitioners are appropriately addressed and accomplished. Additionally, the Board must approve all credentials and privileges of LIPs, unless the delegation of this responsibility is done via resolution or through the bylaws to an individual based on Board approved policies and procedures. Section 2. Services - Program Requirement #4 Program Requirement #4 - Accessible Hours of Operation / Locations Health center provides services at times and locations that assure accessibility and meet the needs of the population to be served. (Section 330(k)(3)(A) of the PHS Act) Compliance Status: Met. Documents reviewed onsite or in advance: Hours of operation for health center sites Most recent Form 5B: Service Sites (Note that the form lists only the TOTAL number of hours per week each site is open, not the specific schedule.) 19 of 38 Form 5C: Other Activities/Locations Service Area Map with site locations noted Other: Patient Orientation Packet Compliance Review Findings: Services are provided at 18 service sites with hours of operation ranging from 20 to 65 hours a week. Ten of the 18 sites provide extended hours either on specific days of the week or Saturdays and, in some situations, both. Both the XXXX and XXXX sites were visited and hours of operation were appropriately displayed on signage of the outside glass doors. Hours of operation are appropriately reflected in English and Spanish and on patient orientation packets. Section 2. Services - Program Requirement #5 Program Requirement #5 – After-Hours Coverage Health center provides professional coverage for medical emergencies during hours when the center is closed. (Section 330(k)(3)(A) of the PHS Act and 42 CFR Part 51c.102(h)(4)) Compliance Status: Met. Documents reviewed onsite or in advance: Health center’s After-Hours Coverage Policies and Procedures Agreements, systems and/or contracts that support after-hours coverage, if applicable Most recent Form 5A - Services Provided, see Emergency Medical Services Other: Telephone Triage Protocols, After-Hours Log, After-Hours Clinical Advice by Telephone Policy and Procedures Compliance Review Findings: Interviews with medical staff and a review of the After-Hours Policy and Procedures reflect an after-hours process through which an answering service answers all calls. If calls are of a medical or dental nature, calls are forwarded to a registered nurse employed by XXXX who triages calls and, based on the complaint, makes various clinical decisions relative to approved Telephone Triage Protocols. Registered nurses rotate the after-hours on call responsibilities weekly and, in cases where a physician or mid-level is required to consult, calls are forwarded to the medical provider handling after-hours call for that week. Medical staff has access to the XXX EMR and all information relative to the patients’ calls is appropriately documented into their medical record. Telephone triage logs are appropriately maintained. Section 2. Services - Program Requirement #6 Program Requirement #6 - Hospital Admitting Privileges and Continuum of Care Health center physicians have admitting privileges at one or more referral hospitals, or other such arrangement to ensure continuity of care. In cases where hospital arrangements (including admitting privileges and membership) are not possible, health center must firmly establish 20 of 38 arrangements for hospitalization, discharge planning, and patient tracking. (Section 330(k)(3)(L) of the PHS Act) Compliance Status: Met. Documents reviewed onsite or in advance: Most recent Form 5C: Other Activities/Locations (If applicable, hospitals where health center providers have admitting privileges should be noted on the form.) Other: XXXX Medical Center Hospitalization Agreement, XXXX Healthcare District Hospitalization Agreement, XXXX Hospital Agreement, Hospitalization and ER Tracking Policy and Procedures Compliance Review Findings: XXXX has MOAs with XXXX Medical Center, XXXX Healthcare District, and XXXX Hospital for the hospitalization of all lifecycles at all of its 18 sites throughout XXXX and XXXX counties. The MOAs clearly delineate the responsibility for notification of hospitalization, emergency room admittance, discharge planning, and patient tracking. The organization’s policy and procedures on hospitalization and emergency room tracking are thorough and delineate responsibility for tracking and appointments for follow-up with Emergency Department personnel and hospital dischargers, with information being tracked in the XXX EMR. Section 2. Services - Program Requirement #7 Program Requirement #7 - Sliding Fee Discounts Health center has a system in place to determine eligibility for patient discounts adjusted on the basis of the patient’s ability to pay. (Section 330(k)(3)(G) of the PHS Act and 42 CFR Part 51c.303(f) and (u)) Compliance Status: Met. Documents reviewed onsite or in advance: Schedule of Fees/charges for all services in scope Sliding Fee Discount Schedule/Schedule of Discounts (often referred to as the “Sliding Fee Scale”) Implementing policies and procedures for the Sliding Fee Discount Program Sliding fee signage and/or notification methods Sliding fee application form(s)/eligibility criteria Other: 2013 UDS Report Compliance Review Findings: XXXX provides services to all patients without regard to their ability to pay. The availability of sliding fee discounts is prominently displayed in signage posted in waiting areas in English and 21 of 38 Spanish, which are the languages used by most of the organization’s patients. Language line assistance, TTY services and interpreters are available as needed to assist clients with limited English proficiency to facilitate their access to services and income-based discounts. The organization has Board-approved policies for income-based discounts that utilize the most current Federal Poverty Guidelines. Policies are applied equally to all eligible patients, including the uninsured and the underinsured, and discounts are applied to all services under the grantee’s approved scope, as listed on Form 5 columns I and II. The organization updates its Sliding Fee Schedule each year to reflect changes in the Federal Poverty Guidelines. The fee schedule was designed to mirror charges for like services provided in the local market. A nominal fee of $20 is charged for medical and mental health services for patients whose income is at or below 100% of FPG. A nominal fee of $35 is charged for dental care for this same income group. Discounts are offered to patients with income greater than 100% of FPG but less than or equal to 200% of FPG, determined as a percentage of the full charge. Non-discounted fees are charged to patients whose income exceeds 200% of FPG. Implementing policies and procedures describe the process by which eligibility for discounts is determined for a 12-month period from the date of determination. The organization also has a financial hardship policy under which fees may be further reduced or waived on a case-by-case determination. Section 2. Services - Program Requirement #8 Program Requirement #8 - Quality Improvement/Assurance Plan Health center has an ongoing Quality Improvement/Quality Assurance (QI/QA) program that includes clinical services and management, and that maintains the confidentiality of patient records. (Section 330(k)(3)(C) of the PHS Act, 45 CFR Part 74.25 (c)(2)-(3), and 42 CFR Part 51c.303(c)(1)-(2)) Compliance Status: Not Met. Documents reviewed onsite or in advance: Quality Improvement/Quality Assurance (QI/QA) Plan and related and/or supporting policies and procedures (e.g., Incident Reporting System, Risk Management Policies, Patient Safety Policies) Clinical Director’s job description HIPAA-compliant Patient Confidentiality and Medical Records Policies and Procedures Clinical Care Policies and Procedures Clinical Information Tracking Policies and Procedures Compliance Review Findings: XXXX’s written Quality Assurance Plan (QAP) describes some QA activities within the organization, but lacks components relative to complete QI/QA Plan and evidence of meaningful QI processes. More specifically, the QA Plan and processes: 22 of 38 does not adequately reflect the scope of the plan or the authority and responsibility for Quality Assurance inclusive of the Chief Medical Officer, Executive Director, and Board of Directors. lacks documentation in the QI Meeting Minutes that reflects periodic assessments and identification of the necessity for change in the provision of services by the health center and results in the institution of such change where indicated. Documentation does not support the review and assessment of Clinical Performance Measures relative to an evaluation process or a rapid cycle process for improvement relative to specific clinical measures and outcomes. does not indicate procedures for an annual QI Work Plan that delineates the responsibilities of the QA Committee on a quarterly or annual basis. If Not Met - Steps/Actions Recommended for Compliance: The grantee must have a QA Plan that identifies the scope and responsible parties for the oversight of organizational Quality Assurance/Quality Improvement. The grantee must demonstrate periodic assessment of utilization of services and the quality of clinical services, particularly HRSA Clinical Performance Measures and the grantee’s dental and behavioral measures as outlined in the health care plan. This periodic assessment must demonstrate identification and documentation of performance, the necessity for change (performance variations), and results when changes are implemented (evaluation of effectiveness). A suggested means for completing such assessment may be accomplished through the identification of three to four clinical measures and a fiscal measure to focus on as performance initiatives for the year and the incorporation of the Plan, Do, Study, Act (PDSA) evaluation process for the implementation of appropriate action plans, identifying those responsible, and providing timelines for follow-up reflected in the QI Minutes. The QI Plan must delineate all QI activities for the year so as to enhance the completion of QI activities and the health center must clearly document these activities in the QI Committee Meeting Minutes. Section 3. Management and Finance - Program Requirement #9 Program Requirement #9 - Key Management Staff Health center maintains a fully staffed health center management team as appropriate for the size and needs of the center. Prior approval by HRSA of a change in the Project Director/Executive Director/CEO position is required. (Section 330(k)(3)(I) of the PHS Act, 42 CFR Part 51c.303(p), and 45 CFR Part 74.25(c)(2)-(3)) Compliance Status: Met. Documents reviewed onsite or in advance: Health center Organizational Chart Key Management Staff position descriptions and biographical sketches UDS Summary Report Compliance Review Findings: 23 of 38 XXXX is a large organization with approximately 350 employees. The Key Management Staff is appropriate to the size and complexity of the organization. As reflected on the most recent Organization Chart, the Key Management Staff consists of the CEO, COO, CMO, CFO, CIO and the Chief Compliance Officer. The CEO has been in that position for the last 12 years. With the exception of the CIO, the Key Management Staff have longevity of tenure. The Key Management’s resumes indicate expertise and experience commensurate with their responsibilities as expressed in their job descriptions. In addition to having a fully-staffed management team, there is evidence of succession planning. Subordinate staff members are being trained to take on progressive additional duties to equip them to move into management roles as opportunities become available. Section 3. Management and Finance - Program Requirement #10 Program Requirement #10 - Contractual/Affiliation Agreements Health center exercises appropriate oversight and authority over all contracted services, including assuring that any subrecipient(s) meets Health Center Program requirements. (Section 330(k)(3)(I)(ii) of the PHS Act, 42 CFR Part 51c.303(n) and (t), Section 1861(aa)(4) and 1905(l)(2)(B) of the Social Security Act, and 45 CFR Part 74.1(a)(2)) Compliance Status: Met. Documents reviewed onsite or in advance: Procurement and/or other policies and procedures that support oversight of contracts or affiliations Compliance Review Findings: XXXX has Board-approved policies that assure the appropriate oversight and procurement over contracted services, including provisions for the monitoring and evaluation of contracted services. None of the health center’s contracts have the potential to limit its authority or compromise the health center’s ability to comply with HRSA’s Health Center Program Requirements. XXXX maintains an electronic system to track the status of its contracts with outside vendors including the name of the contract, the nature of the contract, the dollar amount, the expiration date (if applicable), and the staff person responsible for managing the contractual arrangement. Section 3. Management and Finance - Program Requirement #11 Program Requirement #11 - Collaborative Relationships Health center makes effort to establish and maintain collaborative relationships with other health care providers, including other health centers, in the service area of the center. The health center secures letter(s) of support from existing health centers (section 330 grantees and FQHC LookAlikes) in the service area or provides an explanation for why such letter(s) of support cannot be obtained. (Section 330(k)(3)(B) of the PHS Act and 42 CFR Part 51c.303(n)) 24 of 38 Compliance Status: Met. Documents reviewed onsite or in advance: Letters of Support Memoranda of Agreement/Understanding Compliance Review Findings: XXXX maintains strong collaborative relationships with other key stakeholders in the communities that it serves. XXXX is not engaged in a subreciepient relationship but does have a working relationship with the other FQHC in the surrounding area, as evidenced by a Letter of Support. It was explained that the grantee’s organizational history required that the organization establish itself in the community and become recognized and accepted as an integral contributor to the welfare of those needing primary health care, thereby laying the groundwork for an organizational culture of collaboration and co-operation. Section 3. Management and Finance - Program Requirement #12 Program Requirement #12 - Financial Management and Control Policies Health center maintains accounting and internal control systems appropriate to the size and complexity of the organization reflecting Generally Accepted Accounting Principles (GAAP) and separates functions appropriate to organizational size to safeguard assets and maintain financial stability. Health center assures an annual independent financial audit is performed in accordance with Federal audit requirements, including submission of a corrective action plan addressing all findings, questioned costs, reportable conditions, and material weaknesses cited in the Audit Report. (Section 330(k)(3)(D) and (q) of the PHS Act and 45 CFR Parts 74.14, 74.21, and 74.26) Compliance Status: Met. Documents reviewed onsite or in advance: Most recent independent financial audit and Management Letter, including audit Corrective Action Plans based on prior year audit findings, if applicable Most recent A-133 Compliance Supplement (grantees only) Financial Management/Accounting and Internal Control Policies and Procedures Chart of Accounts Balance Sheet Income Statement Most recent Health Center Program required Financial Performance Measures/UDS Report Most recent Income Analysis (Form 3) Other: Unaudited financial statements for the fiscal year ended December 31, 2013 and the FY 2014 YTD period ended February 28, 2014. Compliance Review Findings: 25 of 38 The health center’s internal control systems are appropriate for organizational size and complexity, and permit the recording, tracking and accumulation of separately identified federal and nonfederal transactions, consistent with the budgeting and accounting requirements of PIN 2013-01. XXXX identifies transactions at a level that allows it to distinguish between the use of federal and non-federal resources that can then be compared to the approved budget. In practice, this is accomplished by allocating federal grant funds to personnel costs for a group of employees whose individual salaries are below the authorized ceiling for which section 330 grant dollars may be utilized. A comparative balance sheet is produced and monthly and year-to-date results are compared to budget each month to demonstrate adherence to the approved budget and to show variances from expected results at the overall level and for each health center location. Although the Finance Committee met only sporadically in the past year, the full Board receives a detailed financial statement each month, presented by the CFO. Monthly reporting includes an organization-wide consolidated financial statement and breakout line item detail by site to facilitate the Board’s ability to make informed decisions and to carry out fiduciary oversight functions designed to support financial stability. Twelve of 19 cost centers were posting an operating deficit as of XXXX XX, 2014 that totaled ($XXX,XXX) in aggregate, compared to a budget expectation of ($XXX,XXX). An independent audit is conducted each year that examines the adequacy of internal controls for protecting health center assets and compliance with GAAP, and also includes an A-133 compliance statement. The audit for 2012 identified no material weaknesses or significant deficiencies. Discussions with the audit firm preparing the 2013 financial statement that is expected to be available in approximately four weeks indicate there will also be no areas identifying a material weakness or significant deficiency. The organization’s last audit with a finding requiring corrective action was for 2011, resulting in a Board-approved Corrective Action Plan that satisfied the concern. The health center’s financial position has been improving overall, although its financial position remains comparatively weak. Liquidity continues to be an area that is improving as XXXX strives to increase the level of cash on-hand, up from eight days at the end of FY 2012 to just over 17 days as of unaudited February 28, 2014, which was the most recently produced financial statement at the time of the visit. Section 3. Management and Finance - Program Requirement #13 Program Requirement #13 - Billing and Collections Health center has systems in place to maximize collections and reimbursement for its costs in providing health services, including written billing, credit and collection policies and procedures. (Section 330(k)(3)(F) and (G) of the PHS Act) Compliance Status: Met. Documents reviewed onsite or in advance: Policies and procedures for credit, collection, and billing 26 of 38 Encounter Form(s) Most recent Income Analysis (Form 3) Managed care or any other third-party payor contracts Most recent Health Center Program required Financial Performance Measures/UDS Report Other: 2011 through 2013 UDS Reports Compliance Review Findings: XXXX accepts all forms of public and private health insurance coverage, including private insurance plans. Medicare and Medicaid provider numbers have been established for all sites, and separate cost-based rates are paid at most locations. Board-approved written policies have been established for billing, credit and collections. Efforts are made to collect on all accounts, as evidenced by collection performance. Efforts are made to collect what is owed from the patient on the day of service based on Board approved policies. Payment plans are offered to those who are unable to pay their fees, and fees may be waived in their entirety for patients experiencing an exceptional hardship also based on board approved policies and set criteria. The grantee’s 2013 collection performance exceeded the national collection average recorded in 2012 and overall collection performance by the organization is strong. An active outreach and enrollment effort is underway to facilitate patient participation in expanded Medicaid and the private insurance market. Section 3. Management and Finance - Program Requirement #14 Program Requirement #14 - Budget Health center has developed a budget that reflects the costs of operations, expenses, and revenues (including the Federal grant) necessary to accomplish the service delivery plan, including the number of patients to be served. (Section 330(k)(3)(D) and (k)(3)(I)(i) of the PHS Act and 45 CFR Part 74.25) Compliance Status: Met. Documents reviewed onsite or in advance: Annual budget Most recent Income Analysis (Form 3) Most recent Staffing Profile Other: Detailed monthly financial statements that include comparisons to budget Compliance Review Findings: XXXX maintains an annual budget that reflects the anticipated income and expense, and all sources thereof, necessary to accomplish its annual Service Delivery Plan. The most recent budget submission to HRSA includes a breakout of expected federal and non-federal expenditures. Budget controls help ensure the use of HRSA funds is in accordance with the approved budget by category and amounts. Drawdowns of the section 330 grant funds are done based on immediate 27 of 38 cash needs. The health center has developed additional code structure within its general ledger accounting system that enables it to distinguish federal transactions from all others. Section 3. Management and Finance - Program Requirement #15 Program Requirement #15 - Program Data Reporting Systems Health center has systems which accurately collect and organize data for program reporting and which support management decision-making. (Section 330(k)(3)(I)(ii) of the PHS Act) Compliance Status: Met. Documents reviewed onsite or in advance: Most recent UDS Report and UDS Health Center Trend Report Most recent Clinical and Financial Performance Measures Forms Clinical and financial information systems (e.g., EHR, practice management systems, billing systems) Compliance Review Findings: The health center has appropriate systems and procedures in place to satisfy HRSA reporting requirements for UDS, FFR and other management information needs, including the data needed for reporting health care and business plan measures required in annual grant renewal applications. The grantee’s practice management system has a module that supports UDS reporting for all required clinical measures and for the two UDS-based financial measures. With the rollout of the EHR system to all practice sites, XXXX is in a position to fully automate the reporting of UDS clinical measures. The primary information needed for reporting dental services is captured by entering data to support billing into the practice management system. Other required elements of the UDS are supplied by the combination of the payroll system that produces data needed for FTE calculation, and the general ledger accounting system, which has adequate code structure to permit income and expense to be tracked in detail for all health center locations and lines of service. XXXX has an extensive IT department that supports all routine and ad hoc reporting needs. The most recent UDS and FFR submissions were completed in a timely manner, and produced information that is used to support management decisions and evaluation of program accomplishments. Section 3. Management and Finance - Program Requirement #16 Program Requirement #16 - Scope of Project Health center maintains its funded scope of project (sites, services, service area, target population, and providers), including any increases based on recent grant awards. (45 CFR Part 74.25) Compliance Status: Not Met. Documents reviewed onsite or in advance: Health Center UDS Trend Report 28 of 38 Health center’s official Scope of Project for Sites and Services (Forms 5A, 5B, and 5C) Most Recent Form 2 - Staffing Profile Notice of Award and information for any recent New Access Point or other supplemental grant awards Compliance Review Findings: The organization’s newest site, XXXX was opened with NAP support awarded in November 2013 and began seeing patients in February 2014. It has been delayed in opening to full-time operations while awaiting state licensure that is expected to be awarded within the month. XXXX has hired a physician who currently works out of its XXXX location and who will relocate to the NAP site when licensure is awarded. His service capacity will be further increased by the hiring of additional provider staff as patient demand increases with the transition to full-time operations. The organization currently provides psychiatry services via contracted psychiatrists and the organization bills for these services. However, Form 5 A - Additional Services, does not reflect the provision of psychiatry services as a specialty service as required per PIN 2009-02, “Specialty Services and Scope of Services.” If Not Met - Steps/Actions Recommended for Compliance: XXXX must work with the Project Officer to submit a Change in Scope to include psychiatry services as a specialty service per PIN 2009-02. Section 4. Governance - Program Requirement #17 Program Requirement #17 - Board Authority Health center governing Board maintains appropriate authority to oversee the operations of the center. (Section 330(k)(3)(H) of the PHS Act and 42 CFR Part 51c.304) Compliance Status: Met. Documents reviewed onsite or in advance: Organizational/corporate bylaws Minutes of recent Board meetings Health center policies and procedures List of Board Committees Other: Board orientation materials, Strategic Plan, Board Self-Evaluations, senior management reports to the Board Compliance Review Findings: 29 of 38 XXXX has a rich history of 43 years of service to the community. The health center was started by a core group of volunteers who identified the need for health care services in the region. Current Board members demonstrate a deep commitment to the organization. The XXXX Board is fully engaged in the execution of its Board Authority as evidenced by the following: Approval of grant applications and budgets; Monthly Board meetings with written minutes documenting those meetings and major decisions made by the Board; The annual evaluation of the CEO, which in the most recent evaluation included a comparative analysis of the compensation package offered to the XXXX CEO as compared to similar health centers in the state; The approval of the expansion of services and locations and hours of operations as documented in the minutes; The adoption of a four-year Strategic Plan for the organization; Measuring the overall progress of XXXX through various metrics, as reported to the Board by the senior staff including patient satisfaction; Measuring its performance as a Board via an annual self-evaluation process; Approval of policies (fiscal, clinical, administrative); and Adoption of bylaws that, amongst other things, address: the health center’s mission; Board authorities; membership size and composition; Board member responsibilities; process for selection and removal and election and terms of office; monthly meetings and quorum requirements; and a provision regarding conflict of interest. Section 4. Governance - Program Requirement #18 Program Requirement #18 - Board Composition The health center governing Board is composed of individuals, a majority of whom are being served by the center and, this majority as a group, represents the individuals being served by the center in terms of demographic factors such as race, ethnicity, and sex. (Section 330(k)(3)(I) of the PHS Act, 42 CFR Part 51c.303(p), and 45 CFR Part 74.25(c)(2)-(3)) Compliance Status: Met. Documents reviewed onsite or in advance: Composition of Board of Directors/most recent Form 6A - Board Composition Organizational/corporate bylaws Board member application and disclosure forms UDS Summary Report Compliance Review Findings: XXXX has a Board comprised of 12 persons and seven (58%) of those members (or their dependents) are patients of the health center and have utilized the health center services within the past two years. As a group, the patient members of the XXXX governing body represent the individuals being served by the health center in terms of demographic factors such as race, ethnicity and sex. A total of 92% of the XXXX Board members are (ethnicity) and the remaining 30 of 38 are (ethnicity). A total of 54% of the Board members are females. There is one Board member who represents the homeless population. The bylaws state a range in the size from nine to 25. The nonconsumer Board members (as well as some of the consumer members) reflect expertise in finance, education, social services, banking, and law enforcement. No more than 50% of the non-consumer Board members derive more than 10% of their annual income from the health care industry. Section 4. Governance - Program Requirement #19 Program Requirement #19 - Conflict of Interest Policy Health center bylaws or written corporate Board approved policy include provisions that prohibit conflict of interest by Board members, employees, consultants, and those who furnish goods or services to the health center. (45 CFR Part 74.42 and 42 CFR Part 51c.304(b)) Compliance Status: Met. Documents reviewed onsite or in advance: Corporate Bylaws Most recent update of Conflict of Interest Policy and related procedures Procurement Policies and Procedures Compliance Review Findings: Article IV, Section 12 of the XXXX bylaws states that, “No member of the Board of Directors shall be an employee of the corporation, or spouse or child, parent, brother, sister by blood or marriage of such an employee,” and that the CEO is not a voting member of the Board. Section 3.4 of the Employee Manual addresses the preclusion of Conflict of Interest amongst the XXXX employees. While the Program Requirement is already met, it is anticipated that at the XXXX 2014 Board meeting, the XXXX governing body will adopt a Conflict of Interest Policy that will locate, in a single document, a comprehensive corporate Conflict of Interest Policy. Section 5. Clinical and Financial Performance Clinical Measure #1 - Percentage diabetic patients whose HbA1c levels are less than 7 percent, less than 8 percent, less than or equal to 9 percent, or greater than 9 percent. Documents reviewed onsite or in advance: UDS Trend, Comparison, and Summary Reports Quality Improvement/Quality Assurance Plan Clinical and Financial Performance Measure Forms from most recent SAC/Designation Application Clinical Performance Analysis: Reason(s) for selecting the measure: 31 of 38 Data for the analysis of this measure was taken from the 2010 – 2012 UDS Trend Report. The grantee’s Health Care Plan reflects a projected goal of 60% for this measure. State of XXXX UDS data reflects 68% of the total diabetics in CHCs achieved this measure in year 2012. The national average for all CHCs for this measure is 70% in year 2012. The Healthy People 2020 goal for this measure is 85.4%. Based on the analysis of data, XXXX has experienced a negative trend of approximately 120% over a three-year period from years 2010 through 2012. Other than year 2010, the grantee has not achieved the state or national averages or the Healthy People 2020 goal. Performance measure status and trend: Key factors (internal and external) contributing to and/or restricting the health center’s performance on the measure: Based on discussions with the CMO and the QI Program Director and a review of chart audit information for various clinic sites, the organization appears to consistently check records and records the percentage of patients who are meeting this measure. However, documentation in the QA Meeting Minutes does not support any organized methodology for formulating strategies and action plans or evaluative methodologies (e.g. PDSA cycles) for the continuous improvement of this measure that could be utilized throughout the sites for uniform improvement. Health center’s in-process and/or proposed action to improve performance on the measure: As part of the QA Program, the grantee should consider utilizing this measure as a performance initiative to ensure a concerted effort is underway to develop, implement and evaluate action plans for improvement of this measure, making the necessary adjustments at all sites to enhance improvement throughout the program. Clinical Measure #2 - Percentage of patients age 5 to 40 years with a diagnosis of persistent asthma (either mild, moderate, or severe) who were prescribed either the preferred long term control medication or an acceptable alternative pharmacological therapy during the current year. Clinical Performance Analysis: 32 of 38 Reason(s) for selecting the measure: Data for the analysis of this measure was taken from the 2010 – 2012 UDS Trend Report. Actual data for this measure was not required until year 2011. The grantee’s Health Care Plan reflects a projected goal of 70% for this measure. State of XXXX UDS data reflects 75.8% of the total diabetics in CHCs achieved this measure in year 2012. The national average for all CHCs for this measure is 73% in year 2012. The Healthy People 2020 goal for this measure is not established based on a review of the Respiratory Disease Objectives specifically delineated under RD-7 at http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=36. Based on the analysis of data, XXXX has experienced a negative trend of approximately XX% over a twoyear period from years 2011 through 2012. XXXX has not achieved its personal goal or the state and national averages. Performance measure status and trend: Key factors (internal and external) contributing to and/or restricting the health center’s performance on the measure: Based on discussion with the CMO and QI Program Director and a review of chart audit information for various clinic sites, the organization appears to consistently check records and records the percentage of patients who are meeting this measure. However, documentation in the QA Meeting Minutes does not support any organized methodology for formulating strategies and action plans or evaluative methodologies (e.g. PDSA cycles) for the continuous improvement of this measure that could be utilized throughout the sites for uniform improvement. Health center’s in-process and/or proposed action to improve performance on the measure: As part of the QA Program, the grantee should consider utilizing this measure as a performance initiative to ensure a concerted effort is underway to develop, implement and evaluate action plans for improvement of this measure, making the necessary adjustments at all sites to enhance improvement throughout the program. 33 of 38 Financial Measure #1 - Change in Net Assets to Expense Ratio Documents reviewed onsite or in advance: UDS Trend, Comparison, and Summary Reports Most recent audit Clinical and Financial Performance Measure Forms from most recent SAC/Designation Application Other: Year-to-date financial statement for FYE December 31, 2014 (i.e., period ending February 28, 2014) Financial Performance Analysis: Reason(s) for selecting the measure: XXXX had experienced multiple years of operating losses and decline in fund balance prior to FYE XXXX XX, 2012, when it posted a small profit that equated to a XX% increase in net assets. Prior to that, it had withheld pay raises, furloughed employees, and taken other measures to align income with spending in the face of a drop-off in patient demand for services that further exacerbated financial challenges. The favorable change in financial performance that was noted in 2012 continued through the following year, for which the unaudited year-end change in net assets was $131,090, corresponding to an increase of XX%. It is important to health center survival that the small positive trend it has recorded for the past two years continue, and preferably increases, to support the growing needs of the organization as it expands into new underserved communities and patient groups. Performance measure status and trend: Audited financial statements for the organization are the official source data for this measure. They disclose a baseline measure for 2012 of XX% (i.e., $XX,XXX divided by $XX,XXX,XXX). The grantee’s goal for this measure was to maintain a ratio of XX% throughout the project. It has not yet attained that result, although FY 2013 draft audit results demonstrate positive change toward goal attainment. The first two months of operations in 2014 have produced a net deficit in financial performance equivalent to XX%, the loss being somewhat greater than budget expectations. Despite the operating loss posted to date for FY 2014, there are other signs of recovery indicative of a small improvement in financial position. For example, XXXX had a 2013 year-end current ratio of X.XX and had increased cash on-hand to XX days, as contrasted with FY 2012 results of .XX for current ratio, and XX days of cash. While moving in a favorable direction, the recovery that is underway appears to be in a fragile state. To illustrate, a loss in the ability to generate earned revenues (such as would be likely to occur if a provider suddenly left the organization or became incapacitated) could reverse the current positive direction of change. An unexpected expenditure to repair critical equipment or a 34 of 38 third payroll occurring within the month could exhaust cash on-hand, potentially forcing the organization to rely on debt. Provider coding practices and/or fees that were set below market value could impede the ability to optimize revenues from billable patient services. Key factors (internal and external) contributing to and/or restricting the health center’s performance on the measure: Some of the key factors supporting the organization’s ability to meet its XX% goal are: Adequacy of exam rooms to support needed patient volume; Effective use of direct patient support staff to free up provider time through task delegation; Patient access to affordable health care coverage through public or private plans, both for current and prospective new patients; Community awareness of the full range of health center services; Ability to retain a trained, proficient workforce; Scheduling practices and kept appointment rates; and Purchasing practices. Virtually everything a health center does and many of the things it does not choose to do impacts the ability to cover operating costs and to generate a net surplus that will fuel the increase in net assets. Health center’s in-process and/or proposed action to improve performance on the measure: XXXX is encouraged to offer providers and staff feedback on their performance relative to management expectations (such as patients per FTE and per hour, individual missed appointment rates, and percentage of FTE “earned” based on measured output). Administrative tools to facilitate this process were left with the organization for its optional use. Performance relative to an empirical methodology for calculating service potential was left with the organization. The grantee is further encouraged to review provider workspace and seek, in general, to schedule the use of providers and support staff in such a way as to afford them access to three exam rooms each. XXXX management plans to expand clinical space to augment service capacity and earned revenue volume. The additional economy of scale gained in this manner should support lower average cost per visit. The implementation of pay raises this year should aid retention efforts. XXXX is also encouraged to explore non-monetary ways to recognize staff achievements, such as methods discussed in an article published by the Health and Medicine Policy Research Group that was shared with the CFO. Developing scheduling templates that are based on individual provider failed appointment experience can produce meaningful improvements in provider utilization and the number of patients seen. Resources such as the state’s Discount Purchasing Programs may afford opportunity to reduce costs and increase profits. Coding training may be used to improve the ability to generate earned revenues. Implementation of fixed discounts in lieu of percentage discounts is also encouraged to support further improvement in collection rates for sliding fee patients. A PowerPoint presentation was left with the organization that explores roles and 35 of 38 responsibilities of staff throughout the health center to explore each of these areas for the potential to improve financial viability. Section 6. Capital and Other Grant Progress Review Capital Grant Program(s) Reviewed: Capital Development (CD) Program (C8A) Capital Development Immediate Facility Improvements (CD-IFI) Program (C8B) Documents reviewed onsite or in advance: Notice of Award for Capital Grant(s) Capital Project Budget Current status of capital project: XXXX was the recipient of funding under the HRSA Capital Development Grant Program for two projects. Neither project has been completed to date. One has a project period that is on the verge of expiring. The other is temporarily on hold, pending resolution of the available options discussed hereafter under “Key Factors.” The smaller of the two was the XXXX Clinic (Grant No. XXXXXX), for which the total budget was $XXX,XXX. The project period for completion of the activities this grant was XXXX X, 2012 through XXXX XX, 2014. Total expenditures to-date as of the time of the site visit were $XX,XXX and the outstanding unspent balance was $XXX,XXX. XXXX is seeking an extension to allow it additional time for completion of the project. The larger Capital Development Grant was for the XXXX Clinic (Grant No. XXXXXX), for which the award was $X,XXX,XXX. The project period for the larger grant was XXXX X, 2012 through XXXX XX, 2015, leaving time for completion of the work, but it has been interrupted for other reasons explained in the “Key Factors” section of the report. Expenditures to-date at the time of the site visit were $XX,XXX, and the unspent balance of funds was $X,XXX,XXX. Key Factors (internal and external) contributing to and/or restricting the completion of the project and the project timeline (e.g., significant updates or modifications to the awarded project such as change in physical location, change in design/layout of the project): The smaller of the two capital development projects, the XXXX initiative, got underway, and the original plan to renovate an aging modular building in order to convert it to clinical space was reevaluated after it was determined that more extensive work was needed and that the anticipated costs of the renovation would exceed budget expectations. Management became aware that the 36 of 38 cost of necessary work would exceed the value of the finished project. Thereafter, a revised Scope of Project was developed, proposing instead to purchase a new modular unit to replace the original. XXXX is awaiting approval of its request, which entails an extension of the project period to permit the funds to be spent in a manner consistent with the objective of increasing available clinical space. The XXXX Clinic expansion project was premised on the health center’s ability to raze an adjacent derelict building it purchased on an adjoining lot situated directly behind the clinic. The intent was to essentially double the square footage of clinical space and to create needed additional parking spaces on the site of the building that was to undergo demolition. The project came to an unexpected halt when it was determined that the structure XXXX had planned to tear down had some historical significance that was previously unknown to management. Grantee’s current or proposed actions to complete the project: As noted, XXXX is seeking HRSA approval to allow it to purchase a new modular unit to meet its objectives for the XXXX project, including an extension of the deadline for spending the needed funds. If the request is permitted, XXXX will proceed with the planned modular building purchase. Discussion remains underway with local officials to ascertain whether XXXX is going to be able to utilize the land it purchased behind the XXXX clinic in the manner intended; or if it must seek out a different solution to address its need for increased clinical space and parking. A resolution of the issues is expected to take place in the near future, clearing the way for the project to move forward. Section 7. Innovative/Best Practices NOTE Examples of documentation of best practices are from different health centers. Governance: The organization maintains an internet-based Board Portal where key Board information and other shared documents are posted. This system provides access for Board Members to board minutes, committee reports, and other relevant documents through a secure and easy to access system. Board members can access information remotely to support Board decisions and other information necessary for them to exercise ‘informed’ authority, as well as to stay abreast of recent developments, readily obtain historical information, and in general, stay connected with the health center. The portal also hosts the Board Master Work Plan and Calendar, which includes the full Board and Committee meeting calendar. The work plan plots out the entire year of meeting dates and key topics to be undertaken. Board Members can more readily update their personal calendars with board and committee meeting dates, thereby improving attendance/participation. 37 of 38 Clinical: The health center has developed a Health Maintenance flow sheet/Nursing Care checklist in the EMR to document care and collect data for the clinical measures needed to meet reporting requirements and Meaningful Use criteria. Individual performance on the clinical measures has been incorporated as an evaluation component of provider evaluations. Fiscal: The health center has developed an Excel software application to identify billing errors and deficiencies not found by the EHS billing management system software and the billing clearinghouse software. Many of these billing errors occur because of reimbursement issues related to the complexities of the health center’s services and billing for these services. Identification of errors prior to billing reduces the time and effort necessary to correct rejected claims and accelerates collection of claim dollars 38 of 38