File
advertisement

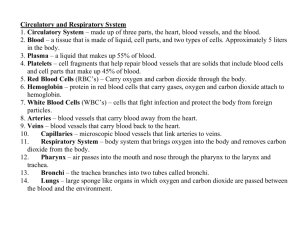
Occurs by bulk flow of gasses and by diffusion of gasses through tissue H6.1 Define partial pressure Dalton’s Law of partial pressure states that the total pressure exerted by a mixture of gasses is the sum of the pressures exerted independently by each gas in a mixture Furthermore, the pressure exerted by each gas, its partial pressure, is directly proportional to its percentage in the total gas mixture. Atmospheric pressure is approximately 760 mm Hg (760 torrs) at sea level and since air is a mixture of gases, we can look at it more closely in terms of the gases that make it up Partial pressures are calculated by multiplying the fractional composition of each gas in the air by the atmospheric pressure For example: PN2 = 760 x 79.02% = 600.6 mm Hg PO2 = 760 x 20.95% = 159.2 mm Hg PCO2 = 760 x 0.03% = 0.2 mm Hg ***different texts give slightly different partial pressures If there is a drop in air pressure, such as is seen at high altitudes, there is also a drop in the partial pressure of oxygen (pO2) Although the air at higher altitudes still contains 20.95% oxygen, the atmospheric pressure is less influenced by gravity, and results in a drop in ALL partial pressure values in proportion to the decrease in atmospheric pressure The saturation of oxygen is then lowered and thus, the amount of oxygen that is transported; the body compensates over time by increasing the number of red blood cells (We will talk about this again at a later date) H6.2 Explain the oxygen dissociation curves of adult and fetal hemoglobin and myoglobin • Molecular oxygen is carried in blood in two ways; bound to hemoglobin within rbcs and dissolved in plasma (only about 1.5%) • 98.5% of oxygen sent out from the lungs to tissues is carried in a loose chemical combination with hemoglobin • Each hemoglobin molecule can combine with 4 oxygen molecules; the process is rapid and reversible • Attachment of the first oxygen molecule changes the shape of Hgb allowing for faster attachment of the next 2 oxygen molecules and even faster attachment of the 4th, therefore, affinity of Hgb for oxygen changes with its state of saturation The hemoglobin-oxygen combination is called oxyhemoglobin and is written HbO2 Hemoglobin that has released oxygen is called reduced hemoglobin or deoxyhemoglobin and is written HHb Loading and unloading of oxygen can be indicated by a single reversible equation: lungs HHb + O2 ↔ HbO2 + H+ Tissues Materno-fetal respiratory gas exchange – showing the saturation of Hgb at various partial pressure of O2 Fig 1.4 Oxygen dissociation curves for human maternal and fetal blood, indicating the physiologic range of PO2 and O2 for mother and fetus. (Modified from Towell ME: Fetal respiratory physiology in Perinatal Medicine.1976 Edited by JW Goodwin, GW Chance: Longman; Toronto, Canada.) Although fetal partial pressure of oxygen is much lower, the saturation is relatively higher than in the adult. This is because fetal haemoglobin (75% - 80% of the haemoglobin at birth) has a greater affinity for oxygen than adult haemoglobin. The fetal oxy-haemoglobin dissociation curve is displaced to the left (see fig 1.4). Important shifts of the dissociation curves take place in the placenta. The maternal blood gains CO2, the pH falls and the curve shifts to the right releasing additional oxygen. On the fetal side of the placenta CO2 is lost, the pH rises and the curve shifts to the left allowing additional oxygen uptake (double Bohr effect).- the effect of pH on Hgb affinity for O2 *** Increased pH increased O2 uptake Decreased pH oxygen unloading Oxygen Dissociation Curves The graph illustrates what percent of the proteins present have bound O2 at a particular PO2 Figure 4·45 Oxygen-binding curves of myoglobin and hemoglobin. (from Horton et al 1996 "Principles of Biochemistry", Prentice Hall) • The fraction of each protein saturated with oxygen, Y, is plotted against the partial pressure of oxygen, pO2. • Myoglobin is an oxygen binding pigment in muscle • When hemoglobin carrying oxygen reaches the muscles, the oxygen is taken over and stored by myoglobin • To be able to do this, myoglobin must have a higher affinity for oxygen than hemoglobin (at equal pO2) but still be able to release oxygen when the muscles need it (during exercise) H6.3 Describe how carbon dioxide is carried by the blood, including the action of carbonic anhydrase, the chloride shift, and buffering by plasma proteins • Systemic capillaries deliver oxygen to the tissues and remove carbon dioxide • About 8% of CO2 in the blood is dissolved in plasma with another 20% bound to hemoglobin (carbaminohemoglobin) • Because carbon dioxide binds to the protein portion of hemoglobin and not to the heme irons, it does not compete with oxygen • It does, however, cause hemoglobin’s shape to change and thus, lowers its affinity for oxygen The remaining 72% of carbon dioxide diffuses into rbcs, where the enzyme carbonic anhydrase catalyzes the combination of carbon dioxide with water to form carbonic acid (H2CO3) (unstable) Carbonic acid dissociates into bicarbonate (HCO3-) and hydrogen (H+) ions The hydrogen ion binds to deoxyhemoglobin, and the bicarbonate moves out of the rbc and into the plasma via a transporter that exchanges one chloride ion for a bicarbonate (the chloride shift) This reaction removes large amounts of carbon dioxide from the plasma and facilitates the diffusion of additional carbon dioxide into the plasma from surrounding tissues Formation of carbonic acid is also important in maintaining the acid-base balance of the blood The bicarbonate acts as the major buffer of the blood plasma • Carbon dioxide is carried in the lungs in these forms •The lower pCO2 of the air inside the alveoli causes the carbonic anhydrase reaction to reverse direction, converting carbonic acid into water and carbon dioxide • The carbon dioxide diffuses out of the rbcs and into the alveoli, and leaves the body with the next exhalation H6.4 Explain the role of the Bohr shift in the supply of oxygen to respiring tissues • The Bohr effect is the release of oxygen by hemoglobin molecules in response to the surrounding elevated levels of carbon dioxide • The Hgb-O2 bond is weakened leading to increased oxygen unloading where it is needed • When carbonic acid dissociates into bicarbonate and hydrogen ions, pH is lowered • This lowered pH reduces hemoglobin’s affinity for oxygen, and oxygen is released more readily The effect of the lowered pH causes a shift of the oxyhemoglobin dissociation curve to the right Increasing temperature has a similar effect on hemoglobin’s affinity for oxygen Because skeletal muscles produce carbon dioxide more rapidly during exercise and active muscles produce heat, the blood unloads a high percentage of the oxygen that it carries to the tissues during exercise (See Fig. 44.33) Figure 4·49 Bohr effect. Lowering the pH decreases the affinity of hemoglobin for oxygen. (from Horton et al 1996 “Principles of Biochemistry”, Prentice Hall) The more energy the cells need, the more cellular respiration takes place and the more carbon dioxide is produced The increased carbon dioxide concentration will reduce the saturation of hemoglobin and release oxygen to the cells H.6.5 Explain how and why ventilation rate varies with exercise • During exercise, more oxygen is used and more carbon dioxide is produced • Each breath is initiated by neurons in the respiratory control center of the brain stem which sends impulses to the diaphragm and intercostal muscles, stimulating them to contract which expands the chest cavity resulting in inspiration • Although the breathing cycle is driven by neurons in the brain stem, the neurons must be able to respond to changes in blood pO2 and pCO2 in order to maintain homeostasis • A rise in pCO2 causes an increase in carbonic acid which dissociates to bicarbonate and hydrogen ions causing a drop in blood pH • This fall in pH, stimulates chemoreceptors in the aortic arch (aortic bodies) and at the bifurcation point of the common carotid arteries (carotid bodies) to send impulses to the respiratory center in the brain stem (medulla), which in turn, responds by increasing the breathing rate • Chemoreceptors in the brain do not respond to blood pH, but do respond after a brief delay, to increased carbon dioxide levels in the CSF H6.6 Outline the possible causes of asthma and its effect on the gas exchange system • Asthma is a chronic lung condition that is characterized by inflammation of the air passages in the lungs. • The condition presents with episodes of coughing, difficulty breathing, wheezing, and chest tightness, alone or in combination; often these episodes are accompanied by a sense of panic • Although hard to pin down, it is believed that asthma is caused by bronchospasms triggered by factors such as cold air, exercise, pollens, or other allergens, and viral illness • It has also been found that the bronchospasms have little effect on air flow through the lungs, and that inflammation of the bronchi usually occurs before the bronchospasms and that the inflammation is probably the result of an immune response • However, once airways are thickened with inflammatory exudate, the effect of bronchospasm is magnified dramatically, reducing air flow • Many asthma sufferers live in industrial areas H6.7 Explain the problem of gas exchange at high altitudes and the way the body acclimatizes • When you travel quickly from sea level to elevations above 8000 ft., where air density and pO2 levels are lower, your body responds with symptoms of acute mountain sickness which include headaches, shortness of breath, nausea, and dizziness; can lead to pulmonary and cerebral edema and may be fatal • When you move on a long term basis from sea level to the mountains, your body begins to make respiratory and hematopoietic adjustments in a process called acclimatization (stabilization occurs within 2-3 days) • When blood oxygen tension declines, the kidneys intervene by accelerating the production of erythropoietin, which stimulates bone marrow production of rbcs • Peripheral chemoreceptors are stimulated and the brain attempts to restore gas exchange to previous levels by increasing the ventilation rate • People living permanently at high altitude have greater lung surface area and larger vital capacity* than those living at sea level, and more red blood cells as well as a larger chest size *vital capacity: the volume of air that can be expelled from the lungs by forcible expiration after the deepest inspiration; total exchangeable air