PT Consult Requests - UNM Hospitalist Wiki
advertisement

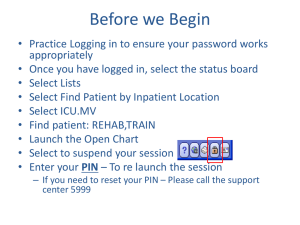
Inpatient PT Consults Lenny Noronha MD, Heidi Gober PT, Julie Rogers PT 11/11/15 UNM Hospitalist Best Practices Background • Inpatient PT consults are frequently ordered by IM ward teams • Discussion from HVC student modules generated interest in optimal use of inpatient PT services • I think hospitalists should know something about everything in the hospital…(personal opinion) Objectives By the end of this presentation, attendees will be able to: • Prepare ward teams and patients before PT consultation • Appreciate work load and communicate more effectively with PT • Chart • Phone • Consider things we can all do, even if chronically short-staffed Outline • Preview cases (2 min) • Review selected literature (6 min) • Overview of UNM Rehab Services (10 min) • Return to cases (10 min) • Questions/Discussion (15 min) Cases • 57ym on CIWA protocol getting to br c mod assist; homeless, no funding. No functional limitations at baseline • 82yf transferred from MICU to your team after 6d on vent for septic shock/CAP. Pt is on 8L nc. She has B severe knee OA, lives c son and d-i-l in Estancia. Son has forgotten to bring in her cane 3 times. It is Friday at 3:45pm. The PT note yesterday: “CGA/SBA, STS FWW” • Audience case Literature review “Time for critically ill patients to regainmobility after early mobilization in the intensive care unit and transition to a general inpatient floor”, Journal of Critical Care 30 (2015) 1238–1242, SarahM. Pandullo, ARNP, CCNS-BC a, Sarah K. Spilman,MA b,⁎, Janell A. Smith, RN, CCRN a, Lisa K. Kingery, RRT c, Sara M. Pille, PT, DPT d, Robert D. Rondinelli, MD, PhD e, Sheryl M. Sahr, MD, MS b • Retrospective review of 182pts transf from ICU to SAC • >48h in ICU (ave 4d) • Patients who walked in ICU more likely to walk on ward Interesting post-hoc analysis… Hopkins RO, Miller RR III, Rodriguez L, et al. Physical therapy on the wards after early physical activity and mobility in the intensive care unit. Phys Ther. 2012;92:1518–1523. • Prospective study of 72pts transferring from RICU to floor • 61 ambulated >100’ on last day in ICU Omission of Physical Therapy Recommendations for High-Risk Patients Transitioning From the Hospital to Subacute Care Facilities, Archives of Physical Medicine and Rehabilitation, Brock Polnaszek, BS, Jacquelyn Mirr, BS,Rachel Roiland, RN, PhD, Andrea Gilmore-Bykovskyi, RN, PhD,Melissa Hovanes, RN, Amy Kind, MD, PhDFrom the aDepartment of Medicine, Geriatrics Division, University of Wisconsin School of Medicine and Public Health, Madison, WI; • Retrospective review of 613 PT DC reccs • 3 Categories UH Rehab services overview • PT • Inpt/outpt • Wound • OT • ST Some Inpatient PT stats • Average 190 PT referrals/day for entire hospital unit # PT pts/day average % of unit 4W 17-24/d 20.3 51 3N 4-6 5 52 5W 11-18 14.6 55 PT teams PT, PTA PT • Eval • Plan of care • Goals • DC recc Physical therapy assistant • Ongoing tx • Communicate c PT Average 8 referrals/d • goal 5-6 visits Average 10-12 pts assigned/d • i.e. change DC recc • Goal 8 visits/d Inpatient PT consult request flow Order Printer Tech adds to Cache Cache list printed at 7am “Team lead” distributes pts Pre-Consult Chart • Activity order • PT consult order • VS (bp, O2) • Labs (H/H, plts) • Notes • Latest PN, HP, consults (ortho) • Text rendition: prev PT, CM, SW Hall • Bring new FWW & belt (single use) • Check in with nurse • Gown Consult rationale at UNM • Improve inpatient mobility • Change in level of care • Home services/facility placement • SNF • Acute rehab Communication • One-to-one PT training with new hire care management employees. • Participation in patient rounds/team conferences regarding discharge plans. • Contact (phone number) information exchanges between rehab and care management. • Utilization and updating patient white boards. • Hand-off information from ICU therapists to floor therapists regarding patients transferring to the floors. • Participation in weekly care management rounds for patients with extended LOS and short stays. Sample note language Assessment PT Assessment Summary : 6/22/15 5E Pt seen to improve functional mobility, transfers and ambulation. Pt presents w/multiple lines, decreased overall strength and activity tolerance, is HOH and using 6L O2. Pt's O2 sat ~85% w/functional mobility, requiring >2 min. to return WNL. Pt is ModA for bed mobility to EOB, CGA/SBA sitting EOB, ModA STS w/FWW. Pt is able to follow directions with VC/TC's and is participatory in therapy, but with decreased motor planning/execution. Pt is progressing toward PT goals and will continue to benefit from skilled interventions in order to maximize independence. DC Rec: Inpatient Rehab "6-clicks" score: OOB mobility not assessed Chalisa Glenn, PTA Referring PT, Julie Rogers, DPT Team cell: 385-3730 Pager: 951-0370 Treatment time: 30 min. Consult time: 30 min. Units: 2TA 3C DC Recommendations Recommend Discharge To: : Inpatient Rehab Glenn PTA, Chalisa - 06/22/2015 08:39 Plan Patient to Be Seen : 5-7 times per week May treatment be provided by PTA? : Yes Glenn PTA, Chalisa - 06/22/2015 08:39 Our DC to facility instructions SNF • Require 1 rehab service recc • Reccs should be updated within 72 hrs of transfer Acute rehab • Need 2 out of 3 rehab service reccs (PT/OT/ST) • Reccs updated within 48h Consult algorithm pocket card Return to cases • 57ym on CIWA protocol getting to br c mod assist; homeless, no funding. No functional limitations at baseline • 82yf transferred from MICU p 6d on vent for septic shock/CAP. She has B severe knee OA, lives c son and d-i-l in Estancia. Son has forgotten to bring in her cane 3 times. • 64yo bachelor c DM adm for spine OM req IV abx x 6wks. Dr. Imber will see in OPAT next week. Practices to consider • MICU accept patients • Observe & record sitting/standing • Assess home function, goals, motivation • Describe initial PT consult • DC to facility patients • Communication with PT team • Additional prompts for instructions (i.e. activity, assist, devices)