RT 254 Exam 1 Review
advertisement
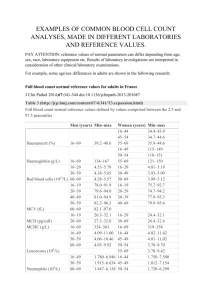
Exam 1 Review Cardiopulmonary Symptoms Physical Examination Clinical Laboratory Studies WBC Count Differential A patient had been admitted to the hospital for acute shortness of breath. A CXR examination reveals pneumonia and the patient’s temperature is elevated. The CBC shows an increased WBC of 15,000/mm3 with 75% neutrophils but only 10% lymphocytes. Given that the normal lymphocyte differential is 20-45%, does the value of 10% suggest a problem with lymphocyte production by the immune system? What type of pneumonia is probably present in this case? The 10% differential for the lymphocytes represents a relative value. Because the total WBC is markedly elevated, the 10% in relative terms represents 1500 lymphocytes in an absolute value, which is well within the normal range. If the total WBC were reduced to less than normal and the differential demonstrated a lymphocyte count of 10%, an abnormal value would be present and would suggest an immunological problem. The patient probably has bacterial pneumonia given the elevated number of neutrophils. Water, Salt and CHF Why do patients who have CHF need to adhere to a low-salt diet? The volume of extracellular water partially determines the preload of the ventricle – Na+ is an important determinant of extracellular volume. In CHF the left ventricle has failed as a pump, leading to pooling of the blood in the lungs and venous circulation. By restricting salt intake, extracellular volume can be reduced, allowing the heart to function more effectively as a pump. Diuretics are often used to help reduce fluid volume. Bedside assessment of the postoperative patient The RT is called to the floor too see a 54year old female who had abdominal surgery 2 days ago. She is currently complaining of dyspnea. Her resting RR is 34 and shallow. Her HR is 110. She is 5’ and weighs 185lbs. During the brief interview, the RT identifies that the dyspnea has gradually increased over the last 12hrs and increases with exertion. During auscultation, the RT identifies diminished breath sounds with some fine late inspiratory crackles. The remainder of the physical examination is normal. What is the most likely cause of this patient’s dyspnea and what should be done? The findings indicate a loss of lung volume as the cause of the sudden dyspnea. The rapid, shallow breathing; fine late inspiratory crackles and history of recent abdominal surgery suggest atelectasis. The RT should verify with a CXR and begin hyperinflation therapy if confirmed Sudden onset of chest pain The RT is called to the ED to see a 47year old man who came in with anxiety and chest pain. He is certain he is having a heart attack and demands immediate treatment. The attending MD is on his way and asks the RT to assess in the meantime. What do you do? Place the patient on oxygen, asks him for details about the chest pain The pain is located laterally on the left side and increases with each inspiratory effort, vital signs are normal except for a slight increase in heart rate. What is the most likely cause of the chest pain and what should be done until the MD arrives? In this case the pain is pleuritic, the RT should continue oxygen therapy, ensure the cardiac leads are attached to rule out any heart disease. Evidence of Tissue Hypoxia The RT is called to the ICU to see a new patient in septic shock. The patient complains of having dyspnea and fever for the last 3 days. His vital signs are: HR 100, RR 24, BP 80/65, body temp below normal. The patient is alert but confused, and his sensorium has deteriorated over the last 12 hours. Auscultation reveals fine crackles in the bases bilaterally and no murmurs or gallop rhythm. There is no evidence of cyanosis, pedal edema, or JVD. Capillary refill is 3 seconds and his extremities are warm to the touch. What suggests that this patient has hypoxia? The patient’s sensorium shows that the brain is not getting enough oxygen, probably due to poor circulation. Terminology for Adventitious Lung Sounds The RT is auscultating a patient who has severe pneumonia in the ICU . He hears a low pitched discontinuous sounds with inspiration and expiration. How should he document these? Coarse crackles, indicating that excessive airway secretions are present. Case Study 1 CBC results normal WBC 19.5 4.5-11.5 A 22 year old white woman is RBC 4.2 4.2-5.4 Hb 10.6 11.5-15.5 brought to the ED by her mother with chief complaints of cough, fever, and normal BP. She has a history of Down syndrome and lives at home with her parents. Initial examination reveals tachycardia, tachypnea, and fever; chest auscultations identifies bronchial breath sounds and inspiratory and expiratory coarse crackles over the right lower lobe. The admitting physician orders a sputum Gram stain and culture, CBC and chest x-ray. The initial laboratory results are as follows: Hct34.9% 38-47% MCV 77.0 80-96 MCHC 30.4% 32-36% WBC Differential results normal Neutrophils 82% 40-75% Lymphocytes 8% Monocytes 4% 0-6% Eosinophils 1% 0-6% Basophils 0% 0-1% Bands 6% 0-6% 20-45% Gram Stain 2+ gram positive cocci; 1+ pus cells with many epithelial cells Case study 1 solution Leukocytosis is present and appears to be the result of an increase in the neutrophils consistent with a bacteria infection (probably pneumonia). The slight increase in immature neutrophils (bands) represents a left shift indicating stress on the bone marrow to release more neutrophils to fight the infection. The relative decrease in the percentage of lymphocytes is caused by the absolute increase in the number of neutrophils and is not an abnormality. The RBC count is within normal limits; however the decreases in Hb, Hct, MCV, and MCHC are consistent with a microcytic, hypochromic anemia. Further investigation is needed to identify the cause, but iron deficiency anemia is a likely reason. The Gram stain of the sputum sample indicates that is was heavily contaminated with secretions from the mouth because many epithelial cells were present. The sample should be discarded and another sputum sample obtained. Common causes of pneumonia Streptococcus pneumoniae Staphylococcus aureus Klebsiella pneumoniae Haemophilus influenzae Case Study 2 A 65 year old woman arrives to the ED complaining of severe shortness of breath, weakness and cough. She has a long history of COPD and 90pack year smoking history, She currently admits to smoking 1pack/day. In the ED she appears acutely and chronically ill and is found to be using her accessory muscles to breathe. She is cyanotic and has decreased breath sounds bilaterally. She is started on O2 by NC and a CBC and electrolyte determination is ordered. The results are as follows: CBC results normal WBC 19.9 4.5-11.5 RBC 5.1 4.2-5.4 Hb 15.8 11.5-15.5 Hct 48.5% 38-47% MCV 98.2 80-96 MCHC 31.6% 32-36% WBC Differential results normal Neutrophils 76% 40-75% Lymphocytes 12% 20-45% Monocytes 5% 0-6% Eosinophils 4% 0-6% Basophils 2% 0-1% Bands 1% 0-6% Na+ 137 137-147 K+ 4.8 3.5-4.8 Cl- 87 98-105 Total CO2 41 23-33 Electrolytes Case study 2 solution The increase in WBC suggests leukocytosis and appears to be the result of an increase in the number of circulating neutrophils. This may be in response to a bacterial infection or acute stress. The RBC count, Hb, and Hct are slightly increased, consistent with polycythemia. These RBC differential findings are consistent with secondary polycythemia typical for patient with a chronic lung disease in which the arterial blood oxygen levels are persistently low. The electrolyte values reveal a decreased serum Cl- and increased serum CO2. This probably is related to the COPD and CO2 retention. Due to the increased HCO3- the kidneys excrete more Cl- in an effort to maintain electrical neutrality. Case Study 3 A 27year old man has a CD4 count of 120. He is concerned about his chronic cough and sputum production. The sputum has been negative for white cells and bacteria. A PPD skin test was placed on his right forearm 2 days ago and now there is a 3-cm reddened area and a 5mm nodule at the site. Initial laboratory data results are as follows: CBC results normal WBC 5.0 Neutrophils 70% 40-75% Lymphocytes 20% 20-45% Monocytes1% 0-6% Eosinophils 4% Basophils 0% 0-1% Bands 5% Hb 14 4.5-11.5 0-6% 0-6% 13.5-16.5 Hct 42% 40-50% Sedimentation rate 40 (elevated) Case study 3 solution The low CD4 count suggest moderate immunocompromise most likely caused by HIV. The elevated sedimentation rate suggests inflammation, which could be caused by TB or other infection. The large area of redness around the skin test site is not significant, but the nodule in this immunocompromised patient indicates a TB infection. This patient’s CBC is normal despite his chronic infection and because TB does not usually cause an elevated WBC count. We anticipate the sputum cultures will be positive in 6 weeks and a PCR test for TB bacilli in the sputum to be positive. Case Study 4 A 20 year old man is brought to the ED by ambulance following a MVC. He complains of a stiff neck and left leg pain. Although he is upset and scared, he is conscious and able to move all extremities. Vital signs are normal except HR-110. His initial CBC is as follows: CBC results normal WBC 14.9 4.5-11.5 RBC 5.1 4.2-5.4 Hb 15.0 11.5-15.5 Hct45.5% 38-47% MCV 95.2 80-96 MCHC 33.6% 32-36% WBC Differential results normal Neutrophils 76% 40-75% Lymphocytes 12% Monocytes 5% 0-6% Eosinophils 4% 0-6% Basophils 2% 0-1% Bands 1% 0-6% 20-45% Case study 4 solution The RBC and indices are all normal. The elevated WBC count suggests possible infection, however the lack of fever and minimal presence of band on the white cell differential suggests otherwise. This is most likely a case of pseudoneutrophilia, where marginated neutrophils are released into circulation as a result of sudden stress. This type of neutrophilia is usually transient and resolves spontaneously in a matter of hours. Auscultation List three reasons why patients with emphysema may have diminished breath sounds. 2. Explain why patients with obstructive lung disease breathe with a prolonged expiratory time. 3. Explain why atelectasis causes late inspiratory crackles as opposed to early inspiratory crackles. 1. What is this? What is being examined?