Introductory Immunology

Introductory Immunology
Dr Lindsay Marshall
MB451, ext. 4017 e-mail: l.marshall@aston.ac.uk
Lecture timetable
All lectures Tuesday morning, 9am, Sumpner lecture theatre
Week Date Lecture topic
14 Jan 27 th Subject overview
15
16
17
Feb 3 rd The innate immune system
Feb 10 th B cells and antibodies
Feb 17 th Antigen presentation
18 Feb 24 th T cells and cytokines
19
20
21
March 3 rd Anatomy of the lymphoid organs
March 10 th Lymphocyte recirculation
March 17 th Immunopathology
Some useful text books:
Sompayrac. How the immune system works, 4 th ed., 2012.
Library class mark: 616.079 SOM
35 copies (+ 16 copies of 3 rd ed.)
Parham. The Immune System, 3 rd ed., 2009; 4 th ed. 2014
Library class mark: 616.097 PAR
29 copies in library
Todd & Spickett ‘Immunology’, 2010.
Library class mark: 576.80973 TOD
18 copies in library
Course assessment –BY1IM1
Good news…
No coursework
Bad news…
Continuous assessment:
5 multi-choice questions EVERY WEEK
Questions are available via Blackboard for 24 hours after the lectures (until 10 am
Wednesday morning)
These make up 40% of the module (you can PASS this module just by doing well on the continuous assessment…)
MORE good news…
Tests start next week!
A (very small) bit of bad news…
Final exam in May-June.
Closed book, 30 MCQ in 1 hour.
Quizzes on Blackboard
Log on to Blackboard as usual and select BY1IM1
Click on the “Quizzes” button
You can have up to 10 attempts at each quiz in the
24 hours that it is available
Only your BEST score will be counted
Aston Replay
All these lectures will be recorded via Panopto and available via
Aston Replay
So you can listen again as often as you like
You might still want to print out lecture slides before the lecture and add notes to them during the lecture, then you can recap areas that you didn’t understand first time round by listening to the recordings.
You SHOULD be able to pass the exam without loads of extra readingbut the only way you’ll get top marks (in anything) is if you are reading the text books in addition to making good lecture notes.
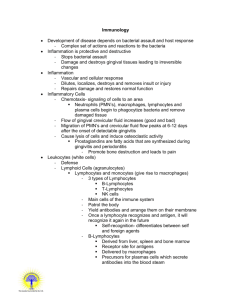
Immunology
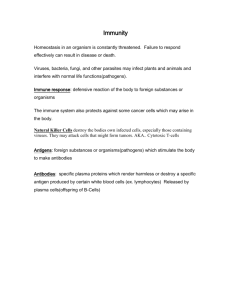
Immunity: from immunis ( Greek) meaning ‘exempt’
Immunity provides exemption (protection) from infectious disease
Why’s it so difficult?
(it isn’t really!)
Details…
Immunology is full of details and terminology and sometimes these get in the way of understanding
The purpose of this course is to…
1) introduce you to all of the cells, mediators and jargon associated with immunology and
2) to give you a basic understanding of how your immune system works so that we can build on this in future courses
Feel free to ask questionsthere’s no such thing as a “silly” question, if you have a question, chances are someone else is wondering the same thing!
You can… ask me during the lecture ask me after the lecture, l don’t mind e-mail me any time use the discussion board on BY1IM1, that way you can answer each other’s questions
The immune system and the Premier league
The immune response is a network of events, like a football match
In football, watching one player doesn’t give you the full picture of the match
For immunology, learning about one cell type doesn’t let you understand the entire immune response
This lecture is the overview or a quick tour of the whole immune system
Future lectures will look at each player in more detail – at the end of this module, we can put all the details together and we’ll understand exactly how and where the immune response works
The immune system has 3 components
1. Physical barriers
2. Innate immune response
3. Adaptive immune response
1. Physical barriers
First line of defence
Stop anything (pathogens) getting in
Skin
Mucous membranes (respiratory tract, GI tract)
2. Innate immune response
Second line of defence after physical barriers
Innate means ‘existing at the time of birth’
The case of the infected splinter
(or how your innate immune system works)
You step on a large splinter
This splinter is covered in bacteria (possibly pathogenic), which have now been given a free pass through the physical barriers (i.e. straight past the first line of defence) into the body
In a couple of hours you can see where the splinter went in – your skin is red and swollen and it hurts!
The redness, the swelling and the pain are all good - these are the signs of inflammation that show that your innate immune response
(second line of defence) is working
Macrophages to the rescue
Cells aren’t fixed, they can move around within your body, the
macrophages are the first cell type to defend against attack
Macro means BIG
Phage means EAT, so the macrophages are big, hungry cells that will devour the bacteria from the splinter in a process called “phagocytosis”
(cell-eating)
Macrophages eat anything
Macrophages eat invaders
Macrophages eat rubbish (cell debris)
Macrophages eat dead cells
Macrophages even eat iron filings…
Where do macrophages come from?
Haematopoiesis occurs in fetal liver and then the bone marrow
B lymphocyte
T lymphocyte
Natural killer (NK) cell
Bi-potential cell
Self-renewing stem cell
Macrophage
Neutrophil
Eosinophil
Mast cell
Megakaryocyte
Red blood cell (erythrocyte)
What do macrophages get up to?
Monocytes – “baby” macrophages
Two billion in circulation
Remain in the blood for about 3 days
Then they travel to the capillaries
They leave the blood, get into the tissues turn into macrophages and hang out, eating rubbish and watching out for bacterial invaders
Remember- monocytes in blood, macrophages in tissue
1.
What happens when the macrophages find an invader?
Phagocytosis
1.
2.
What happens when the macrophages find an invader?
Phagocytosis
Call for back-up
Increased blood flow to area (redness)
Increased tissue fluid leakage (swelling)
Increased nerve activity (pain)
Inflammation
1.
2.
3.
What happens when the macrophages find an invader?
Phagocytosis
Call for back-up
Increased blood flow to area (redness)
Increased tissue fluid leakage (swelling)
Increased nerve activity (pain)
Produce alarm signals (cytokines)
Alert other macrophages to come and help
Alert other cells to come and help (neutrophils)
1.
2.
3.
What happens when the macrophages find an invader?
Phagocytosis
Call for back-up
Increased blood flow to area (redness)
Increased tissue fluid leakage (swelling)
Increased nerve activity (pain)
Cytokine production
Alerts other macrophages to come and help
Alerts other cells to come and help (neutrophils)
All this adds up to…
THE ACUTE INFLAMMATORY RESPONSE
(This explains the redness, swelling and pain that we felt around that splinter)
Macrophages are really useful…
Macrophages act as lookouts
They are the first to encounter the enemy
They send out signals to recruit more defenders
They hold off the invaders until back-up arrives
This battle is usually over in a few days
Innate immunity acts to LIMIT infection
The adaptive immune system
The third level of defence
Edward Jenner - small pox vaccine
1790s - small pox major health problem
Milkmaids often got cowpox
Cowpox symptoms are like small pox
Milkmaids didn’t get small pox
So Edward Jenner injected cow pox pus into a boy o (vacca - vaccine)
Then Jenner infected the boy with small pox…
The boy didn’t get small pox!
His adaptive immune response protected him
But he was only protected against the pox virus - adaptive immunity is SPECIFIC to the invader
Antibodies
Antibodies are the molecules of adaptive immunity
- Identified as proteins in the blood of immune people
Antigen binding regions (Fab)
Light chain
IgG - prototypic antibody molecule
IgG is the most common antibody
In people, there are also IgM, IgA,
IgE and IgD
All have specialised functions and distributions
Heavy chain
Effector function region (Fc)
What do antibodies do?
Antibodies are multi-functional molecules:
Agglutinate invaders
Precipitate invaders
Neutralise invaders
Eliminate infected cells
Opsonise invaders (tagged for destruction)
In bacterial invasion- antibody Fab regions bind to the invaders and antibody Fc regions bind macrophages - antibodies act as bridges
Hungry macrophage
FcR
Antibody
Bacterium
Where do antibodies come from?
B lymphocytes (or B cells)
Made in the bone marrow
(haematopoiesis)
Educated in the bone marrow
(tolerance or self-recognition)
Set free to find their antigen and once they have found it, they will be activated (clonal selection), they’ll differentiate into
plasma cells and concentrate on making soluble antibodies
Remember: one plasma cell makes one specificity of antibody
The other lymphocytes (T cells)
Look like B cells
Have cell surface receptors (TCR) that look like antibodies
TCR production is similar to antibody production (modular design)
T cells also undergo clonal selection
TCR binds specific antigen
T cell selected as special
Proliferation: builds up a clone of identical T cells
Slow, specific response
3 kinds of T cell (for now):
Killer , T
C cells search and destroy infected cells
Helper , T
H cells produce signals to instigate and maintain an appropriate adaptive immune response
Regulatory , Treg cells put the brakes on once the danger is past prevent self-reactivity
Antigen presentation to T cells
T cells need help to recognise antigens
T cells cannot “see” native, soluble, intact proteins
Special proteins (MHC) present antigens to T cells
(Major histocompatibility complex)
Two types of MHC: Class I and Class II
Class I MHC – expressed on every cell
o Only seen by Killer T cells o Tell the Killer T cells what’s going on inside the cell
Class II MHC – expressed by specialised cells – the antigen presenting cells (APC) o Only seen by the Helper T cells
Activation of adaptive immunity
B cells and T cells need to regulated, so they must be activated before they can function
For many aspects of adaptive immunity, a two signal system is adopted
For T cells, these 2 signals are:
1. antigen-specific : T cell recognises antigen presented in MHC class II on APC
2. non-specific : protein on APC binds receptor on T cell
Like opening a safe deposit box with two keys
Both signals are the keys for activation
Either key alone - no joy
Both keys together - ACTIVATION
Secondary lymphoid organs
For adaptive immunity to be activated, the T cell specific for the invader needs to see the APC that has previously encountered the same invader… unlikely over the whole body area
Secondary lymphoid organs make these encounters more likely
The lymphatic system
Mammals have two plumbing systems:
Cardiovascular system o pressurised o pumps blood round the body
Lymphatic system o not pressurised o drains tissue fluid that leaks out of capillaries
Lymph collects in lymphatic vessels and is transported back to the blood, via the lymph nodes
Lymph collects proteins, cells etc from the tissue on its route
The lymphatic system
Invaders (bacteria, viruses) get carried to lymph nodes in the lymph
APC travel through lymph nodes
T cells and B cells circulate via lymph nodes
Lymph nodes are the place to be!
Increases the probability that the lymphocyte will encounter antigen/APC and be activated
Immunological memory
B cells and T cells are activated, proliferate, get rid of the invaders and then most will die
This stops our system being filled up with old T cells and B cells once the infection is cleared
BUT… some of these ‘experienced’ T cells and B cells will hang around in case we are infected a second time
Memory cells are key to adaptive immunity o They are easier to activate than ‘naïve’ cells o There are more of them than the naïve cells o They provide more effective protection to subsequent infections
Tolerance to ‘self’
Adaptive immunity is RANDOM
BCR (antibodies) and TCR are randomly generated by modular design
So there is a chance that the BCR and TCR might NOT recognise an invader
This can become problematic if the BCR/TCR do recognise host or self - autoimmune diseases may result
This risk is minimised because B cells and T cells are ‘taught’ to tolerate self
Not yet fully understood how this happens
But autoimmune diseases are pretty rare
Why do we need both innate and adaptive immune systems?
Innate - fast, effective but not specific
Adaptive - slower but tailored to fit
Innate immune system informs the adaptive immune system
Innate immunity integrates the response -
It tells either B cells or T cells to react depending on the invader and where they should go to find the invader
Today’s lecture in a nutshell
3 lines of defence- physical barriers, innate immunity, adaptive immunity
Macrophages are the cells of innate immunity
T and B cells are the cells of adaptive immunity
Antibodies, made by B cells, are the molecules of adaptive immunity
T cells need the help of MHC to “see” antigen
Cell encounters occur in specialised lymphoid tissue
Lymph percolates through the tissues, collecting cells and antigens
Adaptive immunity has specific memory to protect us against subsequent infections
Mistakes can be made in immune responses- these are rare but devastating