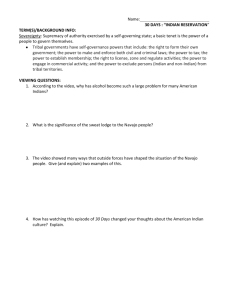
Comprehensive Geriatric Care of Elderly Native Americans
advertisement

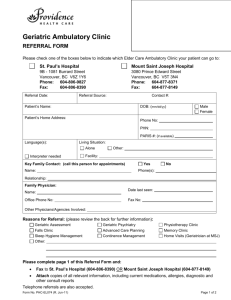
Comprehensive Geriatric Care of Elderly Native Americans Miriam E. Schwartz Department of Family Medicine Gallup Indian Medical Center (GIMC) Gallup, New Mexico 87301 Indian Health Service (IHS) • United States Department of Health and Human Services • The main federal health program for American Indians and Alaska Natives • Provides health services to about 1.8 million Native Americans who belong to approximately 557 federally recognized tribes in 35 states The Navajo Nation The Navajo Nation The Navajo Nation • Window Rock, Arizona – The Capital Gallup Indian Medical Center • Located in Gallup, New Mexico about 5 miles from the Navajo Nation border • Hospital with 99 beds • Clinical Specialties include – Family Medicine, Internal Medicine, Pediatrics, General Surgery, Orthopedics, ENT, Radiology, Pathology, Emergency Medicine, Psychiatry, Dental, OB/GYN Gallup Indian Medical Center • Serves mostly the Navajo Tribe Gallup Indian Medical Center • The workload at Gallup is one of the largest in the Indian Health Service • Enrolled number of patients – 43,000 individuals • Annually - 250,000 outpatient encounters and 5,800 inpatient admissions • The largest staff of all Navajo Area IHS facilities Nature of Problem • Prior to November 2007 - there was no organized geriatric care for the elderly patients at GIMC, but the need is great because our elderly population have unique characteristics given their cultural beliefs, traditions, and environmental situations. Mission and Vision of GIMC • Mission: We will provide health services with – Compassion Accessibility Respect Excellence Mission and Vision of GIMC • Vision: We value our patients and the community. We will work to see that they value us. We will generate the revenue to maximize services. We will use resources judiciously. We will support patient and family involvement, education, and decision making. We will have consistency between our plans and our actions. Results of Environmental Scan • Paucity of data about care of elderly Native Americans • Comprehensive Geriatric Assessment (CGA) and screening tools need to be modified to fit the culture and traditions of the target patient population Approach to the Problem • Geriatric Interdisciplinary Programs 1. 2. 3. 4. 5. 6. Comprehensive Geriatric Assessment Fall Risk Reduction Clinic Fall Injury Prevention Program Case Management of High Risk Patients Caregiver Support Financial Sustainability Target Population • How will you identify? – Patients are referred by Primary Care Physicians, Emergency Department Physicians, Urgent Care Clinic Physicians, and other Health Care Professionals. • Any unique attributes or cultural concerns? – Native American culture • Navajo Tribe (majority of patients) • Hopi • Zuni • Acoma – Traditional Medicine Process and Outcome Measures • Process – Comprehensive Geriatric Assessment – Fall Risk Evaluation • Outcome Measures – Next Slide • Collection of Data – Data Collector Process and Outcome Measures • Outcome Measures – – – – – – – Nursing Home Admissions Morbidity Rate Mortality Rate Health Benefits Functional Status Caregiver Burden Financial Sustainability Project Timeline • December 2008 • Data available for the following – – – – Morbidity Rate Nursing Home Admissions Functional Status Mortality Rate Project Timeline • June 2009 • In addition to the previous outcome measures • Data will be available for the following – Health Benefits – Caregiver Burden – Financial Sustainability Implementing the Program • The geriatric interdisciplinary program at GIMC is already at its nascent state. • Interdisciplinary team members – dental assistants, dietitians, nurses (case manager, podiatry & surgical), physical therapist, optometrist, physician assistant, and social workers. • There are no new opportunities onto which the program was attached. We started the program. Implementing the Program • Who are the key stakeholders? – – – – Department of Family Medicine Urgent Care Clinic Emergency Department Other Departments • How do you plan to engage them? – Meetings with chiefs of departments initially and asking for their suggestions – Implementation of these suggestions Perceived Facilitators/Barriers • Facilitators – Geriatric Interdisciplinary Team Members – Department of Family Medicine – Other Departments Perceived Facilitators/Barriers • Barriers – Integration of this new service line into the business structure of the institution – Negotiation of service agreements with other departments – Development of measures that show improvement in geriatric care and outcomes that are sustainable in a constrained fiscal environment – Local politics and bureaucracy in the institution – Some cultural aspects of care Preliminary Data Month Patients seen in CGA Clinic November 2007 No clinic yet Patients seen for Fall Assessment 4 December 2007 14 1 January 2008 4 6 February 2008 18 5 March 2008 9 5 Preliminary Data Month April 2008 Patients seen in CGA Clinic 8 Patients seen for Fall Assessment 4 May 2008 No clinic 5 June 2008 No clinic No clinic July 2008 10 5 August 2008 11 2 Preliminary Data Month Patients seen in CGA Clinic September 2008 6 Patients seen for Fall Assessment 6 October 2008 (7 scheduled) (23 scheduled) November 2008 No schedule yet No schedule yet December 2008 No schedule yet No schedule yet Total seen 80 43 Sustaining the Program • Meticulous accounting of billing and coding for the geriatric clinics - following the financial aspects of care will be absolutely necessary for our program What I Have Learned • Cultural sensitivity for the target population is important in any project. • Local politics and bureaucracy in the institution are significant factors in any project. • Engaging and motivating the key stake holders and participants are essential elements of any new project. References • Indian Health Service Web Site – www.ihs.gov • Source of Photos www.ihs.gov Thank you for your attention! Thank you very much for your support graciousness and encouragement !!!