Constipation
advertisement

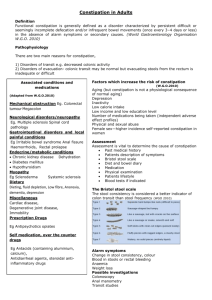
Constipation Constipation means different things to different people. For many people, it simply means infrequent stools. For others, however, constipation means hard stools, difficulty passing stools (straining), or a sense of incomplete emptying after a bowel movement. The cause of each of these "types" of constipation probably is different, and the approach to each should be tailored to the specific type of constipation. Constipation also can alternate with diarrhea. This pattern commonly occurs as part of the irritable bowel syndrome (IBS). At the extreme end of the constipation spectrum is fecal impaction, a condition in which stool hardens in the rectum and prevents the passage of any stool. The number of bowel movements generally decreases with age. Ninety-five percent of adults have bowel movements between three and 21 times per week, and this would be considered normal. The most common pattern is one bowel movement a day, but this pattern is seen in less than 50% of people. Moreover, most people are irregular and do not have bowel movements every day or the same number of bowel movements each day. Medically speaking, constipation usually is defined as fewer than three bowel movements per week. Severe constipation is defined as less than one bowel movement per week. There is no medical reason to have a bowel movement every day. Going without a bowel movement for two or three days does not cause physical discomfort, only mental distress for some people. Contrary to popular belief, there is no evidence that "toxins" accumulate when bowel movements are infrequent or that constipation leads to cancer. It is important to distinguish acute (recent onset) constipation from chronic (long duration) constipation. Acute constipation requires urgent assessment because a serious medical illness may be the underlying cause (for example, tumors of the colon). Constipation also requires an immediate assessment if it is accompanied by worrisome symptoms such as rectal bleeding, abdominal pain and cramps, nausea and vomiting, and involuntary loss of weight. In contrast, the evaluation of chronic constipation may not be urgent, particularly if simple measures bring relief. 1 Theoretically, constipation can be caused by the slow passage of digesting food through any part of the intestine. More than 95% of the time, however, the slowing occurs in the colon. Medications that cause constipation A frequently over-looked cause of constipation is medications. The most common offending medications include: Narcotic pain medications such as codeine (for example, Tylenol #3), oxycodone (for example, Percocet), and hydromorphone (Dilaudid); Antidepressants such as amitriptyline (Elavil) and imipramine (Tofranil) Anticonvulsants such as phenytoin (Dilantin) and carbamazepine (Tegretol) Iron supplements Calcium channel blocking drugs such as diltiazem (Cardizem) and nifedipine (Procardia) Aluminum-containing antacids such as Amphojel and Basaljel In addition to the medications listed above, there are many others that can cause constipation. Simple measures (for example, increasing dietary fiber) for treating the constipation caused by medications are often are effective, and discontinuing the medication is not necessary. If simple measures don't work, it may be possible to substitute a less constipating medication. For example, a nonsteroidal antiinflammatory drug (for example, ibuprofen) may be substituted for narcotic pain medications. Additionally, one of the newer and less constipating anti-depressant medications [for example, fluoxetine (Prozac)] may be substituted for amitriptyline and imipramine. Other causes of constipation Habit Bowel movements are under voluntary control. This means that the normal urge people feel when they need to have a bowel movement can be suppressed. Although occasionally it is appropriate to suppress an urge to 2 defecate (for example, when a bathroom is not available), doing this too frequently can lead to a disappearance of urges and result in constipation. Diet Fiber is important in maintaining a soft, bulky stool. Diets that are low in fiber can, therefore, cause constipation. The best natural sources of fiber are fruits, vegetables, and whole grains. Laxatives One suspected cause of severe constipation is the over-use of stimulant laxatives [for example, senna (Senokot), castor oil, and certain herbs]. An association has been shown between the chronic use of stimulant laxatives and damage to the nerves and muscles of the colon, and it is believed by some that the damage is responsible for the constipation. It is not clear, however, whether the laxatives have caused the damage or whether the damage existed prior to the use of laxatives and, indeed, has caused the laxatives to be used. Nevertheless, because of the possibility that stimulant laxatives can damage the colon, most experts recommend that stimulant laxatives be used as a last resort after non-stimulant treatments have failed. Hormonal disorders Hormones can affect bowel movements. For example: Too little thyroid hormone (hypothyroidism) and too much parathyroid hormone (by raising the calcium levels in the blood) can cause constipation. At the time of a woman's menstrual periods, estrogen and progesterone levels are high and may cause constipation. However, this is rarely a prolonged problem. High levels of estrogen and progesterone during pregnancy also can cause constipation. 3 Diseases that affect the colon There are many diseases that can affect the function of the muscles and/or nerves of the colon. These include diabetes, scleroderma, intestinal pseudo-obstruction, Hirschsprung's disease, and Chagas disease. Cancer or narrowing (stricture) of the colon that blocks the colon likewise can cause a decrease in the flow of stool. Central nervous system diseases Some diseases of the brain and spinal cord may cause constipation, including Parkinson's disease, multiple sclerosis, and spinal cord injuries. Colonic inertia Colonic inertia is a condition in which the nerves and/or muscles of the colon do not work normally. As a result, the contents of the colon are not propelled through the colon normally. The cause of colonic inertia is unclear. In some cases, the muscles or nerves of the colon are diseased. Colonic inertia also may be the result of the chronic use of stimulant laxatives as described above. In most cases, however, there is no clear cause for the constipation. Pelvic floor dysfunction Pelvic floor dysfunction (also known as outlet obstruction or outlet delay) refers to a condition in which the muscles of the lower pelvis that surround the rectum (the pelvic floor muscles) do not work normally. These muscles are critical for defecation (bowel movement). It is not known why these muscles fail to work properly in some people, but they can make the passage of stools difficult even when everything else is normal. What treatments are available for constipation? There are many treatments for constipation, and the best approach relies on a clear understanding of the underlying cause. 4 Dietary fiber (bulk-forming laxatives) The best way of adding fiber to the diet is increasing the quantity of fruits and vegetables that are eaten. This means a minimum of five servings of fruits or vegetables every day. For many people, however, the amount of fruits and vegetables that are necessary may be inconveniently large or may not provide adequate relief from constipation. In this case, fiber supplements can be useful. Fiber is defined as material made by plants that is not digested by the human gastrointestinal tract. Fiber is one of the mainstays in the treatment of constipation. Many types of fiber within the intestine bind to water and keep the water within the intestine. The fiber adds bulk (volume) to the stool and the water softens the stool. There are different sources of fiber and the type of fiber varies from source to source. Types of fiber can be categorized in several ways, for example, by their source. The most common sources of fiber include: fruits and vegetables, wheat or oat bran, psyllium seed (for example, Metamucil, Konsyl), synthetic methyl cellulose (for example, Citrucel), and polycarbophil (for example, Equilactin, Konsyl Fiber). Polycarbophil often is combined with calcium (for example, Fibercon). However, in some studies, the calcium-containing polycarbophil was not as effective as the polycarbophil without calcium. A lesser known source of fiber is an extract of malt (for example, Maltsupex); however, this extract may soften stools in ways other than increasing fiber. 5 Increased gas (flatulence) is a common side effect of high-fiber diets. The gas occurs because the bacteria normally present within the colon are capable of digesting fiber to a small extent. The bacteria produce gas as a byproduct of their digestion of fiber. All fibers, no matter what their source, can cause flatulence. However, since bacteria vary in their ability to digest the various types of fiber, the different sources of fiber may produce different amounts of gas. To complicate the situation, the ability of bacteria to digest one type of fiber can vary from individual to individual. This variability makes the selection of the best type of fiber for each person (for example, a fiber that improves the quality of the stool without causing flatulence) more difficult. Thus, finding the proper fiber for an individual becomes a matter of trial and error. The different sources of fiber should be tried one by one. The fiber should be started at a low dose and increased every one to two weeks until either the desired effect on the stool is achieved or troublesome flatulence interferes. (Fiber does not work overnight.) If flatulence occurs, the dose of fiber can be reduced for a few weeks and the higher dose can then be tried again. (It generally is said that the amount of gas that is produced by fiber decreases when the fiber is ingested for a prolonged period of time; however, this has never been studied.) If flatulence remains a problem and prevents the dose of fiber from being raised to a level that affects the stool satisfactorily, it is time to move on to a different source of fiber. When increasing amounts of fiber are used, it is recommended that greater amounts of water be consumed (for example, a full glass with each dose). In theory, the water prevents "hardening" of the fiber and blockage (obstruction) of the intestine. This seems like simple and reasonable advice. However, ingesting larger amounts of water has never been shown to have a beneficial effect on constipation, with or without the addition of fiber. (There is already a lot of water in the intestine and extra water that is digested is absorbed and excreted in the urine.) It is reasonable to drink enough fluids to prevent dehydration because with dehydration there may be reduced intestinal water. Because of concern about obstruction, persons with narrowings (strictures) or adhesions (scar tissue from previous surgery) of their intestines should not use fiber unless it has been discussed with their physician. Some fiber 6 laxatives contain sugar, and patients with diabetes may need to select sugar-free products. Lubricant laxatives Lubricant laxatives contain mineral oil as either the plain oil or an emulsion (combination with water) of the oil. The oil stays within the intestine, coats the particles of stool, and presumably prevents the removal of water from the stool. This retention of water in the stool results in softer stool. Mineral oil generally is used only for the short-term treatment of constipation since its long-term use has several potential disadvantages. The oil can absorb fat-soluble vitamins from the intestine and, if used for prolonged periods, may lead to deficiencies of these vitamins. This is of particular concern in pregnancy during which an adequate supply of vitamins is important for the fetus. In the very young or very elderly in whom the swallowing mechanism is not strong or is impaired by strokes, small amounts of the swallowed oil may enter the lungs and cause a type of pneumonia called lipid pneumonia. Mineral oil also may decrease the absorption of some drugs such as warfarin (Coumadin) and oral contraceptives, thereby decreasing their effectiveness. Despite these potential disadvantages, mineral oil can be effective when short-term treatment is necessary. Emollient laxatives (stool softeners) Emollient laxatives are generally known as stool softeners. They contain a compound called docusate (for example, Colace). Docusate is a wetting agent that improves the ability of water within the colon to penetrate and mix with stool. This increased water within the stool softens the stool. Although studies have not shown docusate to be consistently effective in relieving constipation. Stool softeners often are used in the long-term treatment of constipation. It may take a week or more for docusate to be effective. The dose should be increased after one to two weeks if no effect is seen. Although docusate generally is safe, it may increase the absorption of mineral oil and some medications from the intestine. Absorbed mineral oil collects in tissues of the body, for example, the lymph nodes and the liver, 7 where it causes inflammation. It is not clear if this inflammation has any important consequences, but it generally is felt that prolonged absorption of mineral oil should not be allowed. The use of emollient laxatives is not recommended together with mineral oil or with certain prescription medications. Emollient laxatives are commonly used when there is a need to soften the stool temporarily and make defecation easier (for example, after surgery, childbirth, or heart attacks). They are also used for individuals with hemorrhoids or anal fissures. Hyperosmolar laxatives Hyperosmolar laxatives are undigestible, unabsorbable compounds that remain within the colon and retain the water that already is in the colon. The result is softening of the stool. The most common hyperosmolar laxatives are lactulose (for example, Kristalose), sorbitol, and polyethylene glycol (for example, MiraLax). and are available by prescription only. These laxatives are safe for long-term use and are associated with few side effects. Hyperosmolar laxatives may be digested by colonic bacteria and turned into gas, which may result in unwanted abdominal bloating and flatulence. This effect is dose-related and less with polyethylene glycol. Therefore, gas can be reduced by reducing the dose of the laxative. In some cases, the gas will decrease over time. Saline laxatives Saline laxatives contain non-absorbable ions such as magnesium, sulfate, phosphate, and citrate [for example, magnesium citrate (Citroma), magnesium hydroxide, sodium phosphate). These ions remain in the colon and cause water to be drawn into the colon. Again, the effect is softening of the stool. Magnesium also may have mild stimulatory effects on the colonic muscles. The magnesium in magnesium-containing laxatives is partially absorbed from the intestine and into the body. Magnesium is eliminated from the body by the kidneys. Therefore, individuals with impaired kidney function may develop toxic levels of magnesium from chronic (long duration) use of magnesium-containing laxatives. 8 Saline laxatives act within a few hours. In general, potent saline laxatives should not be used on a regular basis. If major diarrhea develops with the use of saline laxatives and the lost fluid is not replaced by the consumption of liquids, dehydration may result. For constipation, the most frequentlyused and mildest of the saline laxatives is milk of magnesia. Epsom Salt is a more potent saline laxative that contains magnesium sulfate. Stimulant laxatives Stimulant laxatives cause the muscles of the small intestine and colon to propel their contents more rapidly. They also increase the amount of water in the stool, either by reducing the absorption of the water in the colon or by causing active secretion of water in the small intestine. The most commonly-used stimulant laxatives contain cascara (castor oil), senna (for example, Ex-Lax, Senokot), and aloe. Stimulant laxatives are very effective, but they can cause severe diarrhea with resulting dehydration and loss of electrolytes (especially potassium). They also are more likely than other types of laxatives to cause intestinal cramping. There is concern that chronic use of stimulant laxatives may damage the colon and worsen constipation, as previously discussed. Bisacodyl (for example, Dulcolax, Correctol) is a stimulant laxative that affects the nerves of the colon which, in turn, stimulate the muscles of the colon to propel its contents. Prunes also contain a mild colonic stimulant. Enemas There are many different types of enemas. By distending the rectum, all enemas (even the simplest type, the tap water enema) stimulate the colon to contract and eliminate stool. Other types of enemas have additional mechanisms of action. For example, saline enemas cause water to be drawn into the colon. Phosphate enemas (for example, Fleet phosphosoda) stimulate the muscles of the colon. Mineral oil enemas lubricate and soften hard stool. Emollient enemas (for example, Colace Microenema) contain agents that soften the stool. Enemas are particularly useful when there is impaction, which is hardening of stool in the rectum. In order to be effective, the instructions that come with the enema must be followed. This requires full application of the 9 enema, appropriate positioning after the enema is instilled, and retention of the enema until cramps are felt. Defecation usually occurs between a few minutes and one hour after the enema is inserted. Enemas are meant for occasional rather than regular use. The frequent use of enemas can cause disturbances of the fluids and electrolytes in the body. This is especially true of tap water enemas. Soapsuds enemas are not recommended because they can seriously damage the rectum. Suppositories As is the case with enemas, different types of suppositories have different mechanisms of action. There are stimulant suppositories containing bisacodyl (for example, Dulcolax). Glycerin suppositories are believed to have their effect by irritating the rectum. The insertion of the finger into the rectum when the suppository is placed may itself stimulate a bowel movement. Combination products There are many products that combine different laxatives. For example, there are oral products that combine senna and psyllium (Perdiem), senna and docusate (Senokot-S), and senna and glycerin (Fletcher's Castoria). One product even combines three laxatives, senna-like casanthranol, docusate, and glycerin (Sof-lax Overnight). These products may be convenient and effective, but they also contain stimulant laxatives. Therefore, there is concern about permanent colonic damage with the use of these products, and they probably should not be used for long-term treatment unless non-stimulant treatment fails. Miscellaneous drugs Several prescribed drugs that are used to treat medical diseases consistently cause (as a side effect) loose stools, even diarrhea. There actually are several small studies that have examined these drugs for the treatment of constipation. 10 Exercise People who lead sedentary lives are more frequently constipated than people who are active. Nevertheless, limited studies of exercise on bowel habit have shown that exercise has minimal or no effect on the frequency of bowel movements. Thus, exercise can be recommended for its many other health benefits, but not for its effect on constipation. 11