2012_10-Reproduction..
advertisement

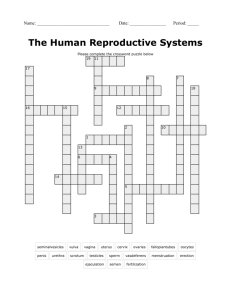
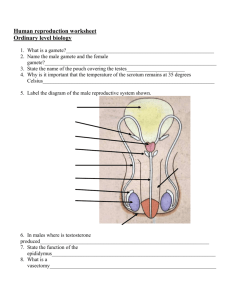
The Human Reproductive Systems Functions of the reproductive systems – To ensure that the sex cells, sperm and ova, are produced and are ready to fertilise each other. – To prepare the uterus to receive the fertilised egg and then modify the uterus as required as the embryo and then the foetus develop. – To ensure that the uterus goes through the processes which expel the baby and the placenta (afterbirth). Components of these systems Male: • • • • • • • • • Testis (_tes) Scrotum Epididymis (_mes) Vas deferens (vasa deferentia) Cowper’s gland (bulbourethral gland) Seminal vesicle Prostate gland Penis Sperm Female • Ovary (_ies) • Follicles (Corpus luteum) • Fimbriae • Oviducts (Fallopian tubes) • Uterus (and cervix) • Vagina • Clitoris The male system The male system Scrotum • The scrotum is very temperature sensitive to ensure that the testes are at the optimum temperature for sperm production. • Human body temperature is around 37oC. • Optimal sperm production is at 35oC. • The scrotum has many tiny muscles which adjust the testicular temperature by moving the testes closer to or further from the body. Testes • The testicle (from Latin testiculus), diminutive of testis, meaning "witness" [of virility], plural testes. • The sperm are produced in the seminiferous tubules. Epididymis • The epididymis (_mes) is a long and convoluted tube behind the testis. • About 100 million sperm are produced each day. • The sperm enter this tube in an immature form and could spend up to three months maturing. • The sperm will not have the capacity to fertilise an ovum until they have reached the uterus. Vas deferens • The vasa deferentia carry the sperm from the epididymes to the prostate gland just prior to ejaculation. Prostate gland • There are a number of glands that add “juices” to the sperm to make the semen. • These are: – Cowper’s gland or bulbourethral gland – Seminal vesicles – Prostate gland • These juices provide fluid, fructose and other components to ensure that the sperm can be transferred to the female and be able to survive long enough to fertilise the ovum. Prostate cancer • Most prostate cancers are slow growing; however, there are cases of aggressive prostate cancers. The cancer cells may metastasize (spread) from the prostate to other parts of the body, particularly the bones and lymph nodes. Prostate cancer may cause pain, difficulty in urinating, problems during sexual intercourse or erectile function. • the Gleason score is a helpful tool in classifying the stage and grade of prostate cancer. The Gleason score can range from 2 through 10. • Treatment options for prostate cancer with intent to cure are primarily surgery, radiation therapy (eg brachytherapy) and proton therapy. Penis • Besides urinating, the other main function of the penis is to deliver semen containing sperm to the female’s cervix. • The only way that this can be done effectively (naturally) is by having an erection. • For an erection to happen the spongy tissue in the penis must be engorged with blood producing a high hydrostatic pressure Ejaculation • Ejaculation occurs when the prostate gland contracts strongly a number of times releasing semen into the urethra. • It is at this stage that sperm delivered by the vas deferens to the urethra is mixed with the semen. • An ejaculate can vary between 2 mL and 10 mL with the average being about 5 mL (a teaspoon) and can contain up to 500 million sperm. • Sperm are so small that they occupy about 0.1% of an ejaculate. The female system The female system Ovaries • The ovaries – Produce two hormones (oestrogen and progesterone) that prepare the body for pregnancy, – Produce a follicle a month in which the ovum (egg) develops, – After ovulation the follicle becomes the corpus luteum which then produces progesterone. Polycystic Ovarian Syndrome • The causes of PCOS are unknown. In some cases, it seems to run in the family whereas for other women the condition only occurs when they are overweight. • • • • • • • Women who have PCOS may have problems such as: Irregular menstrual cycles – menstruation may be less frequent due to less frequent ovulation, and may be either heavier or lighter than average. Amenorrhoea – some women with PCOS do not menstruate, in some cases for many years. Obesity – the cause of this is unclear. Excessive hair growth – may be due to increased testosterone. Acne – the cause is unclear. Infertility – related to less frequent or absent ovulation. There may also be long-term health risks. Recent research suggests that PCOS is related to insulin resistance and the development of diabetes. Some women with PCOS develop diabetes, especially if they are overweight. Fimbriae • An ovary is not directly connected to its adjacent oviduct. When ovulation is about to occur, the sex hormones activate the fimbriae, causing them to swell with blood and hit the ovary in a gentle, sweeping motion. • An oocyte (ovum) is released from the ovary into the peritoneal (abdominal) cavity and the cilia of the fimbriae sweep the ovum into the Fallopian tube (oviduct). Oviduct • The oviduct (Fallopian tube) transports the oocyte (ovum) from the fimbriae to the uterus. • Fertilisation usually occurs in the oviduct about a third of the way from the ovary. • The fertilised ovum is called a zygote. Uterus • The uterus consists of a body and a cervix. The cervix protrudes into the vagina. The uterus is held in position within the pelvis by ligaments. • The reproductive function of the uterus is to accept a fertilised ovum. It implants into the endometrium, and derives nourishment from blood vessels which develop exclusively for this purpose. The fertilised ovum becomes an embryo, attaches to a wall of the uterus, creates a placenta, and, by 12 weeks, develops into a foetus (gestates) until childbirth. Implantation • This diagram shows the movement of the ovum, the zygote (first cell) and the dividing cells moving through the oviduct, into the uterus. • It is then implanted into the endometrium at about day 6. Endometrium • The endometrium is the lining of the uterus which changes its thickness according to the stage of the reproductive cycle. • These changes are controlled by the changing hormones. • The thickness ranges from about 6 mm to about 14 mm. Hysterectomy • Hysterectomy is the surgical removal of the womb (uterus), with or without the removal of the ovaries. • The conditions that may be treated by hysterectomy include: – Fibroids, which are non-malignant growths inside the muscular walls of the uterus. – Heavy or irregular menstrual periods. – Severe period pain, or dysmenorrhoea. – Cancer of the cervix, uterus or ovaries. – Endometriosis, a condition characterised by the migration of cells from the uterine lining to other areas of the body. – Prolapse, which means the uterus falls into the vagina because of loose ligaments or damage to the pelvic floor muscles. – Pelvic inflammatory disease (PID), caused by bacterial infection. Vagina • The vagina (from Latin vagĭna, literally “sheath" or “scabbard") is an elastic fibromuscular tubular tract leading from the uterus to the exterior of the body. • It can expand to be able to allow the birth of a baby. Clitoris • The clitoris is a sexual organ that is present only in female mammals. In humans, the visible button-like portion is located near the anterior junction of the labia minora, above the opening of the urethra and vagina. • The clitoris is much more extensive than most people imagine. • The penis and clitoris have the same embryonic origins. Conditions of the female reproductive system • • • • • • • Endometriosis Polycystic ovarian syndrome Ectopic pregnancy Pelvic Inflammatory Disease Cervical cancer Ovarian cancer Fibroid tumours Gestation Gestation First trimester • • • • • • In medicine, pregnancy is often defined as beginning when the developing embryo becomes implanted into the endometrial lining of a woman's uterus. The first two weeks of the first trimester are calculated as the first two weeks of pregnancy even though the pregnancy does not actually exist. The 5th week marks the start of the embryonic period when the baby's brain, spinal cord, heart and other organs begin to form. In the 6th week, the baby will be developing basic facial features and its arms and legs start to grow. In the 8th week, the baby starts moving and in the next three weeks, the baby's toes, neck and genitals develop. By the end of the first trimester, the foetus will be about 76 mm long and will weigh approximately 28 g. Second trimester • Weeks 13 to 28 of the pregnancy are called the second trimester. • By the 20th week the uterus can expand up to 20 times its normal size during pregnancy. • The placenta fully functions at this time and the foetus makes insulin and urinates. • The reproductive organs distinguish the foetus as male or female. Third trimester • The foetus grows most rapidly during this stage, gaining up to 28 g per day. • Movement of the foetus becomes stronger and more frequent and via improved brain, eye, and muscle function the foetus is prepared for ex utero viability. • Brain synapses begin forming at 17 weeks, and at about week 28 begin to multiply at a rapid pace which continues until 3–4 months after birth. Embryonic and foetal development Embryo at 4 weeks after fertilisation Embryo at 8 weeks after fertilisation Foetus at 18 weeks after fertilisation Foetus at 38 weeks after fertilisation Three stages of Birth