Acid Base Simulations

Acid-Base Balance
H
2
O + CO
2
H
2
CA
CO
3
H
+
+ HCO
3
-
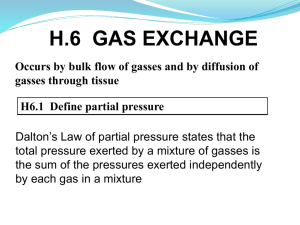
The purpose of this exercise is to simulate respiratory disturbances (which affect PCO
2
) and metabolic disturbances (reflected in the level of fixed acids) to observe how these disturbances affect the acid base balance of blood. In the body, the rate of the hydration reaction between dissolved CO
2
and water to produce the undissociated acid, H
2
CO
3,
is greatly accelerated by the presence of carbonic anhydrase (CA). This enzyme, present in red blood cells as well as some other cells of the body, greatly facilitates the rapid transfer of CO
2
from tissues to blood and from blood to exhaled air. The dissociation of
H
2
CO
3
into H + and HCO
3
can significantly alter blood pH because H+ is a strong acid.
When hydrogen ion concentration deviates too far from normal, these molecular effects show up clinically as abnormalities of organ function. Luckily, two buffer systems play dominant roles in buffering changes in hydrogen ion concentration in the body.
Hydrogen ion combines reversibly with bicarbonate ion to form carbonic acid (HCO
3
-
= a weak acid), which, in turn, is in equilibrium with carbon dioxide and water. The other buffer system is the blood protein system (Pr
-
) of which hemoglobin is the major component. The two systems may be viewed as contributing to the pool of total anion available for buffering.
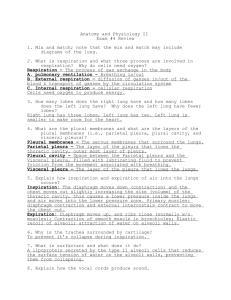
Exercises + Questions:
1. Simulate a metabolic disturbance by adding 10 mM/l of acid to the model system.
How are blood pH and HCO
3
- affected? EXPLAIN.
2. Define the Law of Mass Action. How does this law apply to the carbonic anyhydrase reaction pictured above?
3 Describe what happens when PCO
2
is increased above 40 Torr (how are ECF H+, pH,
HCO
3
- affected?) How does the increase in PCO
2
affect Pr-? Explain the changes using the Law of Mass Action. Describe a method of inducing such a change in the body (increasing PCO
2
) and how would you characterize (diagnose) this condition?
4.
Describe how the bicarbonate/carbonic acid reaction acts to buffer changes in H+ concentration (i.e. how does the CA reaction (above) shift to offset changes in H+ concentration? EXPLAIN. BE SPECIFIC. How does Hemoglobin offset changes in
H+ concentration?
Oxygen and Carbon Dioxide Dissociation Curves
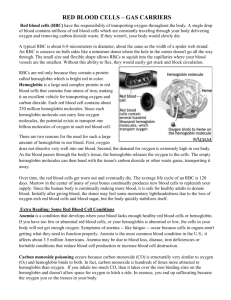
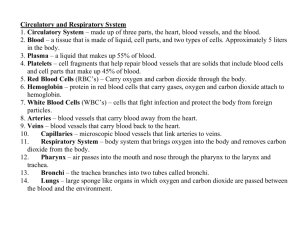
Tissue metabolism requires that oxygen be continually transported from the environment to the tissues and that carbon dioxide be continually transported from the tissues to the environment. The quantities of oxygen and carbon dioxide that can be dissolved in plasma, however, are not sufficient to sustain metabolism. Hemoglobin plays an important role in the process of gas movement between the environment and the tissues.
The quantity of oxygen bound to hemoglobin in normal arterial blood is greater than the amount necessary to supply the oxygen required for resting metabolism. Hence, the presence of hemoglobin provides a reservoir of available oxygen. In addition to its oxygen carrying properties, hemoglobin serves as a powerful buffering agent. When carbon dioxide is dissolved in an aqueous medium, it combines with water to form bicarbonate ion and hydrogen ion (a strong acid). By binding to H+, hemoglobin prevents H+ from contributing to large changes in blood pH.
The buffering and oxygen transport functions of hemoglobin are interrelated. Changes in blood hydrogen ion concentration affect the hemoglobin molecule so that blood having a higher hydrogen ion concentration enhances oxygen release (the Bohr Effect). Since changes in carbon dioxide affect hydrogen ion concentration, they also influence oxygen transport. As a corollary, the amount of oxygen bound to hemoglobin affects carbon dioxide transport. Deoxygenated hemoglobin is capable of accepting a larger number of hydrogen ions than is oxyhemoglobin. As a result, the ability of blood to carry carbon dioxide is increased as oxygen is released (the Haldane effect).
Several other factors also influence the binding of oxygen to hemoglobin (e.g., temperature), but these factors are not included in this simulation. This simulation allows you to examine how the factors such as PO2 and PCO2 influence hemoglobin’s affinity for oxygen and how the dissociation curve illustrate oxygen and carbon dioxide transport in the pulmonary and peripheral capillaries.
Exercises + Questions:
1. What is the shape of the oxyhemoglobin dissociation curve? How does the shape of the curve relate to the cooperative binding of O2? How does its shape influence loading of oxygen at the lung and unloading of oxygen at the tissue level? What causes oxygen movement into and out of the blood?
2. Use the model (gather data) to show how hemoglobin’s affinity for O2 changes as a function of PO2 and PCO2 at the lungs and the cells of working tissues. Why does hemoglobin’s affinity for O2 change at these two locations in the body?
3. The level of carbon dioxide in the blood affects the oxygen carrying capacity of hemoglobin in two ways. Describe the dual effect of CO2 on Hb.
4. Collect data (at least 5 data points) to construct an oxyhemoglobin dissociation curve
(Hb-O2 saturation as a function of PO2). Construct the curve in your laboratory notebook or in Excel and hand in this graph at the end of the laboratory period.