What to Screen? - Curriculum for the Hospitalized Aging Medical
advertisement

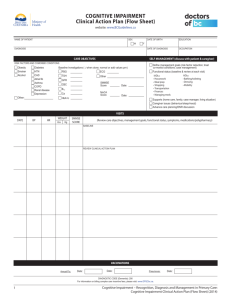
CHAMP The Hospitalized Frail Elder Teaching Strategies for Identification & Assessment Paula M. Podrazik, MD University of Chicago New Admission Mrs.G 80 y/o BF DM type II, htn, s/pCVA, OA, OP admitted for wt. loss, confusion, falls. Recently hospitalized at an outside institution. Meds: glipizide, lisinopril, lasix, asa, celebrex, fosamax q week Exam: Unkempt. A, O x 2 VS Afebrile BP 178/87 P 84 RR 16 Lungs clear, Cor RRR, Neuro non-focal ER evaluation—unremarkable blood work, CT head— no bleed Intern reports patient is at baseline per daughter and comments patient is just a “FTT.” Questions raised What is the importance of identifying frailty in the hospital setting? How do you recognize frailty ? How do you define frailty in the aging? What do you need to screen in the suspected frail patient during hospitalization? Aging patients & the hospital setting High rates of hospitalization Account for 47% of all inpatient days (but represent only 13% of the population) Age 85 and over, twice hospitalization risk High rates of readmission 25% of hospital admissions represent readmission of older adults Cost--outcomes Fethke CC, Smith IM, Johnson N. Medical Care. 1986;24:429-437 Graves EJ, Gillum BS. National Hospital Discharge Survey: annual summary, 1994. Vital Health Stat. 1997;13:128 Worse outcomes for hospitalized Older Adults Delirium Iatrogenic Complications Functional decline Nursing home placement Hospital readmission Caregiver stress Mortality Risk of rehospitalization—one outcomes look at frailty Age over 80 Inadequate social support Multiple active chronic health problems History of depression Moderate-severe functional impairment Multiple hospitalizations past 6 months Hospitalization past 30 days Fair or poor health self rating History of non-adherence to medical regimen Naylor M, Brooten D, Campbell, et al. JAMA. 1999;17:613-620 Hospitalization Outcome: The tension for the Hospitalized Aging Patient Baseline Frailty Hospitalization Outcome Acute illness Hazards of the Hospitalization Words that trigger the need to ID & teach about frailty Failure to thrive Dwindles Declining A/O x 1 or 2 Confused Poor historian Malodorous Recent discharge Unkempt Nursing home Weight loss Age 75 or over Non-compliant Needs assistance/ has caregiver Falls New Admission—Triggers to Teach ID/discuss frailty Mrs.G 80 y/o BF DM type II, htn, s/pCVA, OA, OP admitted for wt. loss, confusion, falls. Recently hospitalized at an outside institution. Meds: glipizide, lisinopril, lasix, asa, celebrex, fosamax q week Exam: Unkempt. A, O x 2 VS Afebrile BP 178/87 P 84 RR 16 Lungs clear, Cor RRR, Neuro non-focal Intern reports patient is at baseline per daughter and comments patient is just a “FTT.” Describe the Aging Population Heterogeneous Population Factors that contribute to heterogeneity Aging physiology Collected co-morbid conditions Functional status Functional Reserve of Older Adults Vision loss: 27% those over age 85 Cognitive impairment: 50% over age 85 Assistance w/ADL: > 50% over age 85 Functional reserve losses impact on an acute illness: Presentation Treatment Morbidity & Survival Recovery What is frailty? Being dependent on others Having many chronic illnesses Experiencing “uncoupling with the environment” Being at substantial risk of dependency & other adverse health outcomes Having complex medical & psychosocial problems Having “atypical” disease presentations Having many chronic illnesses Being able to benefit from specialized geriatric programs Experiencing accelerated aging Rockwood, et al. Can Med Assoc J 1994;150:489-95. Bortz WM. J AM Geriatr Soc 1993;41:1004-8. Fried L, et al. J Gerontol Medical Sciences 2001; 56A(3): M146-M156. Defining Frailty Definition must include: Association with aging Multi-system impairment Instability Change over time Allowance for heterogeneity within the population Association with an increased risk of adverse outcomes Rockwood K, et al. Drugs & Aging 200 Oct 17(4):295-302 ACOVE–a model to ID/define the Vulnerable Elder “in vivo” Assessing the Care of the Vulnerable Elder: ACOVE Project Overview Develop a definition of “vulnerable elders”— community dwellers, >65 & at high risk of functional decline or death Develop system to ID ID medical conditions for which effective methods of prevention& management exist Develop set of Quality Indicators Wenger NS, Shekelle PG, et al. Ann Int Med 2001;135(8) Supplement:642-646 Teaching about Frailty Triggers to teach about frailty in the aging hospitalized patient Advanced age Multiple co-morbidities Suspected cognitive impairment Suspected functional impairments Psychosocial issues Sensory impairments Frailty Suspected: Why to Screen? Prevention Impact on Outcomes Prognostic Index for 1-year Mortality in Older Hospitalized Adults 2 prospective studies—age> 70, assess 1-year mortality, points assigned—mortality risk calculated. Independent risk factors: Male sex #of dependent ADLs CA CHF Cr>3.0 Low albumin level Walter LC, et al. JAMA June 2001; 285(23):2987-2994 Comprehensive Assessment: Impact on outcomes Meta-analysis of Comprehensive Geriatric Assessment programs 28-controlled trials, 4959 subjects allocated to one of five CGA types and 4912 controls Outcomes: Mortality—GEMU programs 6 month mortality by 35%; HAS 36 month mortality by 14% Hospital admission—all CGA programs readmission rate by 12% OR for living @ home favorable in all studies Stuck AE, Siu AL, Wieland GD, et al. Lancet 1993; 342:1032-1036 Hospital Elder Life Program: A program of prevention Yale hospital system, ≥ age 70, admitted to acute care hospital Screened for cognitive impairment, sleep deprivation, immobility, dehydration, vision or hearing impairment Targeted interventions Outcomes Decrease in functional & cognitive decline Inouye S, et al JAGS 2000; 48:1697-1706 Teaching about Frailty: Summary teaching points Baseline vulnerability or frailty affects hospital outcomes High risk for worse outcomes Take measures to prevent delirium, falls, functional decline Identifying a vulnerable elder changes the needs of the D/C plan. Frailty Suspected: What to Screen? Cognition Function Affect Other Sensory function Social New Admission—Triggers to Teach Cognitive Screening Mrs.G 80 y/o BF DM type II, htn, s/pCVA, OA, OP admitted for wt. loss, confusion, falls. Recently hospitalized at an outside institution. Meds: glipizide, lisinopril, lasix, asa, celebrex, fosamax q week Exam: Unkempt. A, O x 2 VS Afebrile BP 178/87 P 84 RR 16 Lungs clear, Cor RRR, Neuro non-focal Intern reports patient is at baseline per daughter and comments patient is just a “FTT.” How common is dementia? Age strongest risk factor for dementia At age 65, prevalence 8-12% At age 85, prevalence 50% Persons with dementia in US- 4 million Projected number by 2040- 14 million Dementia and Delirium MMSE >24/30→ Delirium risk 2.82(1.19-6.65) Delirium associated with worse outcomes Orientation board and cognitive stimulation decreased confusion 26% vs. 8% * Confusion = loss of 2 points on MMSE Inouye SK, et al Ann Intern Med 1992;119:474-481 Cognitive Impairment & Functional Decline with Aging Cognitive impairment associated with functional decline during acute illness Study Design: Cognitive screen grouped admissions: No impairment Mild impairment Moderate/severe impairment ADL/IADL/mobility measured 2 weeks prior admission, discharge, 30 and 90 days. Sands L, Yaffe K, Covinski K, et al. Journal of Gerontology: Medical Sciences 2003;58:37-45. Cognitive status on admission & risk new NH placement at hospital D/C Cognitive status Rate/odds NH None 7.5% 1.0 Mild 13% 1.49(1-2.22) Moderate-severe 29% 3.40(2.48-4.68) Risk NH placement at 90 days after hospitalization vs. cognitive status Cognitive status None Mild Moderate-severe Rate/Odds NH 4.1% 1.0 11.7% 2.80(1.75-4.46) 26.7% 6.67(4.52-8.67) Screen for Cognitive Impairment: Summary Teaching Points Prevent delirium Prevent functional decline Prevent iatrogenic injury—esp. med choice & avoidance of restraints Transition care appropriately Screening Cognitive Impairment Patient measure: Mini Mental Status Exam (MMSE) Mini-cog Proxy measure Folstein MMSE 30 point screening test Screens multiple cognitive domains Not a direct screen of executive function Studies usually use cut off 24 for positive Reliability of results dependent on age & education Folstein M, Folstein S, McHugh P. J Psychiatr Res. 1975;12:189-198 Troubleshooting the MMSE Validation done under rigorous technique Serial 7’s vs. spelling WORLD backwards 8th grade education or < → WORLD >8th grade education→ serial 7’s Administer in quiet, non-threatening environment Correct sensory deficits as much as possible Reminders about MMSE Screening test for cognitive impairment Can help to risk stratify— delirium, functional decline, iatrogenic injury, pressure ulcers Useful as a baseline to monitor change Not a determination of decision-making capacity Screening Tools: Mini-cog Step 1:Remember & repeat three unrelated words Step 2: Clock-drawing test (CDT)—distracter Step 3: Repeat 3 previously presented words Step 4: Scoring:1 pnt. for each recalled word • • • • Score=0; + screen for dementia Score=1-2 with abnl CDT; + screen for dementia Score=1-2 with nl CDT; neg. screen for dementia Score=3; neg. screen for dementia Borson S, et al. Int J Geriatr Psychiatry2000;15:1021-1027 Screening Tests for Cognition: Summary Teaching Points Mini-cog—quick bedside tool MMSE—screening tool only If patient screens positive: Use orientation board Early mobilization Discharge plan—unique D/C needs Screen for functional, sensory impairments New Admission—Triggers to Teach physical function screening Mrs.G 80 y/o BF DM type II, htn, s/pCVA, OA, OP admitted for wt. loss, confusion, falls. Recently hospitalized at an outside institution. Meds: glipizide, lisinopril, lasix, asa, celebrex, fosamax q week Exam: Unkempt. A, O x 2 VS Afebrile BP 178/87 P 84 RR 16 Lungs clear, Cor RRR, Neuro non-focal Intern reports patient is at baseline per daughter and comments patient is just a “FTT.” Functional Screening: What are we talking about? Gait assessment Activities of daily living (ADL) Bathing Dressing Toileting Transferring Feeding Instrumental activities of daily living (IADL) Use telephone Manage finances Shop Arrange transportation Manage medications Cooking Functional Decline Occurs in the Hospital Functional limitations increase with age. Functional decline occurs in approx. 34-50% hospitalized older pts. Impact of acute illness Impact of hospitalization Interventions can decrease functional decline (Hospital Elder Life Program). Functional status determines D/C plan. Summary of functional outcomes during hospitalization At discharge→31% declined At 3 months→59% recovered lost function but 41% failed to return to pre-admission level of function At 3-months→ 22% re-hospitalized & association with functional decline significant Functional loss was associated with a significantly higher 3 month mortality Patient factors associated with functional decline older age preadmission functional impairment lower MMSE on admission re-hospitalization Sager M, Franke T, Inouye S, et al. Arch Intern Med. 1996;156:645-652. Worse health outcomes with functional decline Prolonged hospital stay Higher mortality—twice the risk Higher rates of institutionalization Higher health care expenditure Who is at risk functional decline during a hospital stay? Hospital based study @Yale Prospective cohort study Medical inpatients > 70 What are the risks for functional decline? Functional decline: ADL loss Two part study: Development and Validation Inouye S, Wagner R, Acampora D, et al. J Gen Intern Med. 1999;8:645-652. Independent risk factors associated with functional decline Risk Factor Pressure Ulcer Cognitive impairment Functional impairment Low social activity level Adjusted RR 2.7(1.4-5.2) 1.7(0.9-3.1) 1.8(1.0-3.3) 2.4(1.2-5.1) How does one assess functional status? Report Self-report Proxy report Direct observation Level of support Independent Needs assistance Dependent Activities of Daily Living Bathing Dressing Transference Continence Feeding Instrumental Activities of Daily Living Using the phone Traveling Shopping Preparing meals Housework Taking medicine Managing money Gait-timed Get Up and Go Quantitative evaluation of general functional mobility Timed command w/rise from chair; walk 10 feet; turn around; walk back and sit in chair. Wall JC, Bell C, Campbell S, et al J Rehabil Res Dev 200 37(1):109-113 Gait assessment scoring Usual time to completion 10 seconds Frail elder usually < 20 seconds > 20 seconds needs PT evaluation Performance on test associated with: ADL/IADL performance Falls risk Risk of nursing home placement Trigger to Teach: Who to screen for functional impairment? Who to screen? Person over the age of 70 Patient who is re-admitted in past month Person with at least 1 risk factor Cognitive impairment Functional impairment Pressure ulcer Low social activity score Depression Screen for function, cont. When to screen? After stabilization of acute illness Prior to hospital discharge What to do? Chart orders- walking and range of motion TID Ambulation problem- physical therapy Dressing/bathing/feeding- occupational therapy Function & the hospitalized elder: Summary teaching points Functional limitations increase with age Functional decline occurs in 30-50% of hospitalized older adults Acute illness can lead to further functional decline Hospital care can contribute to additional functional decline Models help stratify those at highest risk for functional decline Interventions decrease functional decline Functional abilities help determine discharge location and services required Questions raised What is the importance of identifying frailty in the hospital setting? How do you recognize frailty ? How do you define frailty in the aging? What do you need to screen in the suspected frail patient during hospitalization? New Admission Mrs.G 80 y/o BF DM type II, htn, s/pCVA, OA, OP admitted for wt. loss, confusion, falls. Recently hospitalized at an outside institution. Meds: glipizide, lisinopril, lasix, asa, celebrex, fosamax q week Exam: Unkempt. A, O x 2 VS Afebrile BP 178/87 P 84 RR 16 Lungs clear, Cor RRR, Neuro non-focal ER evaluation—unremarkable blood work, CT head— no bleed Intern reports patient is at baseline per daughter and comments patient is just a “FTT.” Frailty & the Hospital: A Final Word ID and teach about frailty Screen for cognition, functional status, psychosocial, sensory impairments Impairments associated with worse outcomes Prevention one key. The proper transition of care is the other. Special Thanks Joseph Shega Don Scott Aliza Baron Greg Sachs CHAMP faculty CHAMP faculty course participants