Immunity to Infection
advertisement
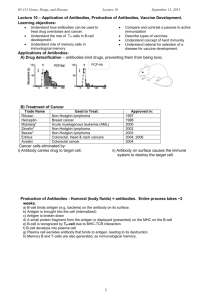
• Immunity is the acquired ability to defend against infection by disease-causing organisms. • The adaptive immune system is responsible for immunity. How B-cells work… Pathogen (e.g. bacteria, virus) Macrophage B-cells Each recognise a different antigen. The correct one develops into… Macrophage Phagocytoses pathogen and displays antigens on surface Plasma cells Clones of the correct B-cell, which produce antibodies 1st meeting a pathogen, this process takes 10-14 days Memory B cell= subesquent meetings, takes about 5 days Abnormal cell e.g cancer cell, infected cell Killer T-cell recognises antigen How T-cells work… X Antigen Clones of killer T-cell attach to antigen Normal cell X Killer T-cells release perforin pores X Helper T-cell stimulates correct killer T-cell to multiply Helper T-cell also stimulates B-cells to make antibodies Suppressor T-cells turn off immune response Abnormal cell gains water, swells and bursts Memory Tcells stay in circulation Active immunity Passive immunity Naturally acquired Naturally acquired Artificially acquired Artificially acquired • Natural immunity is the result of a body’s previous encounter with an organism. • Artificial immunity results from the injection of a vaccine or an antibody. Vaccines stimulate active immunity whereas injection antibody or antiserum is an example of passive immunity. • Active immunity is when the immune system encounters and antigen and is primed to recognise it and destroy it quickly the next time it is encountered. This is active immunity because the body’s immune system prepares itself for future challenges. • Passive immunity is short-term and involves the transfer of immunity from one individual to another via antibody-rich serum. This may be artificial as is the case with anti-venom or natural, as in antibodies crossing the placenta to protect the developing foetus. Induced Immunity Active immunity Production of a person’s own antibodies. Long lasting Natural Active Artificial Active When pathogen Vaccination – usually enters body in the contains a safe antigen normal way, we from the pathogen. make antibodies Person makes antibodies without becoming ill Edward Jenner Passive immunity An individual is given antibodies by another Short-term resistance (weeks- 6months) Natural Passive Baby in utero (placenta) Breast-fed babies Artificial Passive Gamma globulin injection Extremely fast, but short lived (e.g. snake venom) • The word vaccination comes from vacca, which is Latin for cow. • Edward Jenner could be considered the “father of vaccination” as he developed a method of protecting people from smallpox. • He noticed that milkmaids who had previously been infected with cowpox (similar disease but milder) did not catch smallpox. • In 1796, Jenner deliberately infected a small boy with material from a cowpox pustule, then six weeks later infected the boy with material from a smallpox pustule. The boy survived! • Our current understanding of pathogens indicates that Jenner got lucky – not all dangerous diseases have a less pathogenic equivalent as was the case with smallpox and cowpox. • There are four main types of vaccinations: • Live attenuated vaccines • Killed vaccines • Toxoid vaccines • Component vaccines • Many vaccines contain adjuvants. This is a general term given to any substance that when mixed with an injected immunogen will increase the immune response. Examples of adjuvants include aluminium hydroxide and aluminium phosphate. • Contain bacteria or viruses that have been altered so they can't cause disease. • Usually created from the naturally occurring germ itself. The germs used in these vaccines still can infect people, but they rarely cause serious disease. • Viruses are weakened (or attenuated) by growing them over and over again in a laboratory under nourishing conditions called cell culture. The process of growing a virus repeatedly-also known as passing--serves to lessen the disease-causing ability of the virus. Vaccines are made from viruses whose disease-causing ability has deteriorated from multiple passages. • Examples of live attenuated vaccines include: • Measles vaccine (as found in the MMR vaccine) • Mumps vaccine (MMR vaccine) • Rubella (German measles) vaccine ( MMR vaccine) • Oral polio vaccine (OPV) • Varicella (chickenpox) vaccine • Contain killed bacteria or inactivated viruses. • Inactivated (killed) vaccines cannot cause an infection, but they still can stimulate a protective immune response. Viruses are inactivated with chemicals such as formaldehyde. • Examples of inactivated (killed) vaccines: • Inactivated polio vaccine (IPV), which is the injected form of the polio vaccine • Inactivated influenza vaccine • Contain toxins (or poisons) produced by the germ that have been made harmless. • Toxoid vaccines are made by treating toxins (or poisons) produced by germs with heat or chemicals, such as formalin, to destroy their ability to cause illness. Even though toxoids do not cause disease, they stimulate the body to produce protective immunity just like the germs' natural toxins. • Examples of toxoid vaccines: • Diphtheria toxoid vaccine (may be given alone or as one of the components in the DTP, DTaP, or dT vaccines) • Tetanus toxoid vaccine (may be given alone or as part of DTP, DTaP, or dT) • Contain parts of the whole bacteria or viruses. • These vaccines cannot cause disease as they contain only parts of the viruses or bacteria, but they can stimulate the body to produce an immune response that protects against infection with the whole germ. • Component vaccines have become more common with the advent of gene technology, as the antigenic proteins can be identified and cloned then expressed in a laboratory to provide material for vaccination. • Examples of component vaccines: • • • • Haemophilus influenzae type b (Hib) vaccine Hepatitis B (Hep B) vaccine Hepatitis A (Hep A) vaccine Pneumoccocal conjugate vaccine • Pathogens that infect the human body have evolved a number of different techniques for avoiding the immune response. • These include: • Antigenic variation • Antigenic mimicry • Evading macrophage digestion • Hiding in cells • Immune suppression • Disarming antibodies • Antigenic variation • Some species of protozoan parasites evade immune response by shedding their antigens upon entering the host. • Others (e.g. trypanosomes and malarial parasites) can change the surface antigens that they express so that the specific immune system needs to make a new antibody to respond to the infection. This is known as antigenic variation. • Antigenic mimicry • This involves alteration of the pathogen’s surface so that the immune system does not recognise the pathogen as “non-self”. • Blood flukes can hijack blood group antigens from host red blood cells and incorporate them onto their outer surface so that the immune system does not respond to the infection. • Evading macrophage digestion • Macrophages have an important role in the immune system as they phagocytosis and destroy foreign material. Some microbes (e.g. Leishmania) are able to avoid enzymatic breakdown by lysosomes and can remain and grow inside the macrophage – this means they are able to avoid the immune system. • Some bacteria can avoid phagocytosis by releasing an enzyme that destroys the component of complement that attracts phagocytes. • Other bacteria can kill phagocytes by releasing a membrane-damaging toxin • Hiding in cells • Bacteria such as heliobacter can invade the epithelial lining of the intestine to multiply and divide, then transfer into neighbouring cells without entering the extracellular space where they would be vulnerable to detection. • Immune suppression • Most parasites are able to disrupt the immune system of their host to some extent. • HIV is an example of this. It selectively destroys T helper cells, therefore disabling the host immune system. • Disarming antibodies • Bacteria such as Staphylococcus aureus have receptors on their surface that disrupt the normal function of the host’s antibodies. • These receptors bind to the constant region (the stem) rather than the normal antigen binding sites. This prevents normal signalling between antibodies and other parts of the immune system such as complement activation or initiating phagocytosis of a bound antigen. Invader antigens are everywhere! What does it need to get by? Skin! neutrophils Monoctyes (macrophages) Invader dies! T - Helper lymphs B lymphs Plasma B cells Memory B cells Antibodies!! Invader dies!! More T - Helper lymphs! Cytotoxic T lymphs Invader dies!!